Chapter 19 Laser Ear Surgery
Common ear ailments of dogs and cats can be seen in up to 50% of patients in areas of humid climates during some or all of the patient’s life. Dogs have a moderately higher incidence of ear disease than cats.
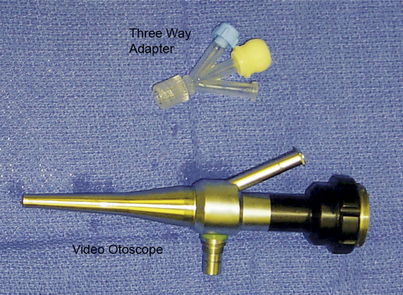
Therapeutic endoscopic telescopes are usually either the 0 degree (directly forward) or 30 degree (oblique view). Video otoscopes are 0 degree. They are usually larger (around 4.75 mm [because of the presence of an operating channel]), have a larger field of view, and are more durable and less costly than other rigid endoscopes. The single working channel of the video otoscope allows access for suction, biopsy, irrigation, and laser devices. The 2-mm channel accepts instrumentation up to 5 Fr, or about 1.8 mm. The biopsy channel can provide for simultaneous irrigation, suction, and treatment with the use of a two- or three-port connector, as shown in Figure 19-1.
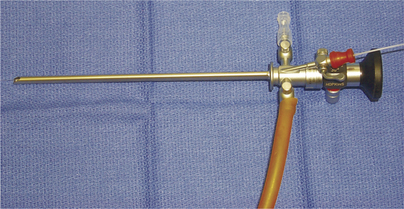
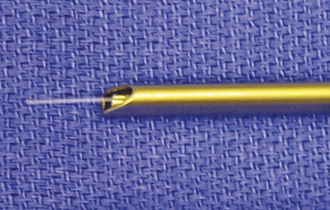
A 2.7- × 180-mm, 0-degree, or 30-degree rigid endoscopic telescope with a 14-Fr operating sheath can also be used in these procedures. The smaller overall diameter, longer length, and separate irrigation and operating channels make this endoscope an excellent choice for interventional otoscopy (Figure 19-2). The 30-degree endoscope is particularly useful in laser surgery and treating lesions of the middle ear. The 30-degree offset allows for visualization of the laser delivery system or surgical instrumentation as it exits the operating channel (Figure 19-3). This allows for more precise alignment of the instrument and decreases the possibility of iatrogenic damage. Because of the higher cost and increased fragility of this equipment, it should not be used in conscious patients.
Lasers can both extend and enhance the therapeutic options for the treatment of aural disease. Two types of lasers are useful in the treatment of auricular pathology. They are the CO2 laser (10,600-nm wavelength) and the diode laser (either 810- or 980-nm wavelength). It is beyond the scope of this chapter to discuss fully the physics involved with each of these wavelengths. The practitioner is strongly encouraged to review and understand the concepts of power density and tissue interactions before using this technology. By combining lasers and video otoscopy, a wider range of problems can be corrected in a minimally invasive fashion. This often leads to a better outcome. Lasers can prove extremely useful in the following:
In general lasers can be used in three different modalities:
A Comparison of CO2 and Diode Laser Energy
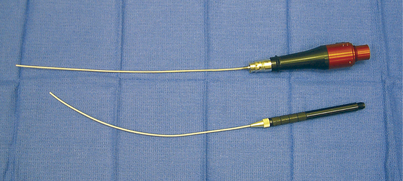
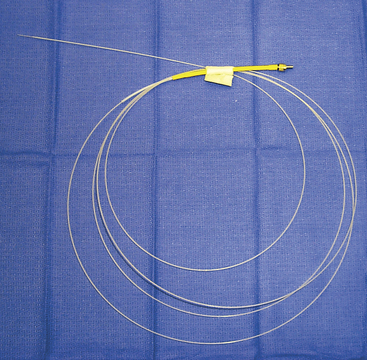
The CO2 laser energy is usually delivered through a semiflexible hollow tube (Figure 19-4) that guides the energy to the target through the operating channel of the endoscope. CO2 laser energy is most useful in the ablation (vaporization) of abnormal tissue. It can also be effectively used to provide hemostasis. In cases where the base of the auricular mass is visible, the laser can be used in an incisional mode to remove these structures more quickly.
Diode laser energy is absorbed by hemoglobin, oxyhemoglobin, and melanin. This selective absorption may aid in treatment if the abnormal area is more pigmented than the surrounding tissue. Lesions can be treated in a contact or noncontact mode. The noncontact mode is usually used only on pigmented lesions on the pinna. The noncontact mode has not been proven to be useful in a fluid environment. Diode laser energy is delivered by a shielded flexible quartz fiber (Figure 19-5). This system allows for the precise delivery of laser energy in a fluid environment in a contact mode. The fiber delivery system of the diode laser may become extremely hot when energized for a prolonged period. This depends on the fiber size, the energy setting (wattage), and the vascularity of the tissue (thermal diffusion). If the fiber becomes overheated, peripheral thermal damage results. It is vital to keep the fiber cool. This can be accomplished by limiting the exposure time (pulse duration) and by cooling the fiber with an irrigant such as saline. The ability to operate immersed in fluid makes the diode laser extremely useful in otoendoscopy. Continual irrigation during the procedure increases visualization and decreases unintentional iatrogenic damage. Irrigation also removes debris and helps control any heat from the laser or the endoscope.
Specific Laser Therapy Goals
The first step in the use of laser energy is to determine the way the energy is to be applied to the target tissue. Typically on the pinna, standard laser techniques can be used to accomplish the desired goals. Here the CO2 laser is clearly superior because of its reduced peripheral thermal tissue interaction and noncontact application. Surgery of the pinna can be provided by laser energy, similar to techniques for other areas of the dermis. In the external ear canal the video otoscopic or fiberoptic telescope can be used to facilitate visualization and direction of the laser energy. This is usually accomplished by extending the direction of the laser energy through special tips that fit into and through working channels in the otoscopic equipment. Diode laser fibers are usually between 400 and 1000 microns and easily fit most working channels. This allows the clinician to visualize the area and provide treatment within the confined space of the external ear canal.
Treatment of Aural Hematomas
Aural hematomas occur when a vessel within the pinna ruptures and blood accumulates under the skin. Aural hematomas occur on the inner (concave) surface of the pinna and can occur in both dogs and cats (Figure 19-6). Because the skin is so firmly attached to the auricular cartilage on the concave surface, the hematoma actually develops subparachondrally or intrachondrally, not subcutaneously.1 Most aural hematomas are lined by cartilage; this suggests that damage to this cartilage may play a role in their occurrence.2 The etiology of this condition is unknown. It may result from self-trauma or head shaking (secondary to otitis externa or media or to external parasites), trauma, increased vascular fragility, hemorrhagic diathesis, or some form of immune-mediated disease.3 Any underlying pathology should be addressed as part of the therapy. It may be wise to delay treatment in thrombocytopenic patients until any platelet abnormality has been corrected.
Three or more round, partial-thickness circular skin incisions of approximately 0.3 to 0.7 centimeters are made in a triangular pattern (Figure 19-7). The size of the opening depends on the size of the patient. After this pattern has been made, one of the proximal incisions is continued to full thickness to penetrate the hematoma. At this time the fluid within the hematoma is removed. This fluid is usually hemorrhagic to serohemorrhagic, depending on the length of time the hematoma has been present. After the fluid has been removed, the remaining incisions are continued to full thickness. At this time any fibrin clots should be removed from the subcutaneous space. It may be useful to lavage the space gently with normal saline or lactated Ringer’s solution.
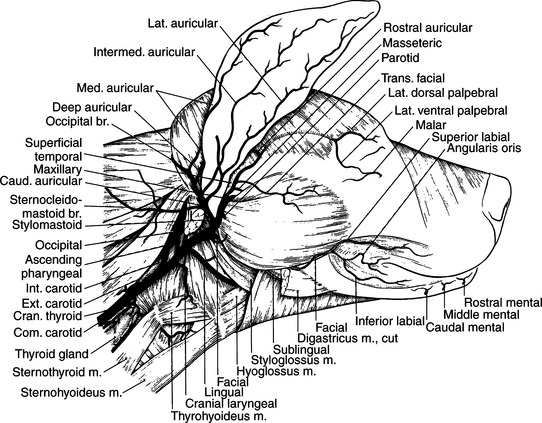
The skin is then sutured with stented 0 Prolene or nylon (3-0 Prolene for feline patients) to the underlying cartilage in a simple interrupted pattern. Only the inner pinna and the cartilage are sutured (Figure 19-8). The sutures should not penetrate the outer (dorsal) skin surface of the pinna. A taper needle is less likely to cause inadvertent bleeding and is preferred. The long axis of the individual sutures should be parallel to the long axis of the ear. This helps to preserve the normal blood supply to the pinna and avoid the three major branches of the auricular artery. After completion of the procedure, 0.006 mg/kg of buprenorphine (Buprenex) is given intravenously. Usually no additional pain control medication is required. An Elizabethan collar is placed to prevent self-trauma. Bandaging of the ear is not necessary or recommended. An alternative procedure that does not involve sutures has been published and may also be effective.4
Aftercare is performed at home by the client. This consists of twice-daily hot compresses applied to the ear for 5 to 10 minutes each. Any scab that forms should be removed, and the drain holes should be kept open for as long as possible. Any reaccumulation of fluid should be gently expressed during the process of compressing. Follow-up visits should be encouraged on a weekly basis. The drain holes usually will close by the second postoperative week. Sutures should be left in place for approximately 7 days after they have closed. Any otitis that is discovered during the course of treatment must be fully and aggressively treated. It is recommended that the otitis be completely resolved for at least 5 days before suture removal.
Neoplasia of the Pinna
Tumors of the ear may originate from the skin, adnexa, or connective tissue. These tumors include papilloma, fibropapilloma, mast cell tumor, cutaneous hemangioma, cutaneous hemangiosarcoma, melanoma, histiocytoma, fibrosarcoma, apocrine gland cyst, rhabdomyoma, and plasma cell tumors.2,5,6,7 Tumors can occur on either side of the pinna. Growths that occur on the outer (convex) surface of the ear are more likely to be centrally located and rarely penetrate the underlying cartilage. Excision of these masses is readily accomplished due to the loose attachment of the skin to the underlying cartilage. When removing these masses, it is important to identify the three main branches of the auricular artery (Figure 19-9). The CO2 laser is useful in these cases. In cases where the mass is a small papilloma, the laser may be used to ablate the mass (Figure 19-10). In all other cases the laser should be used to excise the mass completely. The skin should be closed with 3-0 to 5-0 monofilament nonabsorbable suture. Even in cases that require removal of auricular cartilage, only the skin should be sutured. Deficits that cannot be closed without causing deformity to the ear should be allowed to heal by secondary intention or repaired by the use of a pedicle flap.8 The excised tissue should undergo histopathologic evaluation. Malignant or incompletely excised neoplasia requires additional treatment, up to and including amputation of the pinna. Use of the CO2 laser in these cases increases hemostasis and postoperative patient comfort, thus helping to prevent surgical complications.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree