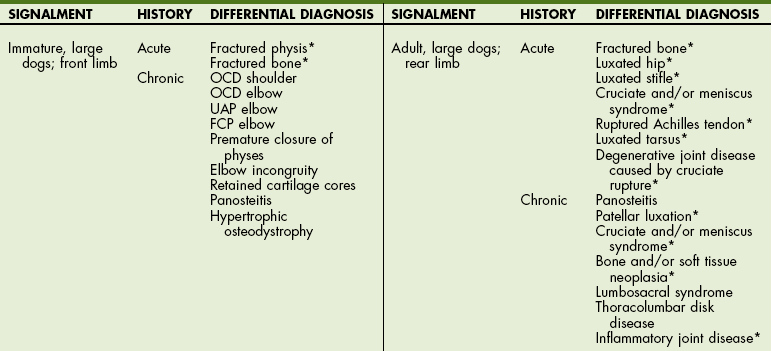
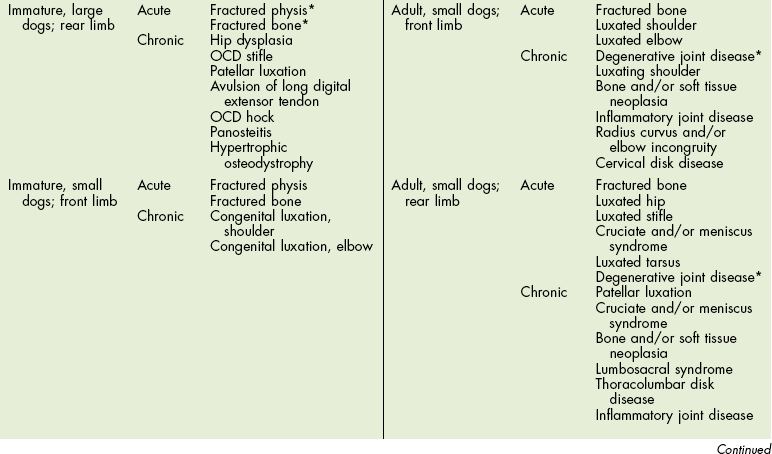
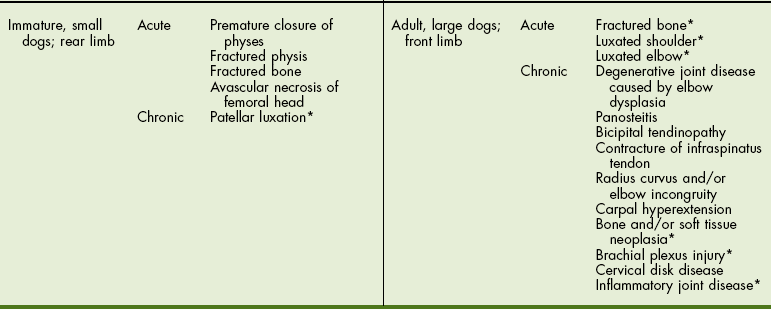
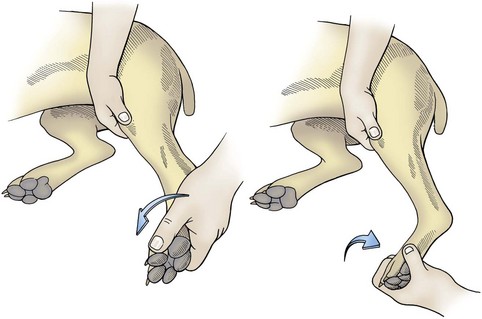
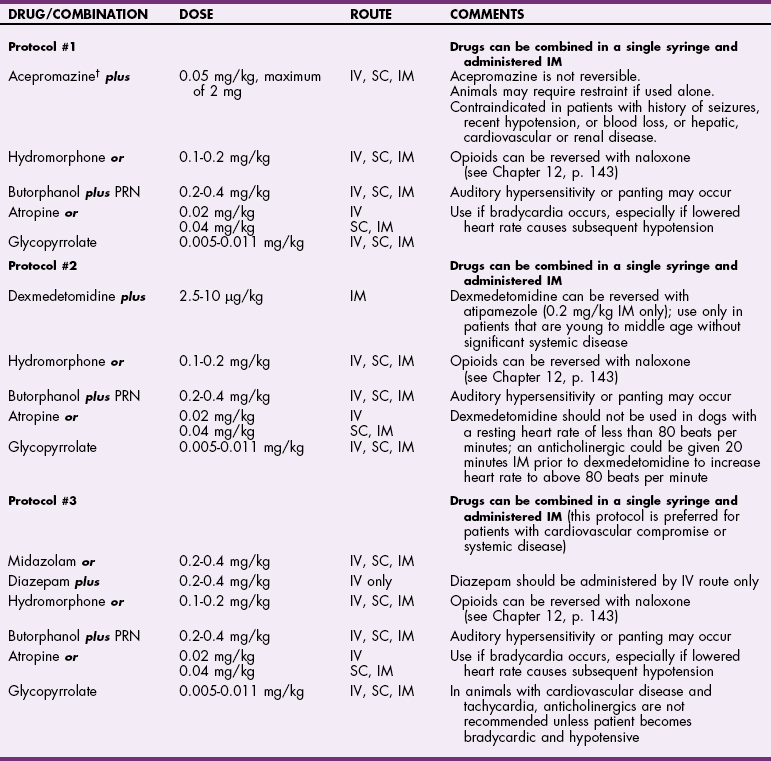
Chapter 32 General Principles and Techniques Unique terms used in orthopedic surgery include descriptions of examination and reduction maneuvers, classification of fractures and fracture healing, types of grafting material, and surgical outcomes. A partial list of definitions is provided in Box 32-1. Other terms are described in the text of this chapter. A differential diagnosis is developed based on results of history, signalment, and physical examination. Other tests or procedures may be necessary to define the disease once the aforementioned findings have narrowed the diagnostic possibilities. Many orthopedic diseases are predictable within certain age groups and breeds (Table 32-1). Information on the animal’s general condition includes anorexia, depression or fever, limb affected, multiple limb involvement, degree of pain or lameness, duration, intensity of onset, historical trauma, effect of exercise, time of day of greatest clinical signs, effect of rest, and changes in lameness associated with weather. Such information provides initial clues to form a differential list of potential causes. Additional questioning, physical examination, and imaging will usually provide data to make a definitive diagnosis. The animal’s general health should be assessed as part of the physical examination. Baseline examination includes obtaining the animal’s temperature, pulse, and respiration. The animal’s overall appearance should be noted (e.g., obesity) and thoracic auscultation and abdominal palpation performed. A general health evaluation is important before anesthetizing any animal that has orthopedic disease. Traumatized animals brought in for fracture evaluation should have thoracic radiographs and serial electrocardiograms (ECGs) performed. Evaluation of the abdominal cavity is done initially with palpation and evaluation of serum chemistry tests. Abdominocentesis (see p. 380) and radiographic or ultrasonographic evaluation of the urinary tract (see p. 757) should be performed if clinical signs suggest injury. Traumatized animals with long bone fractures frequently have concurrent soft tissue injuries (e.g., pneumothorax, traumatic myocarditis, diaphragmatic hernia, and ruptured bladder or urethra). It is crucial to diagnose and treat these injuries before the animal is anesthetized for fracture repair. After the lame limb has been identified, the animal should be returned to the examination room. Limb palpation and a screening neurologic examination should be performed simultaneously. Optimally the first examination should be done without sedation to determine the animal’s response to pain; however, this may not be possible in aggressive animals. The examiner should develop a consistent evaluation pattern. One technique is to start at the front of the animal and work toward the rear. Also, starting at the toes of each limb and progressing proximally is useful. It is preferable to begin examining a sound limb to identify the individual’s normal response to manipulation and pressure. The initial examination should be done with the animal standing to assess muscular symmetry, joint enlargement, and proprioceptive responses. As each bone, joint, and soft tissue area is palpated, any asymmetry (between limbs), response to pain, swelling, abnormalities in range of motion, instability, and crepitation should be noted. Asymmetry should be assessed before and during individual limb palpation and may indicate tumor, abscess, atrophy, joint swelling, or greenstick fracture. Long bones should be palpated to determine if there is swelling (e.g., fracture or tumor), a response to pain while firm pressure is applied (e.g., panosteitis, fracture, or tumor), instability, or crepitation (e.g., fracture). Joints should be isolated and moved through a complete range of motion to detect crepitation, pain, or abnormalities in range of motion. Additional tests of shoulder, hip, and stifle instability should be performed if abnormalities are detected in these joints (see p. 1039 [shoulder], p. 1041 [hip], and p. 1040 [stifle]). Muscles and tendons should be palpated to determine if they are normal and intact. After the initial orthopedic examination to localize pain, the animal may be sedated to facilitate closer examination and to obtain radiographs (Tables 32-2 and 32-3). Sedation for Palpation and Radiographs of Dogs* IV, Intravenous; SC, subcutaneous; IM, intramuscular. *Animals receiving sedatives should be carefully monitored. Parameters including (but not limited to) respiratory rate, heart rate, and pulse oximetry should be monitored regularly. Blood pressure should be checked when blood pressure changes are anticipated. Temperature should be monitored if the animal is sedated for longer than 30 minutes. †Acepromazine (0.05 mg/kg IM or SC; maximum of 2 mg) may be used alone for radiographs and palpation; however, it provides minimal restraint. Protocols courtesy Dr. Stuart Clark-Price. Sedation for Palpation and Radiographs of Cats* IV, Intravenous; SC, subcutaneous; IM, intramuscular. *Animals receiving sedatives should be carefully monitored. Parameters including (but not limited to) respiratory rate, heart rate, and pulse oximetry should be monitored regularly. Blood pressure should be checked when blood pressure changes are anticipated. Temperature should be monitored if the animal is sedated for longer than 30 minutes. †Acepromazine (0.05 mg/kg IM or SC; maximum of 2 mg) may be used alone for radiographs and palpation; however, it provides minimal restraint. Protocols courtesy Dr. Stuart Clark-Price. A complete orthopedic examination of the forelimb includes the following manipulations. Palpate the elbow for fluctuant swelling in the space between the lateral condyle and olecranon and over the medial coronoid process. Fluctuant swelling indicates joint effusion, which results from several elbow diseases. Joint effusion may be more easily detected when the animal is standing. Firm, generalized swelling of the elbow often indicates degenerative joint disease. Flex and extend the elbow (Figs. 32-1 and 32-2). FIG 32-1 Flex and extend the elbow. Notice the angle of greatest flexion of a normal elbow measured with a goniometer. The carpus should almost touch the shoulder. Compare this with the angle of flexion in an elbow with degenerative joint disease (see Fig. 32-2). FIG 32-2 Angle of greatest flexion of elbow in dog with degenerative joint disease. Compare this with the angle of flexion in a normal elbow (see Fig. 32-1). Swelling from joint effusion is difficult to detect in the shoulder because of the overlying muscles. Move the shoulder through a range of motion, including hyperextension and hyperflexion, while stabilizing the scapula (Fig. 32-3). Dogs with osteochondritis dissecans of the humeral head often show a pain response when the shoulder is hyperextended. Palpate the biceps tendon and apply pressure; a painful response may indicate a biceps tendinopathy. Complete orthopedic examination of the rear limb involves various manipulations. Palpate the tarsal joints for fluctuant swelling indicative of joint effusion. This may be a subtle finding in the hock and is more easily noted when the animal is standing because loading the joint forces the fluid peripherally. Firm swelling suggests degenerative joint disease. Extend and flex the hock. Normal flexion should be about 40 to 45 degrees. Decreased flexion indicates degenerative joint disease, which may be secondary to osteochondritis dissecans. Pain on manipulation of the joint (especially coupled with soft tissue swelling) may indicate a fracture. Simultaneously, extend and adduct or abduct the hock and metatarsal bones to demonstrate instability of the collateral ligaments. With the stifle in extension and the hock stressed into flexion, palpate the Achilles tendon (Fig. 32-4). Rupture of the entire tendon complex allows hock flexion while the stifle is extended. Rupture of the gastrocnemius tendon and common tendon of the biceps femoris, gracilis, and semitendinosus muscles, with preservation of the superficial digital flexor, allows partial flexion of the hock while the stifle is extended and causes simultaneous flexion of the digits. Extend and flex the stifle while holding one hand over the cranial aspect of the joint to detect crepitation. Next examine the stability of the patella in relationship to the femur. Extend the stifle, internally rotate the foot, and apply digital pressure in an attempt to displace the patella medially (medial patellar luxation). Detect lateral patellar luxation by slightly flexing the stifle, externally rotating the foot, and applying digital pressure to attempt to displace the patella laterally (Fig. 32-5). The patella normally moves slightly medially and laterally but is considered to be luxating when it leaves the trochlear groove. Hold the stifle in full extension and simultaneously attempt to open the stifle on the medial and lateral aspects to assess the integrity of the collateral ligaments. Test the medial collateral ligament by using one hand to brace the femur while the other hand abducts the tibia. Normally the medial collateral ligament will not allow joint laxity. Test the lateral collateral ligament by bracing the femur with one hand and using the other hand to adduct the tibia (Fig. 32-6). An intact lateral collateral ligament will prevent joint laxity. If the stifle is allowed to flex while the tibia is adducted, it may feel as though there is lateral laxity of the joint. This is a result of anatomic location of the lateral collateral ligament and internal rotation of the tibia and is normal. Test the integrity of the cruciate ligaments by trying to elicit a cranial or caudal drawer motion or by performing a tibial compression test to elicit cranial tibial thrust. Drawer movement is caused by the tibia sliding cranially or caudally in relationship to the femur. This motion is not possible when the cruciate ligaments are intact in adult animals. Immature animals may have slight drawer motion, but it stops abruptly as the ligament tightens. To elicit direct drawer motion, place the index finger and thumb of one hand over the patella and lateral fabellar regions, respectively. Place the index finger of the opposite hand on the tibial tuberosity, and with the thumb positioned caudal to the fibular head, slightly flex the stifle. Stabilize the femur, and gently move the tibia cranial and distal to the femur. Do not allow tibial rotation. Tense muscles may prevent drawer motion. If tibial rotation occurs, gently flex and extend the stifle to relax the animal, and repeat the procedure. Test drawer motion with the femur flexed and extended (Fig. 32-7). Usually the greatest movement is felt with the stifle in flexion. If the patella is luxated, replace it in the trochlear groove before attempting the drawer motion. Perform the tibial compression test to detect cranial tibial thrust. Detect forward motion of the tibia by placing the index finger along the patella and the tibial tuberosity. With the leg in a standing position, flex the hock to tense the gastrocnemius muscle (Fig. 32-8). This compresses the femur and tibia together, causing the tibia to move forward in a cranial cruciate-deficient stifle. The presence and amount of drawer motion depend on the animal’s age, size, state of relaxation, and the duration and type of cruciate pathology. There is minimal drawer motion in normal dogs and cats, although very young puppies may have a “lax” stifle. Sedation or general anesthesia increases the likelihood of a positive drawer sign in dogs with cranial cruciate rupture. Minimal drawer motion may be noted with chronic cruciate pathology (especially in large dogs) because periarticular fibrosis restricts stifle motion. Minimal or partial drawer motion may also occur with incomplete tears or stretching of the cranial cruciate ligament. Drawer motion is also evident with a torn caudal cruciate ligament. To identify caudal drawer motion, start with the stifle in a neutral position. Most caudal ligament ruptures are not discovered until exploration because they are mistaken for cranial ligament injuries. To detect luxation of the hip, use the position of the greater trochanter in relationship to the tuber ischium as a landmark. In the standing animal, compare the distance from the greater trochanter with the tuber ischium bilaterally. A unilateral increase in the distance indicates hip luxation. Animals with acute hip luxations are not weight bearing and may have swelling over the greater trochanter. Externally rotate the femur while placing the thumb in the space between the greater trochanter; the thumb should become displaced (Fig. 32-9, A and B). With hip luxation, the trochanter rolls over the thumb (Fig. 32-9, C and D). With the animal in lateral recumbency, perform the Ortolani maneuver to detect hip laxity associated with hip dysplasia. Place one hand over the dorsal pelvis. Grasp the stifle with the other hand, and orient the femur parallel with the table surface. Simultaneously adduct and push the stifle toward the pelvis. Maintain the pressure and abduct the stifle. As