Chapter 10 Musculoskeletal and Neurologic Diseases
Ferrets with neurologic, musculoskeletal, or systemic disease may present with rear limb weakness, ataxia/incoordination, or both. Primary neurologic and musculoskeletal disorders are not common in pet ferrets. Clinical signs that appear to be caused by primary neurologic disease, particularly posterior paresis, are frequently manifestations of systemic illness. Therefore a thorough and accurate history and physical examination supported by diagnostic imaging and laboratory testing are essential to establishing a diagnosis, treatment plan, and prognosis. Fracture management is covered in Chapter 33.
Neurologic signs in ferrets are often a result of generalized disease, such as heart failure or hypoglycemia. Thus a general health evaluation is important for all neurologic patients. A common cause of posterior paresis is hypoglycemia secondary to a pancreatic beta-cell tumor, or insulinoma (see Chapter 8). Hypoglycemia can also result from food deprivation or anorexia, vomiting, sepsis, neoplasia, severe hepatic disease, or any metabolic disorder.
Cardiac disease, hypoxia, anemia, and toxin ingestion can result in weakness, ataxia, or central nervous system (CNS) depression.5,42 Toxicosis from ibuprofen ingestion has been reported to cause neurologic signs including ataxia, depression, coma, and tremors.41 Clostridium botulinum type C endotoxin causes signs that include dysphagia, ataxia, salivation, and paresis 12 to 96 hours after ingestion of contaminated food; signs can progress to death if the ferret is untreated.11 Proliferative bowel disease has been associated with paresis and ataxia.14 This may also occur secondary to discomfort and physical obstruction of limb movement from diseases such as splenomegaly, a caudal abdominal mass, inguinal or sublumbar lymphadenopathy, cystic calculi, peritonitis, prostatic enlargement, or urinary obstruction. Urinary and fecal incontinence may accompany posterior paresis if the underlying problem affects the caudal lumbar innervation of these structures.
Posterior Paresis, Ataxia, and Seizures
Ataxia
Ataxia is incoordination; it can be characterized as either cerebellar, vestibular, or proprioceptive. Cerebellar ataxia is caused by a disruption in transmission of sensory impulses from the vestibular system, cerebral cortex, and spinal cord via the cerebellum. Because the cerebellum does not initiate motor activity but rather coordinates it, affected patients will demonstrate abnormal rate, range, or force of movement with intact strength. Paresis is not present with cerebellar dysfunction. Vestibular ataxia occurs when damage or disease affects the vestibular system within the inner ear. Motor activity is not initiated but is refined and coordinated via the vestibular system by controlling muscles used to maintain head position, eye movement, and equilibrium. Dysfunction results in loss of balance; animals often list or fall to one side and may have head tilt. Proprioceptive ataxia is caused by spinal disease, which will result in proprioceptive deficits that can be localized to the affected region of the spinal column. Trauma, intervertebral disk disease, and tumors arising within or compressing the spinal cord or nerves should be considered.35
Diagnosis of Posterior Paresis, Ataxia, and Seizures
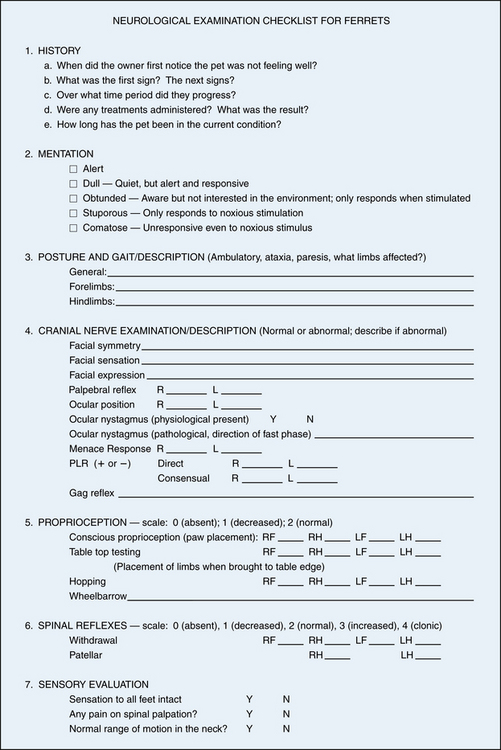
If you suspect primary neurologic disease, perform a complete neurologic and orthopedic examination35 (Fig. 10-1). Characterize the signs as diffuse or focal, acute or chronic, progressive or static; localize the lesion to areas of brain or spinal cord.27 Evaluate reflexes and palpate for spinal cord pain or hyperesthesia. Keep in mind during examination that the ocular menace response in ferrets is normally diminished or absent.
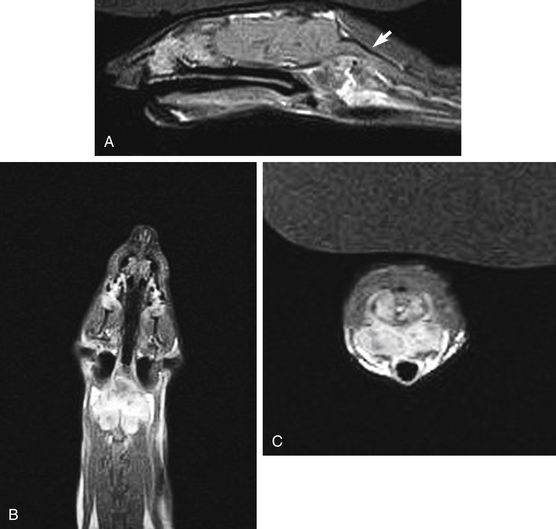
For signs that can be localized to the CNS, perform computed tomography (CT) or magnetic resonance imaging (MRI) if available. Administer an intravenous contrast medium to enhance brain lesions. For CT scanning, use 2.2 mL/kg of 400 mg/mL iodinated contrast medium (iothalamate sodium, Conray 400; Mallinckrodt Inc., St. Louis, MO); for MRI, use 0.2 mL/kg of gadolinium-diethylenetriamine pentaacetic acid (Gd-DTPA)49 (Fig. 10-2).
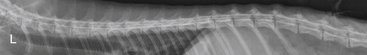
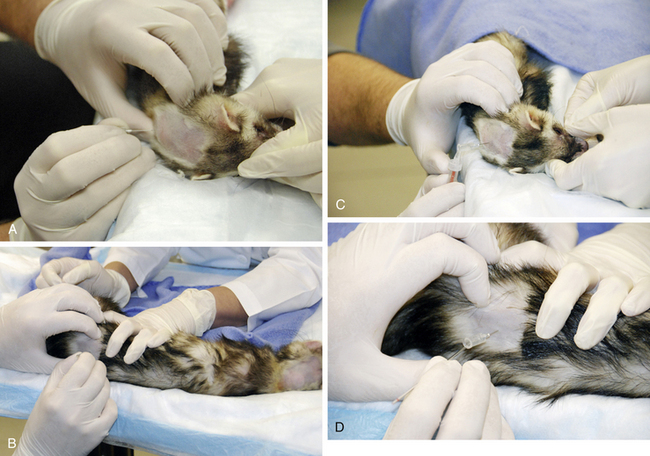
If signs are localized to the spinal column, take spinal radiographs to look for possible fractures or bone abnormalities, such as proliferative or lytic lesions. Myelography is useful for localizing lesions of the spinal cord and determining a site for surgical approach if needed (see Fig. 10-3). If possible, perform a spinal tap to obtain a sample of cerebrospinal fluid (CSF) for analysis. Sites for CSF tap and myelography are the atlanto-occipital and the lumbar (L5-L6) regions. Use a 25-gauge spinal needle, as in canine and feline myelography; a suggested contrast medium is iohexol at 0.25 to 0.5 mL/kg50 (Fig. 10-4). Reference values for CSF fluid analysis are total protein 28 to 68 μg/μL and nucleated cells 0 to 8/μL.37 Some spinal lesions may be amenable to surgical resection or stabilization; many, however, carry a poor prognosis.
For clinical signs localized to peripheral nerves or muscular defects, consult with a veterinary neurologist to perform electromyelography (EMG) and nerve conduction velocity (NCV) studies. Although normal values for ferrets have not been published, comparison of values from the contralateral limb (in unilateral disease) or from another, unaffected ferret will aid in interpreting the results. Tensilon testing (edrophonium HCL) and physostigmine testing can be performed in ferrets at standard canine doses (0.1 mg/kg IV).6,24,38,55 Obtain muscle biopsy samples in the same manner as in dogs and cats when indicated.
Treatment of Posterior Paresis, Ataxia, and Seizures
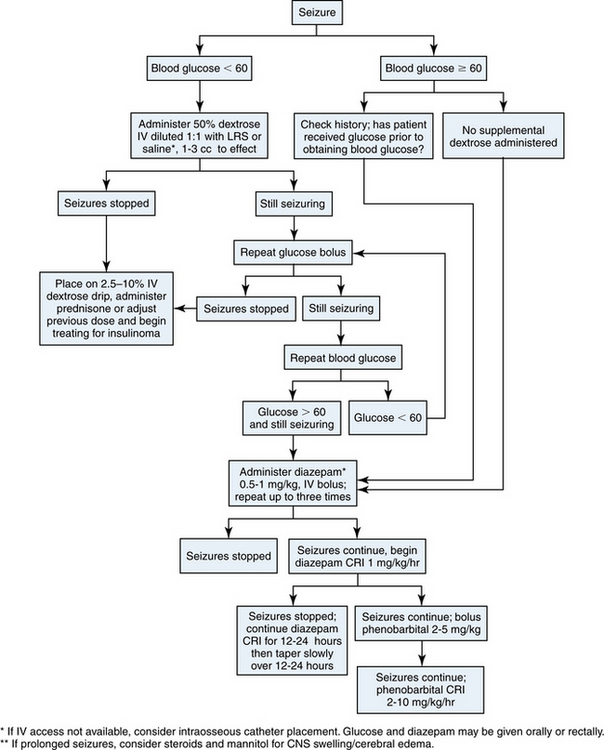
In any seizing ferret, the initial treatment must be directed toward arresting seizure activity (Fig. 10-5). Check the blood glucose concentration immediately in any animal presenting with seizures, ataxia, or other neurologic signs. If the glucose level is lower than 60 mg/dL, give an intravenous bolus of 50% dextrose solution (diluted 1:1 in crystalloid fluid) at a dose of 2 to 5 mL/kg or titrate to effect.10 Begin a dextrose drip infusion adequate to maintain normoglycemia while further diagnostic testing is done. Some ferrets require as much as 10% dextrose added to intravenous fluids to achieve normoglycemia. Administer prednisone or prednisolone to hypoglycemic patients to enhance hepatic gluconeogenesis and inhibit glycogenolysis. If an insulinoma is suspected, initiate additional therapy as indicated (see Chapter 8).
If seizures persist and the blood glucose concentration is normal (or has been restored to normal), begin aggressive seizure management. Administer diazepam (0.5-1.0 mg/kg) intravenously10,24,38; if venous access is not readily available, administer diazepam or midazolam intramuscularly, intranasally (for more rapid absorption), or rectally. Double the dose for rectal or nasal administration.24 Repeat up to three times to arrest seizure activity. If grand mal or focal seizures persist, begin a constant-rate infusion of diazepam (0.1-1.0 mg/kg per hour added to IV fluids) or initiate phenobarbital (2-10 mg/kg per hour) as a constant rate infusion.38 Phenobarbital can also be administered by bolus; use 3 mg/kg slow IV q30-60min up to a total dose of 18 to 24 mg/kg, then 3 to 5 mg/kg q12h.24 Phenobarbital and diazepam can be administered concurrently.38 Propofol can also be added; administer in aliquots of 2 mg/kg to effect, then 6 mg/kg per hour CRI to effect.24 If cerebral edema is suspected, administer dexamethasone (0.2 mg/kg) or prednisone or prednisolone (1 mg/kg IV) and mannitol (0.5-1.0 g/kg IV over 20 minutes).36,38 Once no seizures have occurred for 12 to 24 hours, taper the diazepam infusion slowly over the next 12 to 24 hours. Once seizures are controlled, use oral phenobarbital (1-2 mg/kg PO q8-12h) if necessary for long-term seizure management.38 Potassium bromide can also be used for seizure control; administer orally at 70 to 80 mg/kg per day if used alone or at 22 to 30 mg/kg per day in combination with phenobarbital.38 Check blood levels of phenobarbital within 2 to 3 weeks after starting therapy; potassium bromide levels may not reach a steady state for 60 to 90 days. Adjust dosages based on blood levels and clinical signs. The use of gabapetin, zonisamide, or levetiracetam has not been described in ferrets to date. Investigate any underlying disease stimulating the seizure activity after the patient is stable.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree