CHAPTER | 7 Hypersensitivity Disorders
Canine Atopy (environmental, pollen allergies)
Diagnosis
Treatment and Prognosis
 Potent, long-acting injectable steroids are contraindicated for the treatment of allergies because of their comparatively short anti-inflammatory benefits (3 weeks) relative to their prolonged metabolic and immunodepressive effects (6–10 weeks).
Potent, long-acting injectable steroids are contraindicated for the treatment of allergies because of their comparatively short anti-inflammatory benefits (3 weeks) relative to their prolonged metabolic and immunodepressive effects (6–10 weeks). Injectable short-acting steroids (dexamethasone sodium phosphate 0.5–1 mg/kg or prednisolone acetate 0.1–1 mg/kg) are effective at providing relief and may last 2 to 3 weeks if no concurrent secondary infection occurs. This treatment option allows the clinician to more closely control and monitor the patient’s use of steroids compared with oral treatments administered by the owner.
Injectable short-acting steroids (dexamethasone sodium phosphate 0.5–1 mg/kg or prednisolone acetate 0.1–1 mg/kg) are effective at providing relief and may last 2 to 3 weeks if no concurrent secondary infection occurs. This treatment option allows the clinician to more closely control and monitor the patient’s use of steroids compared with oral treatments administered by the owner. Temaril-P (trimeprazine and prednisolone combination) is a unique drug that provides significant antipruritic effects at a relatively lower dose of the prednisolone. One tablet per 10 to 20 kg should be administered every 24 to 48 hours. The dosage should be tapered to the lowest possible dose and frequency.
Temaril-P (trimeprazine and prednisolone combination) is a unique drug that provides significant antipruritic effects at a relatively lower dose of the prednisolone. One tablet per 10 to 20 kg should be administered every 24 to 48 hours. The dosage should be tapered to the lowest possible dose and frequency. Prednisone 0.25–1 mg/kg (or methylprednisolone 0.2–0.8 mg/kg) PO should be administered every 24 to 48 hours for 3 to 7 days. The dosage should be tapered to the lowest possible dose and frequency.
Prednisone 0.25–1 mg/kg (or methylprednisolone 0.2–0.8 mg/kg) PO should be administered every 24 to 48 hours for 3 to 7 days. The dosage should be tapered to the lowest possible dose and frequency.TABLE 7-1 Antihistamine Therapy in Dogs*
| Antihistamine | Dose |
|---|---|
| Chlorpheniramine | 0.2–3 mg/kg PO q 8–12 hours |
| Diphenhydramine | 1–4 mg/kg PO q 8 hours |
| Hydroxyzine | 3–7 mg/kg PO q 8 hours |
| Amitriptyline | 1–2 mg/kg PO q 12 hours |
| Cyproheptadine | 0.1–2 mg/kg PO q 8–12 hours |
| Trimeprazine | 0.5–5 mg/kg PO q 8–12 hours |
| Brompheniramine | 0.5–2 mg/kg PO q 12 hours |
| Clemastine | 0.05–1.5 mg/kg PO q 12 hours |
| Terfenadine | 0.25–1.5 mg/kg PO q 12–24 hours |
| Astemizole | 1 mg/kg PO q 12–24 hours |
| Promethazine | 1–2.5 mg/kg PO q 12 hours |
| Loratadine | 0.5 mg/kg PO q 24 hours |
| Cetirizine | 0.5–1 mg/kg PO q 24 hours |
| Doxepin | 0.5–1 mg/kg PO q 8–12 hours |
| Dimenhydrinate | 8 mg/kg PO q 8 hours |
| Tripelennamine | 1 mg/kg PO q 12 hours |
| Clomipramine | 1–3 mg/kg PO q 24 hours |
* Antihistamines in bold are preferred by the author.

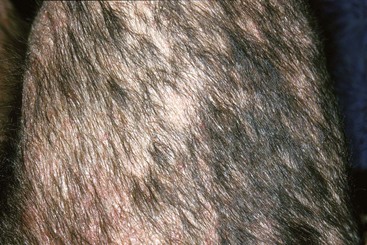
FIGURE 7-4 Canine Atopy.
Close-up of the dog in Figure 7-3. The periocular alopecia and hyperpigmentation caused by facial pruritus are typical of allergic disease.

FIGURE 7-5 Canine Atopy.
Periocular alopecia, erythema, hyperpigmentation, and lichenification caused by pruritus.

FIGURE 7-7 Canine Atopy.
Pododermatitis demonstrating the salivary staining caused by chronic licking.

FIGURE 7-12 Canine Atopy.
Sterile otitis caused by allergy often presents with erythema of the ear pinna and external canal.

FIGURE 7-14 Canine Atopy.
Secondary bacterial pyoderma (erythematous papular rash) on the inguinal area of an allergic dog.

FIGURE 7-17 Canine Atopy.
Severe erythema of the feet caused by intense pruritus and by the patient self-mutilating his feet.

FIGURE 7-18 Canine Atopy.
Same dog as in Figure 7-17 demonstrating the severe pododermatitis typical of atopy. Note the erythema on the abdomen, which is common with allergies.

FIGURE 7-20 Canine Atopy.
Same patient as in Figure 7-19. This intradermal allergy test (IDAT) demonstrates positive reactions with classic erythematous, well-demarcated, raised reactions. Note the difference between negative and positive reactions.

FIGURE 7-24 Canine Atopy.
Severe interdigital dermatitis with ulceration caused by secondary bacterial and yeast infections.

FIGURE 7-27 Canine Atopy.
Same dog as in Figure 7-26. Periocular dermatitis caused by the allergic reaction is obvious.

FIGURE 7-28 Canine Atopy.
Interdigital dermatitis with salivary staining is extremely common in atopic patients.
Canine Food Hypersensitivity
Diagnosis
Treatment and Prognosis
 Potent, long-acting injectable steroids are contraindicated for the treatment of allergies because of their comparatively short anti-inflammatory benefits (3 weeks) relative to their prolonged metabolic and immunodepressive effects (6–10 weeks).
Potent, long-acting injectable steroids are contraindicated for the treatment of allergies because of their comparatively short anti-inflammatory benefits (3 weeks) relative to their prolonged metabolic and immunodepressive effects (6–10 weeks). Injectable short-acting steroids (dexamethasone sodium phosphate 0.5–1 mg/kg or prednisolone acetate 0.1–1 mg/kg) are effective at providing relief and may last 2 to 3 weeks if no concurrent secondary infection occurs. This treatment option allows the clinician to more closely control and monitor the patient’s use of steroids compared with oral treatments administered by the owner.
Injectable short-acting steroids (dexamethasone sodium phosphate 0.5–1 mg/kg or prednisolone acetate 0.1–1 mg/kg) are effective at providing relief and may last 2 to 3 weeks if no concurrent secondary infection occurs. This treatment option allows the clinician to more closely control and monitor the patient’s use of steroids compared with oral treatments administered by the owner.
FIGURE 7-32 Canine Food Hypersensitivity.
Close-up of the dog in Figure 7-31. Erythema, alopecia, and papular rash involving the ear pinnae. No infectious otitis is present—only external lesions associated with the underlying allergy.

FIGURE 7-33 Canine Food Hypersensitivity.
Close-up of the dog in Figure 7-31. Alopecia and erythema in the axillary area. Mild hyperpigmentation and lichenification are caused by a secondary yeast dermatitis. Note the similarity to lesions seen with atopy.

FIGURE 7-43 Canine Food Hypersensitivity.
Facial dermatitis (alopecia, erythema, and pruritus) is a common finding in allergic dogs.

FIGURE 7-44 Canine Food Hypersensitivity.
Perianal dermatitis is one of the most consistent and unique features of food allergy.
Acral Lick Dermatitis (lick granuloma)
Features
Acral lick dermatitis is first noted as excessive, compulsive licking at a focal area on a limb, resulting in a firm, proliferative, ulcerative, alopecic lesion. Causes of the licking are multifactorial, and, although environmental stress (e.g., boredom, confinement, loneliness, separation anxiety) may be a contributor, other factors are usually more important (Box 7-1). This dermatitis is common in dogs, with the highest incidence in middle-aged to older, large-breed dogs, especially Doberman pinschers, Great Danes, Golden retrievers, Labrador retrievers, German shepherds, and Boxers.
Diagnosis
Treatment and Prognosis
TABLE 7-2 Drugs for Psychogenic Dermatoses in Dogs
| Drug | Dose |
|---|---|
| Anxiolytics | |
| Phenobarbital | 2–6 mg/kg PO q 12 hours |
| Diazepam | 0.2 mg/kg PO q 12 hours |
| Hydroxyzine | 2.2 mg/kg PO q 8 hours |
| Tricyclic Antidepressants | |
| Fluoxetine | 1 mg/kg PO q 24 hours |
| Amitriptyline | 1–3 mg/kg PO q 12 hours |
| Imipramine | 2–4 mg/kg PO q 24 hours |
| Clomipramine | 1–3 mg/kg PO q 24 hours |
| Endorphin Blocker | |
| Naltrexone | 2 mg/kg PO q 24 hours |
| Endorphin Substitute | |
| Hydrocodone | 0.25 mg/kg PO q 8 hours |
| Topical Products | |
| Fluocinolone acetonide + Flunixin meglumine | |
| Deep Heet + Bitter Apple | |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree