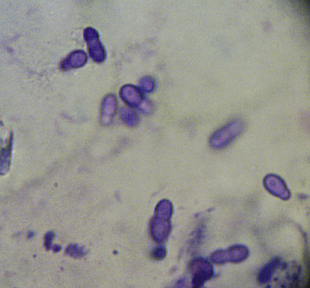
Chapter 59 Malassezia spp. (formerly Pityrosporum spp.) are lipophilic yeasts that normally colonize animal and human skin in low numbers. At least 13 species of Malassezia exist. The vast majority of species are classified as lipid dependent: when grown in the laboratory, these species have an absolute requirement for long-chain fatty acids, which are used as a source of carbon. In contrast, Malassezia pachydermatis, the most commonly isolated yeast species from the skin and ears of healthy dogs and cats, is non–lipid dependent when grown in the laboratory. Lipid-dependent species, including Malassezia globosa, Malassezia sympodialis, Malassezia nana, Malassezia slooffiae, and Malassezia furfur, can colonize the skin of healthy cats.2–5 Malassezia spp. are common opportunistic contributors to chronic dermatitis and otitis externa in dogs, and to a lesser extent in cats. They are isolated more frequently from the ears of dogs and cats with otitis externa than from the ears of healthy dogs and cats.6,7 Dogs with skin disease can have 100- to 10,000-fold increases in skin population densities of Malassezia spp. compared with healthy dogs.8 Species and strains of Malassezia vary in virulence and tropism for different anatomic sites and host species.9,10 A variety of lipid-dependent Malassezia spp. occasionally have been isolated from dogs and cats with otitis externa.6,7,11–14 Malassezia spp. infection can occur in dogs and cats of any age, breed, and sex, but some dog breeds are thought to be predisposed, including American cocker spaniels, West Highland white terriers, basset hounds, poodles, and Australian silky terriers.15 Sphynx and Devon Rex cats have high rates of Malassezia spp. colonization when compared with domestic shorthair cats.16 Malassezia spp. proliferate opportunistically, becoming pathogenic with alterations in host defenses or the skin surface microclimate. Examples of underlying diseases include allergic dermatitis, endocrinopathies, intertrigo, primary keratinization/cornification disorders, and, in cats, underlying neoplasia or retrovirus infections.17,18 A history of treatment with antibiotics was a predisposing factor in one study.19 Prolonged glucocorticoid treatment can also lead to yeast proliferation. The yeasts adhere to the cells of the stratum corneum and secrete lipases, proteinases, phospholipases, and acid sphingomyelinases.20 The resulting skin lesions may be localized or generalized, are thought to result from inflammation, and, in some animals, hypersensitivity reactions to yeast antigens.21,22 The more erythematous the interdigital region is in an atopic dog, the more likely a Malassezia spp. infection is present.23 The most commonly affected anatomic sites are the ear canals, skin folds (including the periocular and perioral skin, ventral neck, axillae, inguinal regions, and perineum), and interdigital skin (Figure 59-1). Clinical signs include erythema, pruritus, alopecia, scaling, and a greasy exudate. The claw beds may develop a reddish-brown stain. Chronicity results in hyperpigmentation, lichenification, and stenosis of the ear canal, and a pungent, offensive odor develops. Pruritus may result in excoriations. Devon Rex and Sphynx cats can develop a greasy dermatitis associated with increased numbers of Malassezia spp., which can respond dramatically to antifungal drug treatment.8 FIGURE 59-1 Five-year-old male neutered pug with a 1 year history of otitis externa and generalized pruritus. Malassezia dermatitis and bacterial pyoderma secondary to underlying atopic dermatitis was diagnosed. Note the distribution of lesions, which affect the facial folds and ventral neck (A) and axillae (B). A thorough physical and dermatologic examination aids diagnosis of Malassezia spp. infection and provides important clues as to the underlying disorder leading to opportunistic proliferation of Malassezia spp. It also allows identification of lesions consistent with concurrent pyoderma (see Chapter 84). Cytology is an important tool for diagnosis and is generally performed using clear (not frosted) acetate (Scotch) tape preparations of the skin. The tape is pressed to the skin, dipped in the final step basophilic (blue) Diff-Quik solution, rinsed, and applied to a slide on which a drop of immersion oil has been placed. Alternatively, the tape is pressed against the affected skin several times and then placed on a dry glass slide, and a small amount of the basophilic Diff-Quik solution is injected under the tape. The tape is then examined using a light microscope, with an additional drop of immersion oil to allow identification of bacteria and Malassezia spp. using the 100˜ objective. The yeasts stain deeply basophilic and exhibit wide-based budding, resembling “footprints,” “peanuts,” or “snowmen” (Figure 59-2). An inflammatory cellular response is often not present, even when Malassezia spp. contribute to disease progression. FIGURE 59-2 Tape preparation from the skin of a dog with Malassezia dermatitis. Note broad-based budding yeasts, which have the appearance of a footprint. Modified Wright’s stain, 1000× oil magnification.
Malassezia Infections
Etiology and Epidemiology
Clinical Features

Physical Examination
Diagnosis
Microbiologic Testing
Cytologic Examination
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Malassezia Infections
Only gold members can continue reading. Log In or Register to continue
