Chapter 15 Gastrointestinal Diseases
Gastrointestinal Stasis Syndrome
The Role of Fiber
To understand the pathogenesis of diet-related and GI diseases of the rabbit, a thorough knowledge of the normal anatomic and physiologic aspects of rabbit digestion must be appreciated. Details of this are discussed in Chapter 14. In summary, rabbits have a unique digestive physiology. They are strict herbivores, but their digestive strategy differs from those of other hindgut or cecal fermenters (e.g., horses) and ruminants. Being a prey species of small size, rabbits rely on a high energy intake while at the same time having the ability to quickly eliminate fibrous waste that would otherwise have to be carried in the digestive tract. To accomplish this, the rabbit’s cecum and colon have a well-developed mechanism for separating out the digestible and readily fermentable components of the diet while allowing the crude fiber components to be purged. The main driving force for this mechanism is the presence of large quantities of indigestible fiber. Lack of this fiber, either due to dietary inadequacies or conditions that cause anorexia, is the major cause of GI disease in rabbits.12
Digesta are separated in the colon in a process of selective retention of fluid and small particles. Normal peristaltic movements propel the larger fiber particles through the colon, while contractions of the haustra in the colon move the fluid and small particles retrograde to the cecum. Small particles and fluid are retained in the cecum, allowing for extensive fermentation. Cecal contents are expelled at regular intervals and reflexively consumed directly from the anus. Fiber stimulates cecocolic motility, either by a distention effect of the bulk, or directly. For example, diets high in fiber promote the production of specific volatile fatty acids in the cecum that directly promote peristalsis.12
The Effect of Diet and Cecocolic Motility
Cecal bacteria are vital to health. The cecum acts as a fermentation chamber and contains large populations of anaerobic organisms, such as Bacteroides species, and large anaerobic metachromatic staining bacteria (LAMB).9,17,31 Other bacteria normally present include gram-negative oval and fusiform rods, along with several nonpathogenic species of protozoa and amoeba.31 A rabbit-specific ascosporogenous yeast (Cyniclomyces guttulatus), in the Saccharomyces family, resides in the normal rabbit cecum.20 Veterinarians unfamiliar with rabbit fecal flora commonly mistake this yeast for coccidia on fecal examinations. This combined microflora is responsible for the processing of food particles entering the cecum into digestible nutrients, which are then reingested as cecotrophs.
An inappropriate diet or GI stasis can disrupt the balance of this complex cecal microflora and the environment in which it grows. Diets low in fiber cause cecocolic hypomotility, prolonging the retention of digesta in the cecum and ultimately producing changes in cecal microflora. Populations of potentially pathogenic bacteria, primarily Clostridium species and coliform species such as Escherichia coli, are normally present in small numbers in the cecum.9,17,21 A slowing of cecocolic motility leads to the production of abnormal cecal fermentation products and alterations in the cecal pH. Even mild alterations in cecal pH will cause an increase in these pathogens as the populations of normal organisms decrease. Similarly, a decrease in peristalsis in the small intestine will allow normally small populations of potentially pathogenic bacteria to proliferate. Overgrowth of these pathogens can cause a range of pathology from mild diarrhea to death from enterotoxemia. Other effects of fiber consumption are indirect. High-fiber diets have a low level of available carbohydrates and thus decrease the risk of enterotoxemia caused by carbohydrate overload of the hindgut. Carbohydrates provide an environment in which pathogens such as E. coli and Clostridium species proliferate. Glucose, a byproduct of carbohydrate digestion, is necessary for the production of iota toxin by Clostridium species. Thus, diarrhea and enterotoxemia in pet rabbits is often caused by this disruption in microflora, commonly referred to as dysbiosis.
History and Clinical Signs
Obtain a complete dietary history, including the type and amount of commercial pelleted ration, hay, fresh leafy greens, and treats. Rabbits whose regular diet consists primarily of pelleted rations are at higher risk of developing GI stasis. The pelleted diets fed exclusively to feeder rabbits are high in calories (high in digestible carbohydrates), low in fiber, high in protein, and highly digestible, designed to increase weight gain in growing rabbits raised for their meat or fur. Commercial pellet formulations available for pet rabbits vary significantly in their protein, carbohydrate, and fiber contents. Formulations that contain a mix of dried fruits, vegetables, seeds, nuts, grains, and pellets generally have the lowest fiber content and the highest content of fat and carbohydrates. As the previous discussion indicates, there is significant potential for GI complications in a rabbit fed these diets. Similarly, rabbits routinely fed large amounts of high-carbohydrate, high-fat treats such as nuts, seeds, baked goods, and fruits are also predisposed to GI stasis. Acute episodes of GI stasis and dysbiosis are common following ingestion of a large volume of these treats. Rabbits at lowest risk are fed diets of unlimited grass or timothy hay, a moderate amount of fresh leafy greens, minimal commercial pellets, and occasional treats (see Chapter 14).
The most common presenting complaint in rabbits with GI stasis is a gradual decrease in appetite and subsequent decrease in fecal production. Appetite usually decreases over a period of 2 to 7 days. Most rabbits will first stop eating pellets, then greens, hay, and finally treats. Left untreated, they stop eating all foods. Water consumption is often decreased as well. Feces become scant, dry, and small, eventually ceasing altogether. Owners may report a corresponding decrease in activity, usually as a result of abdominal pain. Rabbits in pain are reluctant to move, appear less social, may grind their teeth, may dig or scratch, and sit in a hunched position. Weight loss may also be noted, either due to anorexia or underlying disease.
Diagnostic Testing
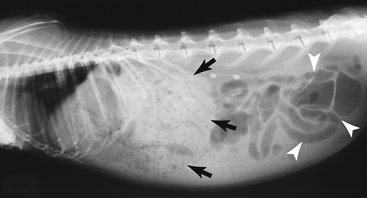
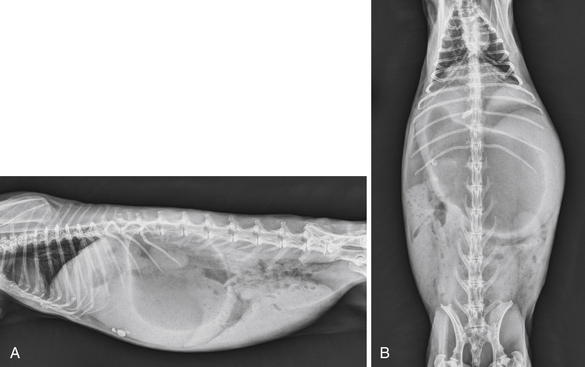
In many cases, the history and physical examination are sufficient for a diagnosis of GI stasis. It is very important, however, to look for an underlying cause. As discussed above, GI stasis occurs secondary to dietary or husbandry deficiencies, stress, pain, or underlying disease and will quickly recur if these are not addressed. Obtain additional diagnostics as indicated to rule out suspected underlying disorders. Radiography may or may not be helpful for diagnosis because the mass of food and hair appears similar to normal ingesta, even with contrast radiography. Visualization of a large, ingesta-filled stomach in a rabbit that has been anorexic for several days is suggestive (Fig. 15-1). This contrasts sharply with the dilated gas and/or fluid-filled stomach observed radiographically in rabbits with acute GI dilation (bloat) (Fig. 15-2) and can be helpful to differentiate the two disorders. Other common radiographic features seen in rabbits with GI stasis include moderate to severe distention of the intestines and cecum and scant fecal pellets. Radiographs may also be helpful to identify underlying causes of GI stasis.
Treatment
The key principles in the treatment of GI stasis are to rehydrate the patient and stomach contents, alleviate pain, provide nutrition, and treat any underlying disorders. Fluid therapy is essential to recovery. Administer fluids via either the intravenous or subcutaneous route, depending on the severity of dehydration. If they are anorexic for more than 1 to 2 days, affected rabbits are usually significantly dehydrated and generally require hospitalization for intravenous fluid therapy. Rehydrate the stomach contents by assisted feeding with a syringe or placing a nasogastric feeding tube (see Chapter 13) if the rabbit will not accept feeding slurries orally. A commercial product (Critical Care for Herbivores, Oxbow Pet Products, Murdock, NE) is available for this purpose, and most rabbits will readily accept this product when offered via a syringe. This formula is relatively high in fiber and will provide nutrition needed to stimulate GI motility in addition to rehydrating the stomach contents. If this formula is not available, blenderized pellets soaked with water or an oral electrolyte solution can be used. Feeding these slurries will also help to prevent hepatic lipidosis, which can develop rapidly in a rabbit with a negative energy balance. In addition to assisted feeding, offer rabbits water, plenty of fresh hay, and a variety of greens to provide every opportunity to self-feed. Ingestion of food is critical to reestablishing GI motility.
Acute Gastrointestinal Dilation or Obstruction
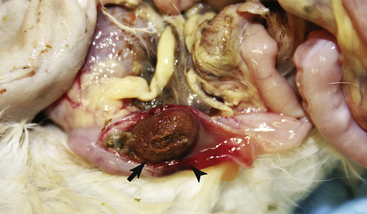
GI obstruction (also referred to as GI dilation or “bloat”) is an acute, life-threatening condition. The pathogenesis, history, and clinical findings differ significantly from those of GI stasis. Confusion arises over the use of the term trichobezoar. As discussed above, trichobezoar is a common misnomer for GI stasis. In most cases of acute GI dilation, the obstruction is located in the small intestine and is a compact mat of hair (trichobezoar). It is not clear exactly where these mats of hair are formed. They may have formed while still on the coat of the animal and have been ingested whole during grooming. It has also been suggested that these trichobezoars were once large cecal pellets containing compacted hair. They may occasionally be ingested and swallowed whole with other cecal contents during normal cechotrophy.24,25 Other foreign objects reported to acutely obstruct the intestinal tract include carpet or other cloth fibers, locust beans, and plastic.24,25 The location of the obstruction is usually in the proximal duodenum, a short distance from the pylorus where the lumen narrows, or in the midduodenum (Fig. 15-3). The second most common location is the ileocecocolonic junction. Acute compressions of the intestinal tract by neoplasia, postsurgical adhesions, tapeworm cysts, and hernias have also been reported.24,25 These all create a complete physical obstruction of the intestines and are not related to functional GI stasis. Rabbits cannot vomit and have a well-developed cardiac sphincter. When outflow from the stomach is obstructed, gastric fluid and swallowed saliva quickly accumulate. This fluid may undergo fermentation to produce large volumes of gas, resulting in a rise in intragastric pressure and a severely dilated stomach. As with gastric dilation in other species, the combination of sequestered fluid, compression of the aorta and vena cava causing hypovolemic shock, electrolyte imbalances, and acid-base disturbances can lead to death within hours of obstruction. Death can also be due to peritonitis resulting from ischemic necrosis at the site of the obstruction or rupture of the stomach.
Diagnostic Testing
Obtain radiographs to confirm the diagnosis. The radiographic appearance of a rabbit with acute GI obstruction differs sharply from that of a rabbit with GI stasis or that of a normal rabbit. The stomach will appear severely distended with gas, fluid, or both (see Fig. 15-2). Gas distention of intestinal loops proximal to the obstruction are noted, especially with obstructions occurring in the midduodenum or ileocecocolonic junction. Pneumoperitoneum indicates that the stomach has ruptured and carries a grave prognosis. Obtain blood for a complete blood count (CBC) and biochemical profile. Results may demonstrate dehydration and a variety of acid-base and electrolyte disorders.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree