CHAPTER 41 Management of Atrial Fibrillation
Atrial fibrillation (AF) is the most important cardiac rhythm disorder affecting performance in horses. The prevalence is about 0.5%, and there is no known sex or age predilection. AF is an atrial tachyarrhythmia that is frequently found in the absence of other cardiac pathology, especially in large breeds. In ponies, AF is encountered only as a result of severe cardiac disease.
CLINICAL PRESENTATION
Most frequently and in contrast to other species, however, horses (but not ponies) develop AF without underlying cardiac disease or with only minor underlying disease. This condition is called lone or primary AF. Treatment of horses with this form of AF is rewarding because of the good success rate for cardioversion and lower rate of recurrence.
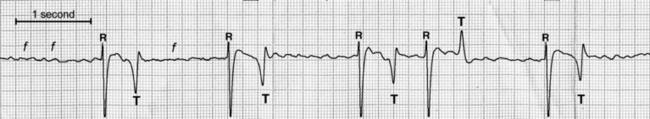
Diagnosis of AF should be confirmed by means of an electrocardiogram (ECG), which will be characterized by normal QRS morphology and irregular R-R intervals, coarse undulations of the isoelectric line (f waves), and absence of P waves (Figure 41-1). Because of aberrant conduction, a shortly coupled QRS complex might have a different T-wave morphology, which should not be mistaken for a ventricular premature beat. The presence of ventricular premature beats suggests an electrolyte disorder or diffuse myocardial disease and warrants further investigation.