the femoral head returns to the acetabulum, use the hand stabilizing the pelvis to detect a click (Fig. 32-10). The Ortolani maneuver can also be performed with the animal in dorsal recumbency, with the stifles held parallel to each other and perpendicular to the table. Apply downward pressure on the stifle to subluxate the hip. Maintain pressure and abduct the stifle. With both procedures, a click is noted as the femoral head returns to the acetabulum in a subluxated hip (Fig. 32-11). The angle of subluxation is the point at which the hip subluxates, and the angle of reduction is the point at which the femoral head returns to the acetabulum. Evaluation of hip laxity is best done with the dog sedated or anesthetized. Because neurologic disorders may mimic orthopedic diseases or may occur concurrently, every orthopedic examination should include several neurologic examination maneuvers performed to screen for neurologic disease. If evidence of neurologic disease is discovered, a complete neurologic examination is indicated (see Chapter 38). Evaluate conscious proprioception in all four limbs by gently supporting the animal and individually turning each paw until the dorsal surface of the paw contacts the ground. Normal animals return the paw to the correct position almost immediately. Loss of conscious proprioception usually indicates neurologic disease; however, animals with fractured limbs may be reluctant to move the limb and therefore may appear to have conscious proprioception deficits. Flex and extend the neck and bend it laterally in both directions. Apply direct pressure on the lateral processes of the sixth cervical vertebra. Animals may exhibit a forelimb lameness associated with cervical nerve root pain (root signature sign), and it is important to rule out cervical disease or nerve root tumors. Apply direct pressure on the thoracolumbar spine while supporting the abdomen. A painful response, exhibited by vocalization, flinching, or tightening the abdominal musculature may indicate thoracolumbar spinal disease. Apply direct pressure on the ventral lumbar musculature to isolate lumbosacral pain (Fig. 32-12). A differential diagnosis is developed based on results of history, signalment, and physical examination. Definitive diagnoses may require additional diagnostic tools including imaging, hematology, serum biochemistry, cytology, or electrodiagnostics. Radiography is generally the initial imaging modality employed to arrive at a definitive diagnosis; however computed tomography, magnetic resonance imaging, ultrasonography, and scintigraphy may be indicated for diagnosis and/or improved visualization of some problems (Table 32-4). Joint taps are useful for differentiating degenerative and inflammatory disease (see p. 1217). Fine needle aspirates or biopsies are essential for diagnosing neoplastic disease (see p. 1398). Imaging Modalities for Orthopedic Problems 1, Imaging modality used for primary evaluation; 2, imaging modality used for additional evaluation. Carobbi, B, Ness, MG. Preliminary study evaluating tests used to diagnose canine cranial cruciate ligament failure. J Small Anim Pract. 2009;50:224–226. Cook, JL, Renfro, DC, Tomlinson, JL, Sorensen, JE. Measurement of angles of abduction for diagnosis of shoulder instability in dogs using goniometry and digital image analysis. Veterinary Surgery. 2005;34:463–468. Devitt, CM, Neely, MR, Vanvechten, BJ. Relationship of physical examination test of shoulder instability to arthroscopic findings in dogs. Vet Surg. 2007;36:661–668. Perioperative Patient Management Perioperative management of surgical patients is discussed in detail in Chapter 4. Orthopedic patients may be brought in for elective surgery (e.g., cranial cruciate ligament injury, hip dysplasia, and osteochondritis dissecans), or nonelective surgery (e.g., bone fractures and joint luxations). When animals are brought in for elective surgery, there is ample time to perform an appropriate preoperative diagnostic evaluation. Younger patients (less than 5 to 7 years old) should have selected screening laboratory tests, including packed-cell volume (PCV), and serum total solids. Urinalysis, fecal analysis, and heartworm tests may be indicated, depending on the history and the animal’s geographic location. The need for further laboratory evaluation should be based on signalment, physical examination, and results of initial screening tests. Orthopedic patients benefit from perioperative analgesics (Table 32-5). The projected level of postoperative discomfort and the duration of discomfort should be assessed to determine the choice of preoperative analgesic. Most orthopedic surgeries are considered moderately to severely painful. Although there is much debate concerning preemptive analgesia, especially in the human medical literature, there are several principles that must be followed in order for preemptive analgesia to be successful. First, the depth of analgesia must be sufficient to block pain receptors during surgery. Second, nociceptive receptors from the entire field must be blocked. And last, analgesia must be continued in the postoperative period (see Chapter 12). Anesthetic Considerations in the Stable Patient Undergoing Fracture Repair *Monitor for hyperthermia in cats. †Buprenorphine is a better analgesic than morphine in cats. ‡Black box warning added by the FDA in October 2010 identified cases of renal failure and death in cats with repeated uses of meloxicam. Meloxicam is approved for single use only in cats in the United States. Anesthetic protocols should be chosen based on signalment, physical examination findings, and laboratory analysis. Patients treated for elective orthopedic problems (e.g., cruciate reconstruction) and who have no preoperative findings suggestive of major organ dysfunction can be managed using a variety of anesthetic techniques (see Table 32-5). Patients with cardiovascular compromise or trauma should be anesthetized with care (Table 32-6). When appropriate, balanced anesthetic protocols that include analgesic agents supplemented with epidural analgesia are recommended to decrease intraoperative pain response and reduce the amount of anesthetic needed (Tables 32-7 and 32-8). Epidural anesthesia (with lidocaine, bupivacaine, or ropivacaine) in combination with general anesthesia provides profound relaxation by temporarily paralyzing rear limb muscles, easing fracture reduction of the pelvis, femur, and tibia (see Chapter 12). The duration of action depends on the drug used, ranging from 1 to 6 hours. Fentanyl, morphine or buprenorphine can be added to the epidural injection, providing postoperative pain relief for up to 24 hours. Additionally, opioids may be used alone in the epidural space when relaxation of muscles is not warranted but postoperative analgesia is desired. A brachial plexus block using local anesthetics will provide additional analgesia and muscle relaxation in patients undergoing surgery of the forelimb.
Fundamentals of Orthopedic Surgery and Fracture Management
Definitions
Differential Diagnosis
Orthopedic Examination
Orthopedic Examination
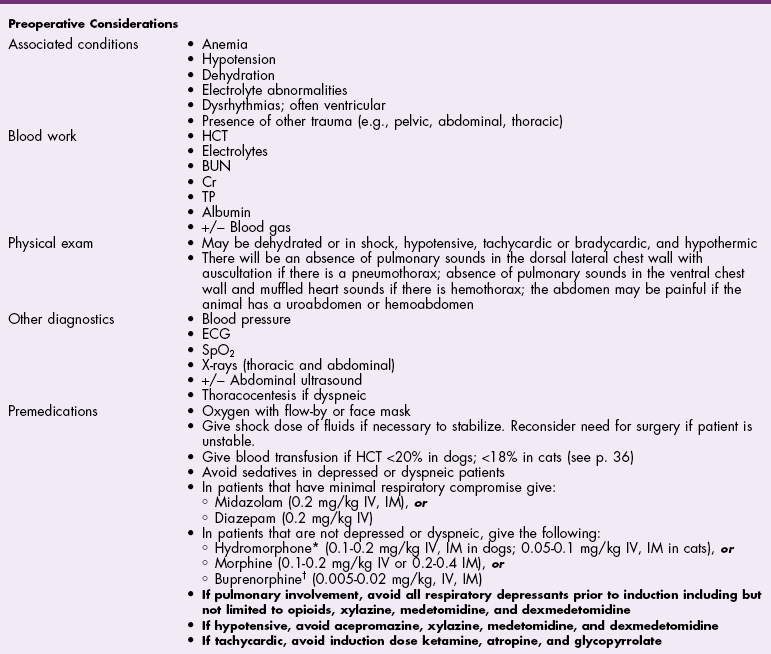
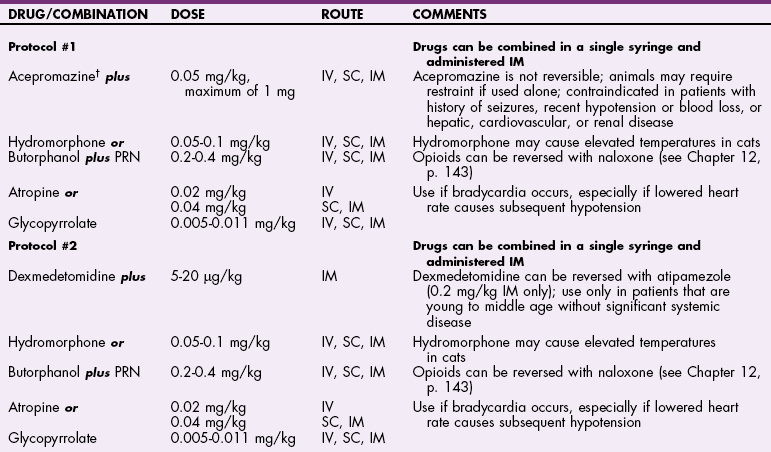
![]() TABLE 32-2
TABLE 32-2
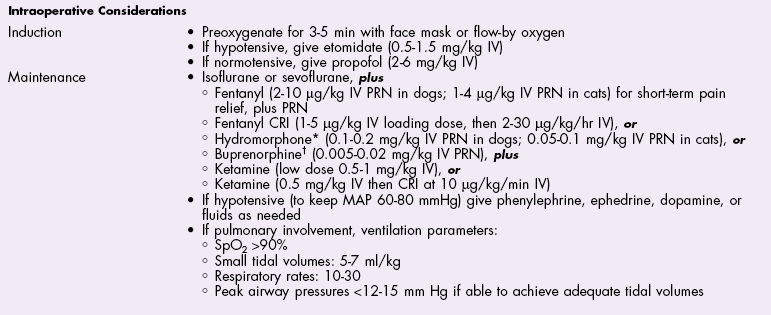
![]() TABLE 32-3
TABLE 32-3
Forelimb
Elbow


Shoulder
Rear Limb
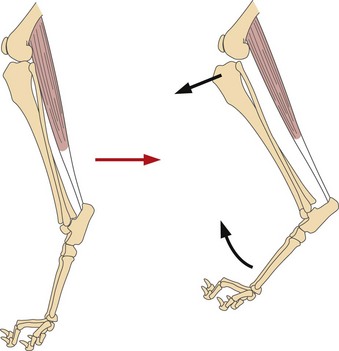
Hock
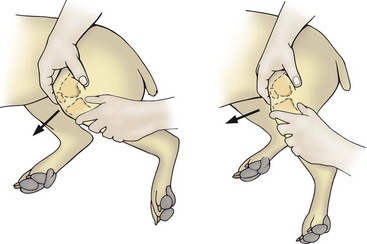
Patella
Collateral ligaments
Cruciate ligaments
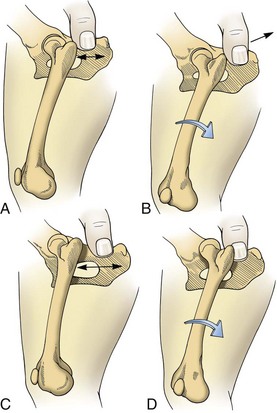
Hip luxation
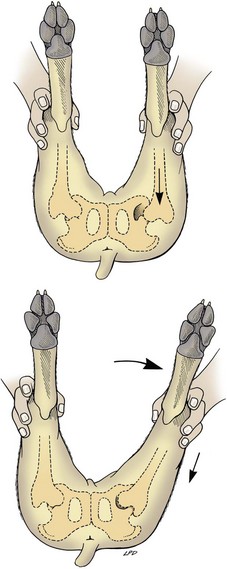
Hip laxity
Rule Out Neurologic Disease
Additional Diagnostic Techniques
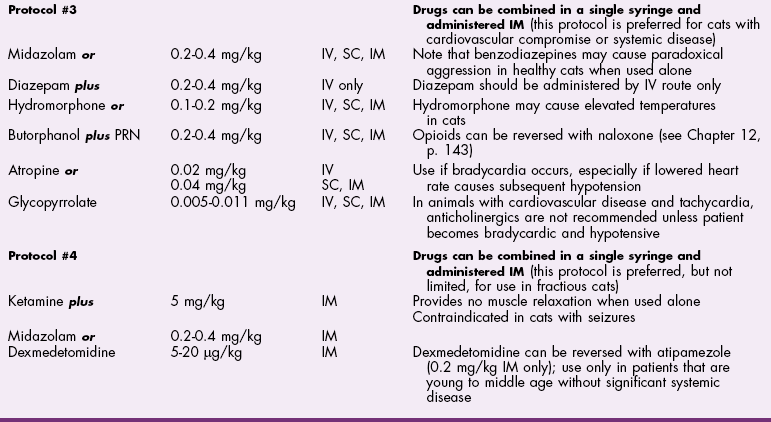
![]() TABLE 32-4
TABLE 32-4
Preoperative Management
Pain Management and Anesthesia
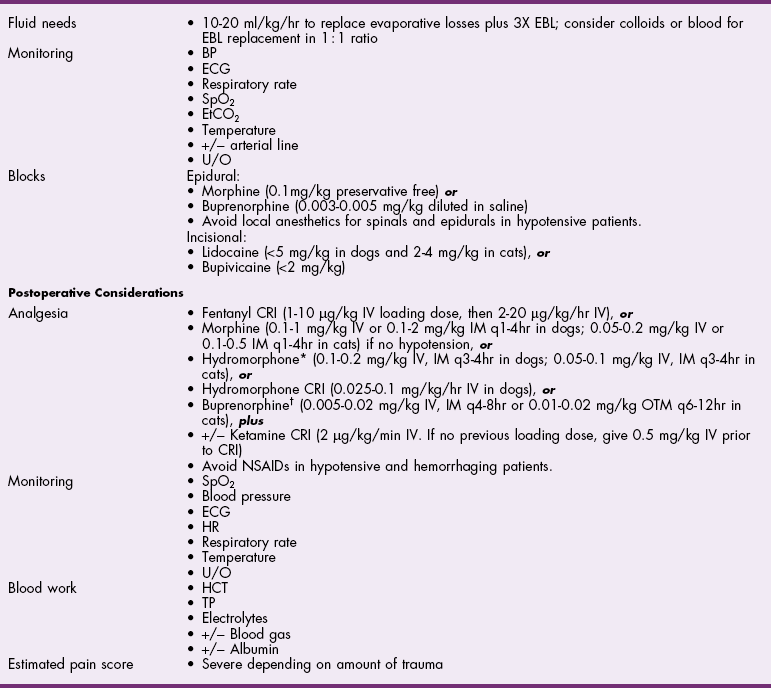
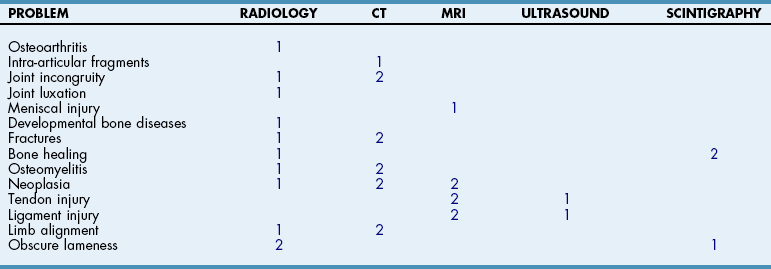
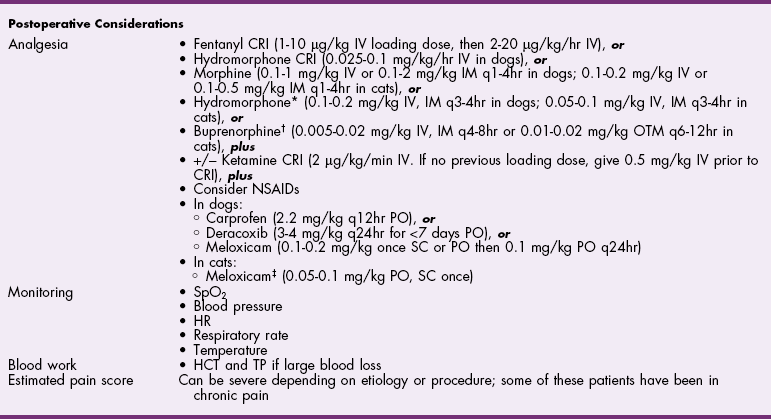
![]() TABLE 32-5
TABLE 32-5
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Fundamentals of Orthopedic Surgery and Fracture Management