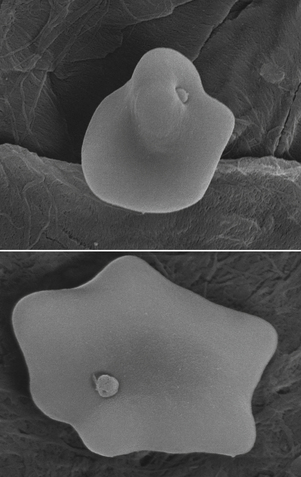
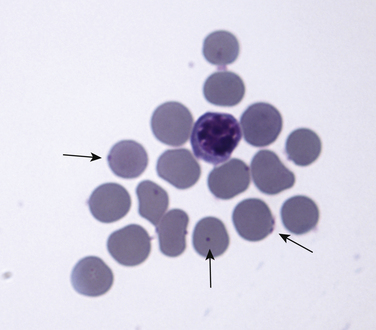
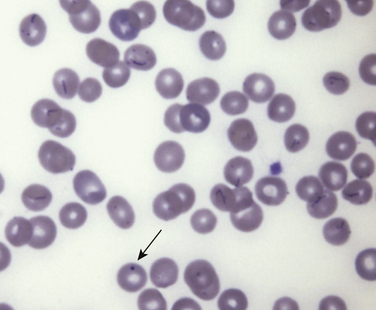
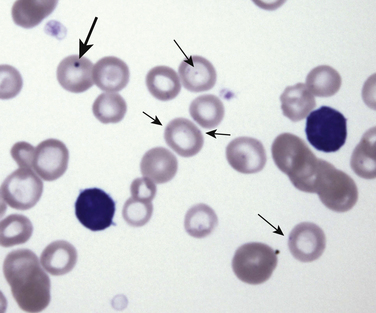
Chapter 41 At least three hemoplasma species infect domestic as well as wild cats, Mycoplasma haemofelis, ‘Candidatus Mycoplasma haemominutum,’ and ‘Candidatus Mycoplasma turicensis.’ The ‘Candidatus’ prefix is applied to newly discovered hemoplasmas until more information is available to support their classification. This is because hemoplasmas cannot be cultured in the laboratory, which limits full characterization of these organisms. M. haemofelis (previously the Ohio strain, or large form of Haemobartonella felis) is the most pathogenic organism and can cause moderate to severe hemolytic anemia in immunocompetent cats. The resulting disease has been referred to as feline infectious anemia. Using cytologic evaluation of blood smears, M. haemofelis organisms are cocci that sometimes form short chains of three to six organisms (Figure 41-1). M. haemofelis is the least prevalent of the three feline hemoplasmas. It has been found using PCR in 0.5% to 5% of sick cats at veterinary hospitals. The whole genome sequences of M. haemofelis and M. haemominutum have been determined.3–5 FIGURE 41-1 Romanowsky-stained blood smear from an 8-year-old male neutered domestic shorthair cat showing epierythrocytic bacteria typical of Mycoplasma haemofelis (arrows). ‘Ca. M. haemominutum’ (previously the California strain or small form of H. felis) is generally smaller than M. haemofelis and has not clearly been associated with disease in immunocompetent cats. Using cytologic evaluation of blood smears, ‘Ca. M. haemominutum’ are small cocci, 0.3 to 0.6 µm in diameter, although M. haemofelis and ‘Ca. M. haemominutum’ cannot always reliably be distinguished by this method. ‘Ca. M. haemominutum’ is common in the cat population worldwide, infecting as many as 20% of cats that visit veterinary hospitals.6–8 Infection of cats with ‘Ca. M. haemominutum’ results in a mild decrease in hematocrit. There is some evidence that ‘Ca. M. haemominutum’ may play a role in disease. For example, cats that are co-infected with FeLV and ‘Ca. M. haemominutum’ develop more significant anemia than cats infected with ‘Ca. M. haemominutum’ alone, and progression to FeLV-induced myeloproliferative disease occurred more rapidly.9 There are also descriptions of cats with hemolytic anemia in which the only recognized cause of anemia was ‘Ca. M. haemominutum.’10 ‘Ca. M. haemominutum’ is commonly found in co-infections with ‘Ca. M. turicensis’ or M. haemofelis. Mixed infections with all three feline hemoplasma species also have been described. ‘Ca. M. turicensis’ was first described in a cat from Switzerland that had severe intravascular hemolysis (turicensis pertains to Turicum, the Latin name of Zurich).11 Infections with ‘Ca. M. turicensis’ have since been detected worldwide.8,12–14 ‘Ca. M. turicensis’ has never been seen using light microscopic examination of blood smears, and organism loads in infected cats are typically low. Infection with ‘Ca. M. turicensis’ is slightly more prevalent in the cat population than infection with M. haemofelis. Most studies show a prevalence of 0.5% to 10% in sick cats that visit veterinary hospitals. The pathogenic potential of this organism is not fully understood. Inoculation of an immunosuppressed cat with ‘Ca. M. turicensis’ resulted in severe anemia,11 but little or no anemia occurs in immunocompetent cats after inoculation with ‘Ca. M. turicensis.’ Cofactors, such as co-infection with other hemoplasmas or concurrent immunosuppression, may influence the development of anemia in cats infected with ‘Ca. M. turicensis.’ Infection of cats by hemoplasmas is strongly associated with male sex, nonpedigree status, and outdoor access (Box 41-1).8,12,15,16 Infection with ‘Ca. M. haemominutum’ is more prevalent in older cats, presumably because the chance of acquiring persistent subclinical infection increases over time. In contrast, young cats may be more likely to develop disease after infection by M. haemofelis. Some studies, but not others, have shown an association between retrovirus and hemoplasma infections. Cats infected with M. haemofelis in the United States were 6 times more likely to be FIV infected than cats negative for hemoplasmas.15 Several hemoplasma species also infect dogs. Infection with Mycoplasma haemocanis (previously Haemobartonella canis) has been associated with hemolytic anemia in splenectomized dogs, and rarely in dogs with other immunosuppressive disease or concurrent infections. The 16S rRNA gene of M. haemocanis has the same sequence as M. haemofelis, but the whole genome sequence of M. haemocanis distinguishes it as a different species.17 M. haemocanis is a coccoid organism that often forms long chains of organisms (Figure 41-2). The prevalence of this infection is particularly high in kennel-raised dogs, which are often infected subclinically.18 In the southwestern United States, infection was also prevalent among coyotes.19 FIGURE 41-2 Romanowsky-stained blood smear showing chains of epierythrocytic bacteria typical of Mycoplasma haemocanis. A Howell-Jolly body is also present (arrow). Three additional hemoplasma species have been detected in dogs. ‘Candidatus Mycoplasma haematoparvum’ is a small (0.3 µm) coccoid organism that resembles ‘Ca. Mycoplasma haemominutum’ morphologically as well as genetically (Figure 41-3). ‘Ca. M. haemominutum’ has also been detected in several dogs using PCR assays, and organisms that resemble ‘Ca. M. haematoparvum’ and ‘Ca. M. haemominutum’ have been detected in European wolves and bush dogs from Brazil.20 The ovine hemoplasma Mycoplasma ovis was detected in the spleens of a small number of dogs from the southeastern United States, and the bovine hemoplasma ‘Ca. Mycoplasma haemobos’ was detected in a dog from northern Australia.21,22 The clinical importance of these hemoplasma species in dogs remains unclear. FIGURE 41-3 Blood smear from a dog showing ‘Candidatus Mycoplasma haematoparvum’ (small arrows) and a Howell-Jolly Body (large arrow). The mode of transmission of hemoplasmas remains unclear. To some extent, fleas and other arthropod vectors may be capable of transmitting feline hemoplasmas,23 but experimental evidence for vector-borne transmission of feline hemoplasmas is weak. Transmission of M. haemocanis by the brown dog tick, Rhipicephalus sanguineus, has been demonstrated experimentally, although this was before PCR assays were available to confirm infection.24 Geographic variation in the prevalence of hemoplasma infection in dogs and cats supports a role for arthropod vectors in transmission. For example, in Europe, infection with M. haemocanis is more prevalent in Mediterranean countries, which follows the distribution of Rh. sanguineus. Vertical (e.g., transplacental) spread has also been hypothesized and has been documented for bovine hemoplasmas. Biting has been suggested as a means of transmission of feline hemoplasmas, and the strong male sex predilection, recent history of cat bite abscessation in some cats, and association with FIV infection in some studies supports this mode. Additionally, studies in Switzerland found that subcutaneous inoculation of blood that contained ‘Ca. M. turicensis’ resulted in transmission, whereas inoculation of saliva that contained ‘Ca. M. turicensis’ did not.25 This suggests that hemoplasma transmission by social contact (saliva via mutual grooming etc.) is less likely than transmission by aggressive interaction (blood transmission during a cat bite incident). Because infection can also be transmitted by ingestion of blood, it may be that the biting cat (rather than the bitten cat) is most at risk for acquisition of infection. Transmission of M. haemocanis through ingestion of infected blood has also been described,26 so aggressive interactions between dogs may also have the potential to transmit hemoplasmas; however, this mode of transmission remains to be proven in field circumstances. Transmission can also occur following blood transfusion. Because only M. haemofelis infection is associated with significant anemia in cats, only the pathogenesis of disease induced by this species is described here. After experimental infection, there is a delay of 2 to 34 days before the onset of clinical signs. Anemia then occurs and persists for about 18 to 30 days (acute phase), although its severity and chronicity vary considerably between infected cats. Anemia predominantly results from extravascular hemolysis, and the onset of anemia is usually followed by a strong regenerative response with reticulocytosis. The organism resides in an indentation on the erythrocyte surface (Figure 41-4). Production of both cold and warm reactive erythrocyte-bound antibodies, increased osmotic fragility, and decreased erythrocyte life span have been noted in infected cats.27–29 The organisms can also “bridge” adjacent erythrocytes, which might promote splenic trapping and removal of red blood cells. In contrast, erythrocyte-bound antibody formation and significant reticulocytosis have not been documented in cats infected with ‘Ca. M. haemominutum’ or ‘Ca. M. turicensis.’ Anemia can result in signs of lethargy, inappetence, pallor, and weakness. Some owners report that their cats eat dirt or litter or lick cement (pica). Weight loss and dehydration can occur. Rapid development of anemia may result in neurologic signs, vocalization, collapse, and death. In some infected cats, cyclical changes in the hematocrit and numbers of infected erythrocytes occur, with sharp declines in the hematocrit correlating with appearance of large numbers of organisms in blood smears.30–32 The proportion of erythrocytes associated with visible organisms on blood smears can decline from 90% to less than 1% in less than 3 hours.33,34 These dramatic fluctuations in organism numbers appear to result from rapid replication of M. haemofelis, followed by rapid clearance from the blood as a result of the host’s immune response. Repeated antigenic variation in M. haemofelis may allow the organism to again proliferate in the face of this immune response, which contributes to ongoing fluctuations in organism numbers. In cats that survive the acute phase, the hematocrit then returns to normal or near-normal (recovery phase), and organisms can no longer be visualized in blood smears. It is possible that at least some of these recovered cats remain persistently infected, whereby the organism evades the host immune system, and that recrudescence of anemia may follow stress, pregnancy, intercurrent infection, or neoplasia.32,33 However, evidence is accumulating that differences may exist in the ability of hemoplasmas to persist within the host, the carrier state being more frequent for ‘Ca. M. haemominutum’ but less frequent for M. haemofelis and ‘Ca. M. turicensis.’ In cats, splenectomy has a variable effect on the course of hemoplasmosis. Recrudescence of anemia and bacteremia has been documented in some chronically infected cats after splenectomy, although other studies suggest that splenectomy increases the number of visible organisms in blood smears without causing significant anemia.32,34 Infection of splenectomized cats with ‘Ca. M. haemominutum’ does not appear to enhance the pathogenicity of this organism.35 Physical examination findings in cats with acute M. haemofelis infection include fever, weakness, mucosal pallor, tachypnea, tachycardia, and weak or bounding femoral pulse quality. Other physical examination abnormalities can include dehydration, cardiac murmurs, splenomegaly, and occasionally mild icterus (Figure 41-5). Moribund cats may be hypothermic. FIGURE 41-5 Mild icterus of the nictating membrane in an 8-year-old male neutered domestic shorthair with hemolytic anemia secondary to Mycoplasma haemofelis infection. Dogs with hemoplasmosis can show lethargy and mucosal pallor. Fever is usually absent.
Hemoplasma Infections
Etiology and Epidemiology
Clinical Features
Physical Examination Findings

![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree