CHAPTER 130 Making a Neuroanatomic Diagnosis
Establishment of a neurologic diagnosis requires thorough and orderly completion of several procedures, beginning with obtaining a history and performing physical and neurologic examinations. The signalment, environment, and function of the horse, as well as the husbandry practices of the owner, can provide tremendous insight into predisposing disease factors.
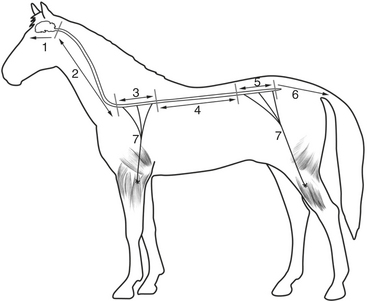
The three major regions of the nervous system are often further subdivided into more discrete neuroanatomic areas (Figure 130-1). Disease in each of these areas commonly manifests with a set of cardinal clinical signs that distinguish lesions in these regions and are reflective of dysfunction of the neurologic structures residing in each area. Individual animals may have one or more clinical signs referable to the affected region. The remainder of this chapter reviews the clinical features of disease affecting each of the regions of the neuraxis in horses.
DEFINITION OF THE DISCRETE COMPONENTS OF THE INTRACRANIAL REGION
Clinical Signs of Telencephalic Disease
Diseases of the telencephalon often result in unusual behaviors such as aggressiveness, head pressing, and aimless wandering, signs that are readily noticed and frequently form the primary complaint of horse owners. Telencephalic lesions may also cause various degrees of altered mentation ranging from delirium to coma. Other clinical signs of telencephalic disease include seizures, circling, head turns, and blindness. Horses with telencephalic lesions that circle do so toward the side of the lesion, and any associated head turn is also toward the side of the lesion. A head turn is characterized by lateral deviation of the head and neck from the sagittal plane without concurrent rotation about the poll. Blindness associated with a unilateral lesion of the occipital cerebral cortex, which contains the visual cortex, will cause a menace deficit contralateral to the lesion and will be associated with normal pupillary light reflexes. Although proprioceptive and postural reaction deficits can be detected in the limbs of horses with telencephalic lesions, they are often subtle and more pronounced in the limbs contralateral to the lesion and typically do not cause significant gait abnormalities. Deficits in olfaction (cranial nerve I or olfactory rhinencephalon) can also be present, although clinical detection of such an abnormality can be difficult in the absence of other signs. Relatively little cerebrocortical integrative function is needed to complete activities required for daily existence. Thus, telencephalic lesions can be clinically occult.