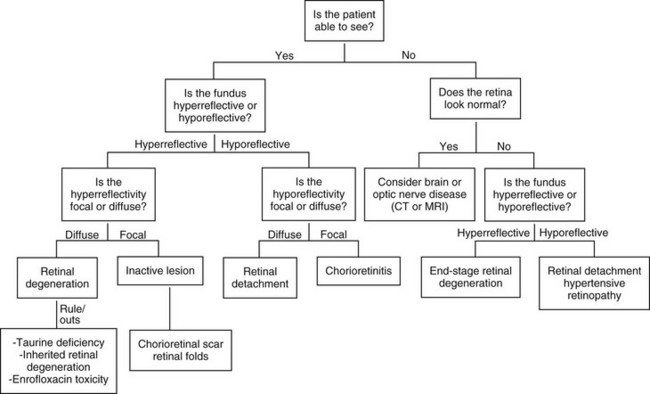
Chapter 255 Examination of the feline retina is an important part of a thorough systemic evaluation. Any cat with a pupillary abnormality, a presenting complaint of vision loss, a systemic illness of unknown origin, or a cardiac abnormality should undergo a complete retinal examination. Proper retinal evaluation can help the practitioner to focus the diagnostic search as well as monitor response to therapy. This chapter reviews the most common causes of retinal lesions in the feline and presents a diagnostic approach to retinal changes. Figure 255-1 provides a diagnostic algorithm for feline retinal disease. The incidence of ocular signs in hypertensive cats is about 40% to 60%, and ocular signs are the most common form of target organ dysfunction associated with systemic hypertension. Hypertensive retinopathy is identified most often in cats older than 10 years of age with systolic blood pressures greater than 168 mm Hg when measured by an oscillometric technique (Sansom et al, 2004). The presence of ocular changes is an indication to start antihypertensive therapy even if blood pressure measurements do not consistently meet the criteria for hypertension. Treatment of hypertensive retinopathy is focused solely on control of the systemic hypertension. No topical medications are indicated to treat the ocular component. Amlodipine has been demonstrated to be particularly effective in the resolution of systemic hypertension and hypertensive retinopathy (Maggio et al, 2000). Current recommendations for the treatment of systemic hypertension can be found in Chapter 169, but cats with hypertensive retinopathy should be evaluated for underlying systemic disease, including renal failure, hyperthyroidism, and the more uncommon condition of hyperaldosteronism (Conn’s syndrome).
Feline Retinopathies
Hypertensive Retinopathy
Treatment and Prognosis
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree