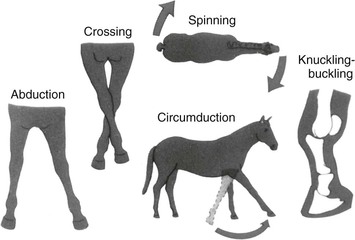
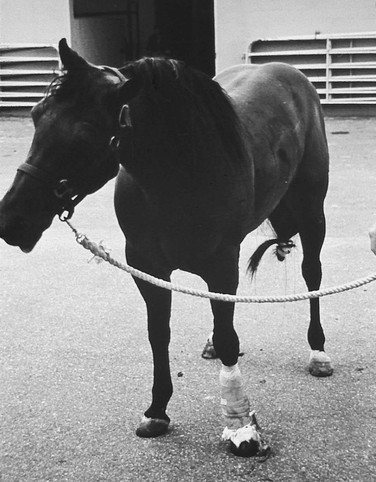
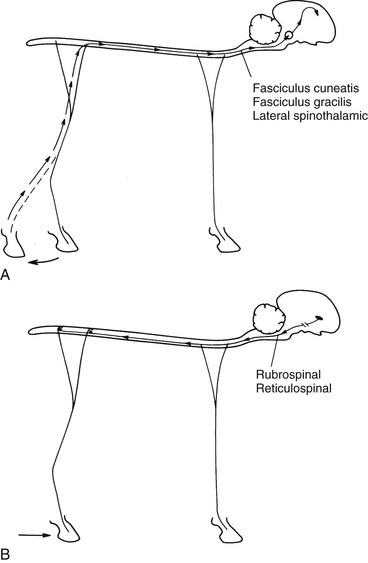
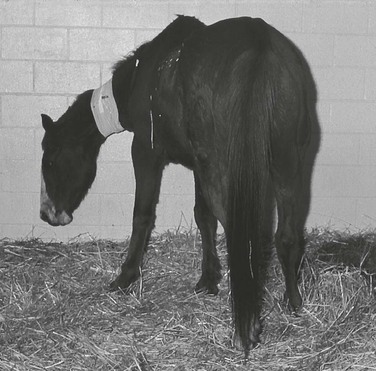
David C. Van Metre, Robert J. MacKay *, Consulting Editors The clinical signs of neurologic disease depend on the location of the disease process within the nervous system (Table 8-1). Widely varying disease entities may produce similar or identical clinical signs. Seizures, for example, may be the result of metabolic, toxic, traumatic, neoplastic, or other causes. Definitive diagnosis of neurologic disease, therefore, cannot be made on the basis of clinical signs alone. Localization of lesions within the nervous system by meticulous physical and neurologic examination is the first and key step in developing a differential diagnosis list and a rational diagnostic and therapeutic plan. TABLE 8-1 Localization of Central Nervous System Lesions According to Major Signs Encountered ARAS, Ascending reticular activating system; LMN, lower motor neuron; UMN, upper motor neuron. The species, breed, age, and pedigree of an animal are important considerations in the differential diagnosis of neurologic disease. Many diseases are species specific, particularly in the case of infectious and genetic diseases. Some diseases are not only species specific but also have higher incidence in certain breeds of that species. An example of this is juvenile idiopathic epilepsy, which has been observed in several breeds of horses but has its highest incidence in Arabian foals.1 Examples of the numerous other breed-related neurologic diseases of large animals are cerebellar abiotrophy (Arabian foals), progressive ataxia (Charolais), demyelinating myelopathy (Limousins), neuraxial edema (polled Herefords), and many others.2–10 Atlantoaxial malformations most commonly occur in Arabian foals and Holstein calves but can occur in other breeds.11,12 Disease susceptibility also may be linked to age. Acute lead poisoning, for example, occurs most commonly in calves, whereas adult cattle tend to develop the subacute form of the disease.13 Some diseases are found in the neonate at birth. A large number of congenital disorders of the central nervous system (CNS) can affect domestic livestock. These diseases have a variable clinical course, depending on the nature of the disorder. Congenital disorders of myelin metabolism worsen with age, whereas other developmental conditions may remain stable throughout the animal’s life.14–19 Examples of these disorders that have genetic tests available are listed in Chapter 52. Many disorders of the CNS produce characteristic patterns of onset and progression. Some CNS diseases occur acutely, developing the full range of clinical signs within hours. If the disease is not fatal, the signs either stabilize by 24 hours and remain constant thereafter or improve. Diseases that may display this clinical course include traumatic injuries and some types of toxic, infectious, and metabolic diseases. Diseases with degenerative, neoplastic, and certain viral causes may develop more slowly, requiring days to weeks for development of characteristic clinical signs.2,20,21 The diet of patients with neurologic disease should be evaluated20–25 (Table 8-2). Equine motor neuron disease is seen mainly in horses that are housed without access to pasture and whose diet is deficient in vitamin E.26 Copper deficiency occurs in ruminants pastured in areas with shale or volcanic soils, which are either deficient in copper or contain high concentrations of molybdenum and sulfur; demyelination of the spinal cord in newborn small ruminants may result, as can vertebral fractures in calves. Dietary deficiency of calcium in rapidly growing weaned calves also results in vertebral and long bone fractures. Overfeeding of protein and energy, as well as imbalance of certain trace minerals, has been linked to cervical vertebral stenotic myelopathy in horses (wobbler).27,28 TABLE 8-2 Dietary Deficiencies Associated with Neurologic Disorders of Livestock Examination of the patient’s environment may provide valuable information about the cause of CNS disease. Outbreaks of botulism and listeriosis have been associated with ingestion of rotting vegetation around haystacks, silos, and feed bunks.29,30 Plant poisonings are common in livestock, and identification of neurotoxic plants is important whenever multiple animals are affected simultaneously30–32 (Table 8-3). Nonplant neurotoxicants of livestock include lead, ethylene glycol, organic mercurials, chlorinated hydrocarbons, organophosphates, salt, sulfur, petroleum distillates, and many others. Dose of the neurotoxicant may be important, with different clinical signs appearing depending on the level of exposure. For example, ingestion of high concentrations of organophosphates or carbamates produces marked ataxia, coma, muscle tremors, salivation, and miotic pupils. When low doses of organophosphates are ingested chronically, however, the result is an axonopathy of spinal cord and medullary neurons, resulting in pelvic limb paresis and ataxia, which may progress to tetraparesis and recumbency.33 Therapeutic and dietary interventions also may result in toxicoses when improperly administered. Overdosing of cattle with propylene glycol produces profound ataxia, depression, and coma.34 Ingestion of urea or ammoniated feedstuff produces hyperesthesia, excitability, coma, and convulsions. High concentrations of salt in drinking water or, more commonly, lack of fresh water or interruption of the water supply followed by unlimited access to water can result in laminar necrosis of the cerebral cortex or eosinophilic meningitis.33 The clinical signs are those of forebrain dysfunction, including blindness, dullness, seizures, coma, and death.35–37 Geographic area also may be important in the differential diagnosis of neurologic disease. Certain infectious diseases may be more common in particular areas of the country or even regions within a single state where the conditions for disease vectors are optimal.38 The travel history of the animal must be considered, as well as the animal’s location at the time clinical signs appeared. Travel also may result in increased contact with other animals and greater risk of exposure to infectious diseases. Intermingling of horses from different premises is a potential risk for equine herpesvirus-1 myeloencephalopathy (EHM).39 TABLE 8-3 Selected Poisonous Plants Producing Neurologic Signs (also see Chapter 54) When a neurologic problem is evaluated, the vaccination history and previous herd or individual disease problems should be noted. Some vaccines are highly protective, such as those for rabies and tetanus. Neurologic disease may be a secondary complication of disease in another organ system. Foals and calves with severe diarrhea, for example, may convulse secondary to hypokalemia, hypernatremia, hyponatremia, or hypoglycemia. Preexisting diseases in the population should be determined. For example, outbreaks of EHM are sometimes preceded by respiratory disease or abortions in herdmates.39 Thromboembolic meningoencephalitis of cattle often follows an outbreak of respiratory disease within the herd. Historical evidence of limited colostral intake may be important in the diagnosis of bacterial meningitis of neonates. Bloody diarrhea often precedes the onset of nervous coccidiosis of calves.40 Hypomagnesemia, eclampsia (hypocalcemia), hypokalemia, hypophosphatemia, and nervous ketosis are common causes of recumbency, convulsions, and tremors in adult livestock. These diseases usually occur between the beginning of the last trimester and the first 2 months after parturition. A thorough physical examination should always precede or be performed concurrently with the neurologic examination. In some instances disease of organ systems other than the nervous system may take precedence for diagnosis and treatment. Such may be the case with animals in shock or suffering from other life-threatening cardiovascular or respiratory disturbances. The neurologic examination should be carried out in a systematic fashion. The exact order of the examination is not important in itself, but procedures that may cause discomfort or pain such as palpation of the spine should be left until last. A common system used by many neurologists is to start at the head and progress to the tail.41 Some clinicians prefer to examine the animal standing in the stall initially and then observe the gait. Because large animals are less amenable to handling than the typical cat or dog, another system for the neurologic examination is to begin with procedures that require minimal handling of the animal, such as observation of mental status, posture, and gait, and proceed to those that require greater manipulation: examination of the cranial nerves, assessment of spinal reflexes, and so on. Neurologic examination alone rarely leads to definitive diagnosis but rather helps to answer the questions “Does the animal have neurologic disease?” and “What is the location of the neurologic lesion?” Once these questions are answered, a list of differential diagnoses can be made in light of other information such as the signalment of the animal and the history of the current problem. The diagnostic plan is based on the location of the lesion and the most likely differential diagnoses. Initial examination should be done from a distance. The examiner observes the animal’s mental state and whether its responses to its surroundings are appropriate. This is done ideally in the animal’s usual environment, where it would be expected to be calmest. When this is not possible, the influence of factors such as the stress and excitement of previous travel and the animal’s natural fear of unfamiliar surroundings, sounds, and smells must be taken into account. The reports from the animal’s usual handler may be informative, if he or she is a good observer and has an understanding of normal behavior in animals. Compare the patient’s interaction with its environment to a summary of its previous behavior and to the activities of the herdmates. All livestock should recognize and fear strangers and should show awareness of the examiner’s position. Normal animals change the posture of the head, ears, and eyes as the examiner moves. Depending on previous conditioning, normal behavior may include cautionary moves, avoidance, belligerence, or affection. Animals with decreased mental alertness (obtunded, dull, depressed) have reduced responses to examination, lassitude, lack of recognition, unwillingness to rise or lift the head from the ground, lack of appetite, drooped ears, stupor, or coma (Fig. 8-1). Systemic illness also may cause dull mentation; thorough physical examination and, perhaps, diagnostic tests including a complete blood count and serum chemistry are important in determining whether systemic disease is present. Changes in behavior are consequences of diseases affecting the forebrain: the cerebrum or the relay areas of the diencephalon. Abnormal behavior caused by forebrain dysfunction can be termed dementia. Some common examples of dementia include head-pressing, compulsive walking (often around the inside of an enclosure), frequent yawning, loss or absence of innate behaviors such as udder seeking by neonates and mutual affinity of dams and offspring, and loss of learned behaviors such as the ability to be led by a lead rope and halter. Hyperexcitability, rage, mania, exaggerated fear, or frantic motor activities are suggestive of a lesion of the limbic system of the forebrain, an assembly of interconnected neurons in the brain that is involved in emotional responses and patterns of behavior. Animals so affected may strike or kick at inappropriate times, demolish their stalls, bellow, show belligerence, or, if recumbent, struggle violently. The age, species, previous management system, and even the breed of animal are important considerations in the assessment of behavior. Bulls and stallions exhibit behavior that is very different from that of steers and geldings. Beef cattle behave differently than dairy cattle do. Animals that are handled regularly show fewer and milder fearful or aggressive responses than do animals that are handled rarely. The source of mental alertness is the ascending reticular activating system (ARAS) of the brainstem, which repetitively signals the forebrain to maintain consciousness. For this purpose, the ARAS integrates inputs to the brain of all sensory modalities. The portion of the ARAS within the midbrain is functionally the most important with progressively less input caudally and rostrally in the brainstem. The ARAS is important in maintaining the animal’s level of consciousness and arousal. The relationship between the cerebral cortex and the ARAS is sometimes described as follows: The cerebral cortex determines the content of consciousness, and the ARAS determines the level of consciousness. Diseases affecting the ARAS tend to produce profound depression of consciousness, particularly if the midbrain segment of this system is affected. In this case, other signs of midbrain disease such as pupillary dilation and loss of the oculocephalic reflexes (see later) are often observed. The forebrain is the “seat of consciousness”: Conscious perception of both external stimuli (e.g., vision, hearing, touch) and internal stimuli (e.g., abdominal pain) depends on its integrity. In general, level of consciousness is not substantially altered by forebrain diseases unless the injury is diffuse and severe. A seizure (convulsion, ictus) is a manifestation of forebrain dysfunction characterized by involuntary somatic and autonomic motor activities and/or loss of consciousness. Seizures may be generalized or focal (partial). Generalized seizures are characterized by recumbency, loss of consciousness, flailing or galloping motions of the limbs, elimination of feces and urine, and nystagmus. Localized involuntary movements with or without obvious alterations of consciousness characterize focal seizures. Alternatively, focal seizures may result in episodes of abnormal or bizarre behavior or momentary lapses of consciousness without collapse or significant motor activity. A third form of seizure is focal with secondary generalization. The onset of the seizure is focal within the forebrain, but seizure activity subsequently spreads throughout the brain, resulting in a generalized seizure. Animals with this form of seizure activity exhibit initial focal signs such as head turning, bellowing, and focal tremors followed by loss of consciousness and generalized signs of involuntary motor activity, as described previously. Rarely, seizures in large animals may be preceded by an aura, a period in which the animal exhibits anxiety or restless behavior shortly before the onset of the seizure itself. A postictal phase, a period of time subsequent to the seizure during which the animal is obtunded or, occasionally, restless and anxious, is usual after seizures in most animals. The postictal phase usually lasts a few minutes to hours but may last as long as several days. The postictal phase may be the only stage of the seizure observed by the animal’s handler. Thus seizures should be considered as a possible cause in any animal with a history of episodes of abnormal behavior. The typical history is that the animal is found in a dull or excited state, without the handler observing the onset of this change of behavior. Additional signs of postictal forebrain dysfunction may include blindness, absent menace responses, and insensitivity to cutaneous noxious stimulation. Additional supporting evidence includes physical injuries such as scrapes and cuts that may have been incurred during the seizure. Abnormalities of forebrain dysfunction are the ultimate cause of seizure activity. During a seizure, neurons in the cerebral cortex exhibit spontaneous electrical activity, beginning either focally or simultaneously throughout the cortex, resulting in the clinical manifestations of focal or generalized seizures. Causes of seizures are legion, including alterations in the neuronal environment resulting from metabolic disturbances or toxicities and the effects of structural brain diseases such as congenital or developmental disorders, traumatic injuries, neoplasia, and inflammatory conditions. Diagnosis of seizures and other states of altered mentation must include a thorough physical examination and screening for metabolic diseases such as electrolyte imbalances and hepatic or renal failure. Abnormalities in the neurologic examination found between seizures (interictal period) support a diagnosis of primary brain disease and are an indication for diagnostic procedures such as cerebrospinal fluid (CSF) tap. Some toxins cause additional systemic signs such as neuromuscular involvement (tremors, weakness) or parenchymal organ failure (icterus, uremia). Such signs, combined with clinical history and inspection of the environment, will help to direct specific tests for toxins. Narcolepsy is a condition reported in cattle and horses wherein the normal mechanisms of sleep are disturbed.42–45 Although sudden onset of sleep is one manifestation of narcolepsy, the acute onset of cataplexy—complete paralysis of striated muscles—is usually a more prominent clinical feature. Animals may be observed to suddenly collapse to the ground or to buckle at the knees. Cardiac and respiratory muscles are not affected. Narcoleptic attacks may be difficult to distinguish from seizures but are not accompanied by the involuntary motor activity that characterizes most generalized seizures. In some cases, traumatic injuries to the head, face, and limbs can result. Gait should be evaluated by moving the animal in a straight line, moving it in a tight circle, backing up, and moving it over obstacles such as a curb. Having the patient walk up and down a slope with varying steepness and with the head elevated may reveal subtler abnormalities. The examination may need to be modified depending on the species of the patient, amenability to handling, and consideration of safety concerns. Quadrupeds begin walking by protracting the pelvic limb, followed by the thoracic limb of the same side, then the opposite pelvic limb, and finally the opposite thoracic limb. Gait on a level surface requires integrity of the musculature, motor and sensory components of the peripheral nerves, local spinal reflexes, ascending and descending pathways in the spinal cord, and centers within the brainstem. Dysfunction of ascending pathways (spinocerebellar tracts) results in mild to severe proprioceptive disturbances when standing or walking, which are exacerbated by turning the animal in a circle or stepping it on and off a curb. Animals with cerebral disease are usually able to perform simple motor activities such as walking along a straight path without obvious deficits but may exhibit decreased proprioception when they are required to perform complex motor activities such as walking on slopes or negotiating obstacles such as curbs or ground poles. Subtle gait deficits may be elicited by walking and then trotting the patient, or walking or trotting the patient briskly and then stopping suddenly. While a helper is walking the animal in a straight line on a level surface, the examiner should take hold of the tail on the same side and pull the animal firmly to one side during the stance phase of the stride. The normal animal will move toward the pull but should not stumble or fall. If the tension on the tail is maintained, strength can be assessed. Animals with lesions anywhere within the ascending or descending pathways controlling gait may be weak and/or show decreased proprioception in the form of stumbling, tripping, or crossing the limbs. The same test can be performed in the patient at rest. Resistance to lateral pressure at rest is provided by the antigravity myotatic reflex. Because this reflex uses peripheral nerves and spinal cord segments of the lumbosacral intumescence, inability to resist the tail-pull test at rest is suggestive of lower motor neuron (spinal cord gray matter, nerve roots, or peripheral nerves) of the L3 to S2 spinal cord segments on the side being tested. Circling the patient in a wide circle and then a tight circle also may elicit deficits, such as knuckling, stumbling, interference between feet, pivoting on one foot, or wide movements in the outside limb (circumduction), that are not observed when the animal is walked in a straight line. Assessment of gait is facilitated when animals are halterbroken and can be led. This is not the case in many ruminants, so the clinician must rely more on observing the animal in its usual environment or in a confined area such as a pen. A handler may drive animals that are not halterbroken, but this should be done with due consideration of animal and handler safety. A grading system for gait deficits has been described elsewhere,46 as follows: Proprioception is the sense of body position in space. Proprioceptive information is collected by receptors in the skin, joints, muscles, and vestibular system. General proprioceptive pathways run mainly in the lateral (spinocerebellar) and dorsal (conscious perception) funiculi of the spinal cord, relaying information to centers in the brainstem, cerebellum, and cerebral cortex. The vestibular system and pathways in the spinal cord to the vestibular centers in the medulla oblongata and cerebellum also help to control proprioception. Abnormalities of proprioception include stumbling, adduction or abduction of the limbs, circumduction, and interference between limbs (Fig. 8-2). Animals with proprioceptive deficits often slap down the feet hard, rather like the gait of a person walking down stairs in the dark, unsure of where the next step is. Walking the animal off a curb or step or down a slope exaggerates this appearance. When spun in a tight circle, normal animals lift the inside forefoot as the weight shifts. The outside rear leg is put down within a line demarcated by the lateral margin of the trunk. When spun in a tight circle, patients with abnormal proprioception may pivot on the inner hindfoot rather than lifting it and replacing it into a normal position. The outside foot may circumduct widely, knuckle, or buckle, and the inside foot may step on the outside foot. Animals with abnormal proprioception worsen when they are required to climb hills or lift the foot over a curb or are walked with the head elevated. The gait of noncompliant cattle may be assessed by observation of maneuvers through corrals, alleys, or a squeeze chute. Having the animal walk backward also tests proprioception. The normal subject should be able to do so in a smooth, coordinated fashion, with conjugate movement of diagonally opposite limbs. Animals with lesions of upper motor neurons in the descending motor pathways may exhibit abnormalities such as foot dragging and weakness, sometimes to the point of “dog-sitting”; others may be reluctant to move straight backward and will try avoidance maneuvers such as circling to one side or the other in order to avoid it. Such tactics should raise the index of suspicion of a neurologic deficit. Care should be taken when backing an animal with severe neurologic deficits because some animals could fall backward during the procedure. Animals that are uncooperative or that have been little handled may exhibit reluctance to walk backward that is not caused by neurologic disease. Observing the patient’s general level of cooperation and having a behavioral history will help the examiner determine whether the problem is caused by neurologic disease or the animal’s lack of compliance. Cerebellar disease causes errors in the rate, range, and force of voluntary movements; there is generalized ataxia with a rolling, drunken gait. Protraction of the limbs is delayed and limb movements are exaggerated, characterized either by excessive flexion during protraction, a condition known as hypermetria, or by hypometria, characterized by reduced joint flexion. There are often coarse bobbing movements of the head when the patient is walking; an intention tremor (most notable in the head) occurs when the animal initiates purposeful movements, such as reaching out to take food. Intention tremors may disappear when the animal is relaxed or recumbent. Cerebellar diseases may also result in opisthotonos or seizure-like fits. Spontaneous circling is seen in diseases of the vestibular system and forebrain. Circling varies from a mild tendency to move in one direction to spinning and staggering in tight circles. Circling most often occurs toward the side of the lesion, except in paradoxic vestibular disease (caused by lesions in the vestibular components of the cerebellum) and with some asymmetric forebrain lesions, in which the animal circles away from the side of the lesion. Localization of the neurologic lesion in animals that circle is made on the basis of other neurologic abnormalities such as dementia, seizures, and central blindness (forebrain disease) or proprioceptive deficits, head tilt, spontaneous nystagmus, obtundation, and other cranial nerve deficits (vestibular disease). The integrity of conscious proprioceptive pathways may be tested by means of the postural reactions. Normal animals stand at rest with the limbs in line with the abaxial boundaries of the trunk. When the limbs are moved, normal alert animals do not permit the limbs to be placed outside of the body axis or across midline. After the examiner places the limbs in an abnormal position, the neurologically intact animal returns to a normal stance within a few seconds. Animals with conscious proprioceptive deficits allow the limb to remain in the abnormal position for longer than the usual period of time. This can vary from animals in which replacement of the limb into a normal position is slightly slowed to animals that do not try to replace the limb at all. The examiner should cross one of the animal’s limbs over the opposite limb or abduct one limb; the normal response is for the limb to be placed back into the resting position. Normal animals often strongly resist attempts to place the limbs in abnormal positions. It should be noted that normal animals are extremely variable in their responses to this maneuver, so undue reliance should not be placed on its results, particularly if there are no other signs of ataxia. Animals with proprioceptive deficits may spontaneously place the limbs in abnormal positions: excessively adducted, abducted, or even crossed. Abnormalities of proprioception alone are poorly localizing signs, although a couple of generalities may be stated. Unilateral lesions rostral to the medulla oblongata produce mild to moderate proprioceptive and postural deficits in the contralateral limbs. Unilateral lesions in the medulla oblongata or spinal cord produce more severe proprioceptive and postural deficits in the ipsilateral limbs. Lesions of the cerebellum rarely result in postural deficits. Additional postural reactions such as hopping, hemiwalking, and wheelbarrowing can be tested in small ruminants, calves, and some foals. Hopping is tested in the thoracic limbs by lifting the pelvic limbs a few inches off the ground by means of a hand and arm placed around the abdomen, flexing one thoracic limb slightly, and moving the animal away from the side of the flexed thoracic limb so that it has to hop laterally on the thoracic limb still in contact with the ground. It is easiest if the examiner stands in one place and turns clockwise when testing the animal’s right thoracic limb and counterclockwise when testing the left thoracic limb. Hopping in the pelvic limbs can be tested similarly, supporting both thoracic limbs off the ground with an arm around the chest. Hemiwalking is done by supporting both limbs on one side of the body in a slightly flexed position and pushing the animal toward the opposite side so that it must walk laterally on the two limbs still in contact with the ground. Both hopping and hemiwalking should be done with care not to push the patient over. Adult horses can be made to hop on one thoracic limb by picking up the opposite limb and firmly pushing the head and shoulders laterally. Hopping and hemiwalking involve the same ascending and descending motor tracts involved in gait on a level surface but also require input from the forebrain. These maneuvers are abnormal on the ipsilateral side in animals with lesions in the skeletal muscles, peripheral nerves, spinal cord, and medulla oblongata and on the contralateral side in animals with lesions in the midbrain or forebrain. Animals with forebrain lesions have normal gait on a level surface but subtle deficits in hemiwalking and hopping. Posture refers to the position of the body and head in space, in relationship to gravity and to each other. Animals adopt slightly different postures when on a sloped or uneven surface compared with posture on a level surface. However, sustained asymmetric postures such as head tilt (Fig. 8-3), in which one ear is closer to the ground than the other, and head turn (Fig. 8-4), in which the nose is turned back toward the trunk, are abnormal. Circling often accompanies head tilt and head turn in asymmetric vestibular disease, and all tend to be toward the direction of the lesion. The exception to this rule occurs in paradoxic vestibular syndrome, in which head tilt and circling occur in a direction away from the side of the lesion. The righting response is most easily tested in small ruminants and in recumbent large animals (Fig. 8-5). The response is initiated by receptors in the eyes and vestibular labyrinths and by proprioceptive receptors in the joints, tendons, and muscles. Information regarding limb position and balance is relayed ultimately to the cerebral cortex. Descending impulses are initiated in the motor cortex and relayed via the brainstem, cerebellum, and spinal cord to the appendicular musculature. The normal response to stimulation is to lift the head, assume sternal recumbency, and rise. The normal horse rises on the thoracic limbs first, whereas the normal ruminant rises on the pelvic limbs first. Animals that are in lateral recumbency and unable to lift the head from the ground may have lesions in the peripheral or brainstem vestibular centers or in the cervical spinal cord cranial to the C4 spinal cord segment. Unilateral lesions in this area result in an inability to lift the head from the ground when the lesion side is up. When the lesion side is down, the animal can raise the head slightly. Animals with incomplete lesions of the C7 to T2 spinal cord segments are able to lift the head and neck but cannot rotate the thorax into a prone position, and they may remain recumbent. Animals with lesions of the thoracolumbar and lumbosacral spinal cord (T3 to S3 spinal cord segments) can usually lift the head and neck, arise on the thoracic limbs, and assume a dog-sitting position.
Localization and Differentiation of Neurologic Diseases

Sign or Problem Encountered
Lesion Location
Changes in Gait and Locomotion
Ataxia
Spinocerebellar tracts, spinal cord, and brainstem; vestibular system; cerebellum
Conscious proprioceptive deficit
Fasciculus gracilis and fasciculus cuneatus and connections, spinal cord, brainstem, forebrain
Knuckling
Usually LMN, ventral horn gray matter, spinal cord; occasionally UMN, spinal cord, brainstem
Abduction or adduction
Spinocerebellar tracts, spinal cord, brainstem, cerebellum
Abnormal postural placement
Spinocerebellar tracts, spinal cord, and brainstem; gracilis and fasciculus cuneatus and connections, spinal cord and brain
Hypermetria
Cerebellum, cerebellar peduncles, spinocerebellar tracts
Circling, or falling to one side
Forebrain, vestibular nuclei and connections, cerebellum
Paraplegia
UMN, from T2 to S2, or LMN, L3 to S2
Hemiplegia
Ipsilateral brainstem or spinal cord, cranial to T3
Changes in Sensorium and Behavior
Coma or semicoma
ARAS; diffuse forebrain
Obtundation
ARAS; forebrain
Seizures
Forebrain
Head pressing, compulsive walking
Forebrain
Aggression or rage
Forebrain
Inappropriate sexuality
Forebrain
Hyperphagia or hypophagia
Hypothalamus
Diabetes insipidus
Hypothalamus
Head shaking
Unknown, probably peripheral trigeminal neuralgia
Changes in Head Posture
Stiff neck
Meninges, cervical spine
Head tilt
Vestibular nuclei and connections (medulla oblongata, cerebellum)
Head tremor
Cerebellum, basal ganglia
Opisthotonos
Cerebellum (rostral vermis), rostral brainstem, cerebrum, cranial nerve VIII
Cranial Nerve Dysfunction
Blindness
Cerebral cortex, internal capsule, optic tracts, optic chiasm, optic nerve, eye
Anisocoria
Cervical spinal cord (tectotegmentospinal tract), cranial thoracic nerve roots, vagosympathetic trunk, midbrain (oculomotor nerve nucleus), cranial cervical ganglion, ciliary ganglion, oculomotor nerve, optic nerve
Mydriasis
Oculomotor nerve, midbrain, optic nerve, eye
Miosis
Vagosympathetic trunk, ciliary ganglia, tectum, brainstem, cervical spinal cord
Ptosis
Facial nerve, vagosympathetic trunk, cranial cervical ganglion, midbrain, oculomotor nerve, cervical spinal cord (tectotegmentospinal tract)
Strabismus
Ventrolateral
Cerebellum, vestibular nucleus, oculomotor nerve
Dorsomedial
Trochlear nerve
Medial
Abducent nerve
Nystagmus
Horizontal
Nerve VIII (peripheral)
Vertical or rotatory
Vestibular nuclei, peripheral vestibular receptor, cerebellum, vestibulocochlear nerve
Jaw drop
Trigeminal motor nucleus (pons), trigeminal nerve
Flaccid tongue
Hypoglossal nucleus (medulla oblongata), hypoglossal nerve, lingual muscle
Facial paralysis
Facial nucleus (medulla oblongata), facial nerve, facial muscles
Facial analgesia
Trigeminal nerve (sensory component), pons, forebrain
Dry eye
Cranial nerve VII before exiting petrous temporal bone
Changes in Reflexes
Patellar
L3-L6 spinal cord, femoral nerve, quadriceps femoris muscle
Flexors (thoracic limbs)
C5-T2 spinal cord segments, radial, ulnar, musculocutaneous and median nerves, and innervated muscles
Flexors (pelvic limbs)
L6-S2 spinal cord segments (pelvic limbs); sciatic, peroneal, and tibial nerves; flexor muscles of the limbs
Triceps
C6-T1 spinal cord segments, radial nerve, triceps muscle
Cutaneous trunci
C8-T1 spinal cord segments, lateral thoracic nerve, white matter of thoracic spinal cord
Anal
S1-S5 sacral spinal cord segments, pudendal nerve
Cervicofacial
Dorsal columns of cervical spinal cord segments; facial nucleus (medulla oblongata), nerve, facial nucleus, muscles of ear; connections between cervical plexus and facial nerve
Dysuria (dribbling urine)
Spinal cord, S1-S5, sacral nerves, bladder wall
Diagnosis of Neurologic Diseases
Signalment
History
Diet
Dietary Deficiency
Disease Produced
Neurologic Sign
Copper
Demyelination, pathologic fractures of vertebrae
Ataxia, recumbency
Vitamin E
Demyelination
Ataxia, recumbency
Vitamin A
Encephalopathy
Convulsions, blindness
Magnesium
Grass tetany, transport tetany, milk tremors
Convulsions, tremors, ataxia
Potassium
Weakness
Postpartum recumbency
Calcium or phosphorus
Milk fever, pathologic vertebral fractures, tetany
Weakness, ataxia, recumbency, tetany
Vitamin E or selenium
Nutritional myodegeneration
Weakness, ataxia, recumbency, sudden death
Environment
Plant Poisoning
Clinical Signs
Blue green algae (Aphanizomenon, Anabaena flos-aquae)
Sudden death, tremors, salivation, miosis, bradycardia
Bracken fern (Pteridium aquilinum)
Ataxia, weight loss, strip sweating (horses only)
Buckeye (Aesculus species)
Incoordination, twitching, sluggishness
Catsear (Hypochaeris radicata)
Hyperflexion of the hock during movement (stringhalt)
Cheesewood (Malva)
Tremors, worsened by forced exercise, hyperflexion of the hock during movement (stringhalt)
Creeping indigo (Indigofera spicata) and Birdsville indigo (Indigofera linnae)
Ataxia, obtundation, blepharospasm, corneal edema, lingual ulcers, seizures
Dandelion (Taraxacum officinale)
Hyperflexion of the hock during movement (stringhalt)
Death camus (Zigadenus species)
Trembling, uncontrolled running, recumbency, opisthotonos, convulsions, vomiting, salivation
Dutchman’s breeches (Dicentra)
Trembling, uncontrolled running, recumbency, opisthotonos
Fiddleneck (Amsinckia intermedia)
Ataxia, obtundation, somnolence, excitability, head pressing (hepatic encephalopathy)
Horse tail (Equisetum arvense)
Ataxia, weight loss, strip sweating (horses only)
Laburnum (Laburnum anagyroides)
Excitement, incoordination, convulsions, death
Larkspur (Delphinium)
Ataxia, collapse, recumbency, inability to lift head, tremors of face, flank, and hip; vomiting
Locoweed (Astragalus species)
Ataxia, weight loss, recumbency, hyperesthesia
Lupine (Lupinus)
Tremors, hyperexcitability, depression
Milkweed (Asclepias species)
Tremors, salivation, ataxia
Monkshood (Aconitum)
Restlessness, salivation, paresthesia, irregular heartbeat, recumbency, coma
Nightshades (Atropa species, Solanum species)
Tremors, ataxia, recumbency, convulsions
Poison hemlock (Conium maculatum)
Tremors, vomiting, ataxia, sudden death, abortions, pupillary dilation, bradycardia, coma
Rape (Brassica napus)
Blindness, ataxia, aggressiveness
Rattlebox (Crotalaria spectabilis)
Ataxia, obtundation, somnolence, excitability, head pressing (hepatic encephalopathy)
Rayless goldenrod (Haplopappus heterophyllus)
Lassitude, obtundation, arched back, stiff-legged gait, tremors, weakness, collapse
Russian knapweed (Rhaponticum repens; Acroptilon repens)
Facial rigidity and dystonia, lack of prehension, ataxia, depression (horses only)
Tansy ragwort (Senecio jacobea) and common groundsel (Senecio vulgaris)
Ataxia, obtundation, somnolence, excitability, head pressing (hepatic encephalopathy)
Tobacco (Nicotiana species)
Tremors, salivation, ataxia, convulsions, birth defects
Water hemlock (Cicuta maculata)
Tremors, vomiting, ataxia, sudden death, convulsions, odontoprisis, pupillary dilation, abortions, bloat
White snakeroot (Eupatorium rugosum)
Tremors, salivation, convulsions
Yellow star thistle (Centaurea solstitialis)
Facial rigidity and dystonia, lack of prehension, ataxia, depression (horses only)
Vaccination and Disease History
Gestational Stage
Nervous System Examination
General Comments
Mentation and Behavior
Gait
Grade 0:
Normal gait
Grade 1:
Very subtle deficits, observed by only an experienced clinician
Grade 2:
Deficits apparent to an inexperienced clinician
Grade 3:
Deficits apparent to laypersons
Grade 4:
Severe deficits including stumbling, knuckling at the fetlock, falling
Grade 5:
Recumbency and inability to rise
Conscious Proprioception and Postural Reactions
Abnormalities of Posture and the Righting Response