CHAPTER | 8 Autoimmune and Immune-Mediated Skin Disorders
Historically, steroid therapy has been the mainstay of treatment for these diseases. We are beginning to realize the usefulness of nonsteroid alternatives (Table 8-1) in many cases, with mild cases often not requiring any steroid therapy.
TABLE 8-1 Immunosuppressive Therapies for Autoimmune and Immune-Mediated Skin Disease
| Drug—Species | Induction Dosage | Maintenance Dosage |
|---|---|---|
| Topical Therapy | ||
| Steroids (hydrocortisone, dexamethasone, triamcinolone, fluocinolone, betamethasone, mometasone, etc.) | Applied every 12 hours | Taper to lowest effective dose |
| Tacrolimus | Applied every 12 hours | Taper to lowest effective dose |
| Conservative Oral Treatments With Very Few Adverse Effects | ||
| Essential fatty acids—dogs and cats | 180 mg EPA/10 lb PO daily | |
| Vitamin E | 400 IU PO daily | |
| Tetracycline and niacinamide—dogs | Dogs >10 kg—500 mg of each drug PO q 8 hours Dogs <10 kg—250 mg of each drug PO q 8 hours | Dogs >10 kg—500 mg of each drug PO q 12–24 hours Dogs >10 kg—250 mg of each drug PO q 12–24 hours |
| Doxycycline may be substituted for tetracycline | 5–10 mg/kg q 12 hours | Then, taper to lowest effective dose |
| Cyclosporine (Atopica)—dogs and cats | 5–12.5 mg/kg PO q 12–24 hours | After remission is achieved, taper slowly to lowest effective dose |
| Reliably Effective Treatments But Adverse Effects Are Common and May Be Severe | ||
| Prednisone—dogs | 1–3 mg/kg PO q 12–24 hours | 0.5–2 mg/kg PO q 48 hours |
| Prednisolone—cats | 2–2.5 mg/kg PO q 12–24 hours | 2.5–5 mg/kg PO q 2–7 days |
| Methylprednisolone—dogs | 0.8–1.4 mg/kg PO q 12–24 hours | 0.4–0.8 mg/kg PO q 48 hours |
| Triamcinolone—dogs | 0.1–0.3 mg/kg PO q 12–24 hours | 0.1–0.2 mg/kg PO q 48–72 hours |
| Triamcinolone—cats | 0.3–1 mg/kg PO q 12–24 hours | 0.6–1 mg/kg PO q 2–7 days |
| Dexamethasone—dogs and cats | 0.1–0.2 mg/kg PO q 12–24 hours | 0.05–0.1 mg/kg PO q 48–72 hours |
| Azathioprine—dogs | 1.5–2.5 mg/kg PO q 24–48 hours | 1.5–2.5 mg/kg PO q 48–72 hours |
| Chlorambucil—dogs and cats | 0.1–0.2 mg/kg PO q 24 hours | 0.1–0.2 mg/kg PO q 48 hours |
| Dapsone—dogs only | 1 mg/kg PO q 8 hours | Taper to lowest effective dose |
| Aggressive Treatments With Few Studies Documenting Efficacy and Safety | ||
| Methylprednisolone sodium succinate (pulse therapy)—dogs and cats | 1 mg/kg IV over a 3- to 4-hour period q 24 hours for 2–3 consecutive days | Alternate-day oral glucocorticosteroid |
| Dexamethasone (pulse therapy)—dogs and cats | 1 mg/kg IV once or twice 24 hours apart | Alternate-day oral glucocorticosteroid |
| Cyclophosphamide—dogs and cats | 50 mg/m2 (or 1.5 mg/kg) PO q 48 hours | 25–50 mg/m2 (or 0.75–1.5 mg/kg) PO q 48 hours |
| Mycophenolate mofetil | 10–20 mg/kg q 8–12 hours | Then, taper to lowest effective dose |
| Leflunomide | 2 mg/kg q 12 hours | Then, taper to lowest effective dose |
Pemphigus Foliaceus
Diagnosis
Treatment and Prognosis
 Immunosuppressive doses of oral prednisone or methylprednisolone should be administered daily (see Table 8-1). After lesions resolve (after approximately 2–8 weeks), the dosage should be gradually tapered over a period of several (8–10) weeks until the lowest possible alternate-day dosage that maintains remission is being administered. If no significant improvement is seen within 2 to 4 weeks of initiation of therapy, a concurrent skin infection should be ruled out, then alternative or additional immunosuppressive medications considered.
Immunosuppressive doses of oral prednisone or methylprednisolone should be administered daily (see Table 8-1). After lesions resolve (after approximately 2–8 weeks), the dosage should be gradually tapered over a period of several (8–10) weeks until the lowest possible alternate-day dosage that maintains remission is being administered. If no significant improvement is seen within 2 to 4 weeks of initiation of therapy, a concurrent skin infection should be ruled out, then alternative or additional immunosuppressive medications considered. Alternative steroids for prednisone- and methylprednisolone-refractory cases include triamcinolone and dexamethasone (see Table 8-1).
Alternative steroids for prednisone- and methylprednisolone-refractory cases include triamcinolone and dexamethasone (see Table 8-1). In cats, treatment with immunosuppressive doses of triamcinolone or dexamethasone is often more effective than therapy with prednisolone or methylprednisolone. Oral triamcinolone or dexamethasone should be administered daily until remission is achieved (approximately 2–8 weeks), then the dosage should be gradually tapered until the lowest possible and least frequent dosage that maintains remission is being administered (see Table 8-1).
In cats, treatment with immunosuppressive doses of triamcinolone or dexamethasone is often more effective than therapy with prednisolone or methylprednisolone. Oral triamcinolone or dexamethasone should be administered daily until remission is achieved (approximately 2–8 weeks), then the dosage should be gradually tapered until the lowest possible and least frequent dosage that maintains remission is being administered (see Table 8-1).
FIGURE 8-1 Pemphigus Foliaceus.
An adult Doberman with pemphigus foliaceus. Note the diffuse pattern of lesions.

FIGURE 8-2 Pemphigus Foliaceus.
Same dog as in Figure 8-1. Alopecic, crusting, papular lesions on the face are apparent. Note the similarity of lesions to folliculitis; however, the pattern of distribution is unique.

FIGURE 8-4 Pemphigus Foliaceus.
Same dog as in Figure 8-3. Alopecic, crusting, papular dermatitis on the face and nasal planum is characteristic of autoimmune skin disease. Note the similarity to folliculitis lesions; however, no follicles are present on the nasal planum, making these lesions a unique feature.

FIGURE 8-6 Pemphigus Foliaceus.
Same dog as in Figure 8-5. Lesions on the nasal planum are characteristic of autoimmune skin disease.

FIGURE 8-13 Pemphigus Foliaceus.
Hyperkeratosis and crusting of the scrotum of a dog with pemphigus foliaceus.

FIGURE 8-17 Pemphigus Foliaceus.
Close-up of the cat in Figure 8-16. The alopecic, crusting, papular dermatitis on the face and ear pinna is characteristic of autoimmune skin disease.

FIGURE 8-18 Pemphigus Foliaceus.
Same cat as in Figure 8-16. The crusting papular rash on the ear pinna is a unique feature of autoimmune skin disease.

FIGURE 8-19 Pemphigus Foliaceus.
Same cat as in Figure 8-16. Alopecic, crusting, erosive dermatitis around the nipples is a common and unique feature of pemphigus foliaceus in cats.

FIGURE 8-21 Pemphigus Foliaceus.
Hyperkeratosis and crusting on the footpads are common features of autoimmune skin disease.

FIGURE 8-23 Pemphigus Foliaceus.
Paronychia and hyperkeratosis of the footpads in a cat with pemphigus foliaceus.
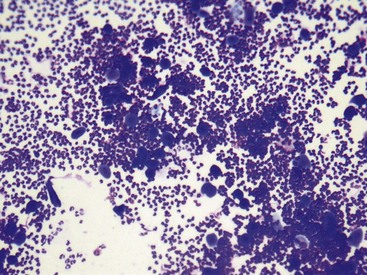
FIGURE 8-24 Pemphigus Foliaceus.
Microscopic image of acantholytic cells and numerous neutrophils as viewed with a 10× objective.
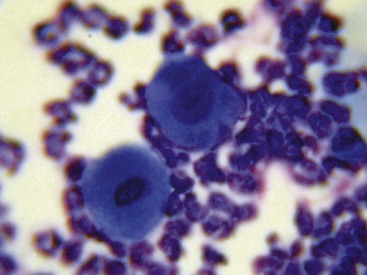
FIGURE 8-25 Pemphigus Foliaceus.
Microscopic image of acantholytic cells as viewed with a 100× (oil) objective.

FIGURE 8-27 Pemphigus Foliaceus.
Severe crusting of the footpads developed over several weeks in a middle-aged dog.

FIGURE 8-29 Pemphigus Foliaceus.
Severe paronychia, exudative dermatitis with crusting, is a common feature of pemphigus in cats.

FIGURE 8-31 Pemphigus Foliaceus.
Close-up of the dog as in Figure 8-30. Alopecia with crusting around the eye is apparent.

FIGURE 8-32 Pemphigus Foliaceus.
Same dog as in Figure 8-30. Crusting of the footpads is a characteristic feature of most autoimmune skin diseases.

FIGURE 8-38 Pemphigus Foliaceus.
Severe alopecia with punctate, crusted erosions on the ear pinna of a dog with pemphigus.

FIGURE 8-41 Pemphigus Foliaceus.
Alopecic, crusting dermatitis around the eye of a dog with pemphigus.
Pemphigus Erythematosus
Diagnosis
Treatment and Prognosis
 Immunosuppressive doses of oral prednisone or methylprednisolone should be administered daily (see Table 8-1). After lesions resolve (after approximately 2–8 weeks), the dosage should be gradually tapered over a period of several (8–10) weeks until the lowest possible alternate-day dosage that maintains remission is being administered. If no significant improvement is seen within 2 to 4 weeks of initiation of therapy, concurrent skin infection should be ruled out, then alternative or additional immunosuppressive medications considered.
Immunosuppressive doses of oral prednisone or methylprednisolone should be administered daily (see Table 8-1). After lesions resolve (after approximately 2–8 weeks), the dosage should be gradually tapered over a period of several (8–10) weeks until the lowest possible alternate-day dosage that maintains remission is being administered. If no significant improvement is seen within 2 to 4 weeks of initiation of therapy, concurrent skin infection should be ruled out, then alternative or additional immunosuppressive medications considered. Alternative steroids for prednisone- and methylprednisolone-refractory cases include triamcinolone and dexamethasone (see Table 8-1).
Alternative steroids for prednisone- and methylprednisolone-refractory cases include triamcinolone and dexamethasone (see Table 8-1). In cats, treatment with immunosuppressive doses of triamcinolone or dexamethasone often is more effective than therapy with prednisolone or methylprednisolone. Oral triamcinolone or dexamethasone should be administered daily until remission is achieved (approximately 2–8 weeks), then the dosage should be gradually tapered until the lowest possible and least frequent dosage that maintains remission is being administered (see Table 8-1).
In cats, treatment with immunosuppressive doses of triamcinolone or dexamethasone often is more effective than therapy with prednisolone or methylprednisolone. Oral triamcinolone or dexamethasone should be administered daily until remission is achieved (approximately 2–8 weeks), then the dosage should be gradually tapered until the lowest possible and least frequent dosage that maintains remission is being administered (see Table 8-1).
FIGURE 8-46 Pemphigus Erythematosus.
Same dog as in Figure 8-45. Depigmenting erosive lesions on the nasal planum.
Pemphigus Vulgaris
Diagnosis
Treatment and Prognosis
Because Pemphigus vulgaris is usually severe, aggressive therapy is usually required.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree




























































