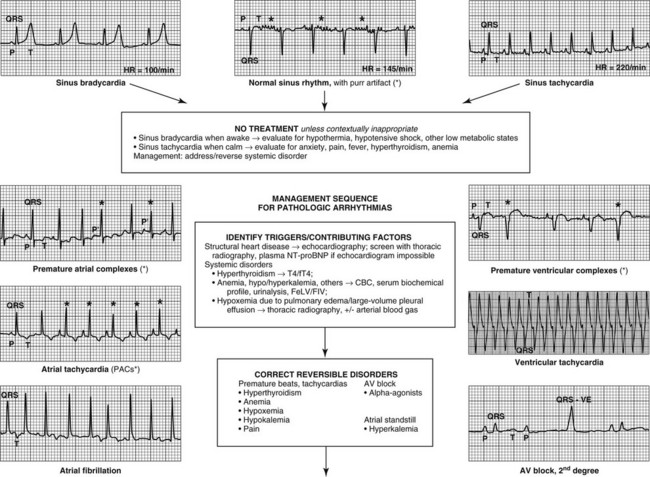
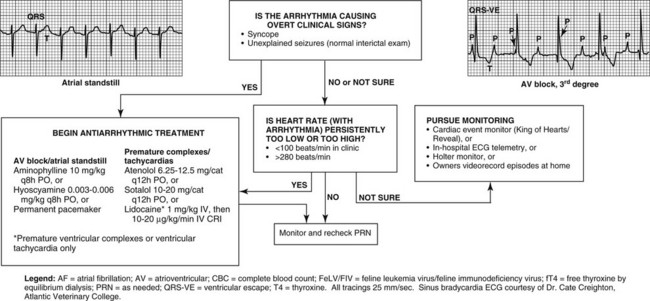
Chapter 173 The presence or absence of structural heart disease is not suspected reliably from physical examination findings alone: depending on the criteria used, as few as 18% of cats with heart murmurs have evidence of left ventricular concentric hypertrophy on an echocardiogram (Paige et al, 2009; Wagner et al, 2010). The suspicion of structural heart disease may be increased or decreased by the results of thoracic radiography with or without N-terminal prohormone B-type natriuretic peptide testing (Côté et al, 2011b, 2011c; Ettinger, 2010; Fox et al, 2011), and confirmation requires echocardiography. Reversible contributing factors to an arrhythmia are identified through routine laboratory tests. For example, hypokalemia, anemia, and hypoxemia can induce premature ventricular complexes and potentially render these refractory to antiarrhythmic treatment (Côté et al, 2011a). Such abnormalities may be identified or suspected via basic clinical testing (Figure 173-1). Figure 173-1 Examples of feline electrocardiograms and a management approach to feline cardiac arrhythmias. The presence or absence of syncope is described by the owner; however, many owners cannot recognize the features of syncope. Since some cats produce subtle signs that could be explained either by syncope or by such nonsyncopal disorders as behavioral or metabolic disturbances, obtaining information during an episode can be enormously helpful. Owners may be instructed to record episodes on video at home for review by the veterinarian or to record an ECG during an episode via Holter or event monitoring. The information obtained is especially valuable when episodes are infrequent or ambiguous in their expression. It is also important to recognize that cats with syncope often are misdiagnosed with a seizure disorder because facial twitching and tonic-clonic motion are common signs of feline syncope. In feline medicine, it remains unresolved whether cats with clinical signs caused by bradyarrhythmias have cerebral hypoxia leading to an epileptic focus and true seizure activity or whether physical manifestations of syncope closely resemble seizure activity (Penning et al, 2009). Normal sinus rhythm in the cat is evident when spontaneous automaticity in the sinoatrial node produces a heart rate of 110 to 180 beats/min. Each atrial depolarization leads to a ventricular depolarization. Therefore, on the ECG, each P wave is followed by a QRS complex at a fixed PR interval. The R-R interval is unchanging and thus the rate is constant, or if it changes, it does so gradually over a few heartbeats, not immediately from one beat to the next. These features are identical in sinus tachycardia, the equivalent of normal sinus rhythm but with a rate of more than 180 beats/min in cats (see Figure 173-1). A number of key points can be made regarding sinus tachycardia in cats: • Sinus tachycardia is the cardiac rhythm expected in essentially all cats in the clinical setting (Côté et al, 2011a) because of anxiety and arousal. A heart rate of less than 160 beats/min on physical examination during an appointment should trigger a suspicion of relative bradycardia. An ECG is then warranted to rule out a pathologic bradycardia like second- or third-degree atrioventricular (AV) block. • QRS complexes in normal feline ECGs may be positive or negative because of the wide normal range of the mean electrical axis of the feline ventricles. • QRS complexes in normal feline ECGs may be very small, and no minimum limit of normal has been recognized for the height of the R wave in the cat in lead II. It may seem paradoxical that diseased heart tissue tends to fire more than normal, not less. The paradox is clarified by contrasting normal and abnormal cardiac cells. Healthy cardiomyocytes maintain a stable, inactivated state until triggered to depolarize, like dominos in a tumbling series, by each heartbeat’s advancing wave of normal electrical activity. Disruption of myocardial tissue interferes with this organized, sequential pattern of cardiac depolarization. In cats, myocyte stretch and myocardial interstitial fibrosis, in particular, are common atrial lesions that are associated with such disruptions (Boyden et al, 1984). These alterations render a cell less stable and more prone to depolarizing inappropriately. To continue the analogy, a single domino topples out in the periphery, creating a rogue heartbeat (ectopy) that propagates outward and commands the rhythm of the heart for that beat. A premature depolarization may not occur if it begins too prematurely, when the adjacent myocardium is refractory because all the dominos have tumbled and have not yet been prepared for the next tumble (i.e., have not yet repolarized). This concept of premature depolarization applies to all chambers of the heart. In humans, these arrhythmias involve various substrates and mechanisms, like the origin of atrial fibrillation from the pulmonary venous-atrial junction, but these mechanisms have not been investigated in vivo in the cat. In the atria of cats, premature, spontaneous atrial depolarizations may occur singly (premature atrial complexes or PACs; synonyms include atrial premature complexes, atrial premature contractions, and premature atrial depolarizations), in a series of four or more from the same focus in the atrium (atrial tachycardia or AT), or as a series of chaotic, seemingly randomly generated atrial impulses (atrial fibrillation or AF) (see Figure 173-1). The ECG characteristics of these rhythms can be summarized as follows: • PACs: Shorter R-R interval (i.e., the heartbeat occurs prematurely), with the P wave of the PAC (called P′ or P-prime) often superimposed on the normal T wave of the preceding beat. The morphology of the QRS complex is identical or nearly identical to that of a normal sinus QRS complex. The next sinus beat generally occurs at an interval that is not in phase with the expected timing of normal sinus rhythm had the PAC not occurred. This creates a noncompensatory pause following the PAC, which suggests that the PAC penetrated and reset the sinoatrial nodal cycle. • AT: As described for PACs, but consisting of four or more consecutive PACs. The QRS following the initial PAC of the sequence occasionally may be different in morphology owing to abnormal ventricular conduction (aberrancy). • AF: Absence of P waves in all ECG leads. The morphology of the QRS complex is identical or nearly identical to that of the normal sinus QRS complex, often with subtle variation in the QRS complexes. Fine baseline undulations (atrial fibrillation waves) are seen. The rhythm is irregularly irregular; that is, the R-R interval has no discernible consistency or pattern through the ECG tracing. The prognosis for cats with PACs, AT, or AF is governed by the underlying cause. These three arrhythmias do not appear to confer a prognosis that is better or worse than the prognosis associated with the cat’s underlying structural heart disease (Atkins et al, 2001).
Feline Cardiac Arrhythmias
Sinus Tachycardia
Particularities in Cats
Premature Atrial Complexes, Atrial Tachycardia, and Atrial Fibrillation
Treatment
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 of a 0.125-mg tablet every 48 hours PO and is preferred to the pediatric elixir, which many cats dislike. A β-blocker, or alternatively diltiazem, may be added if rate control is insufficient with digoxin alone. Diltiazem is dosed at 1 mg/kg every 8 hours PO, although current tablet sizes make this more difficult, and typically
of a 0.125-mg tablet every 48 hours PO and is preferred to the pediatric elixir, which many cats dislike. A β-blocker, or alternatively diltiazem, may be added if rate control is insufficient with digoxin alone. Diltiazem is dosed at 1 mg/kg every 8 hours PO, although current tablet sizes make this more difficult, and typically  of a 30-mg tablet per cat is given; extended-release versions also are available and typically are dosed at 15 mg per cat every 12 hours PO, although adverse gastrointestinal and hepatobiliary effects, and unpredictable pharmacokinetic effects, make these versions undesirable in the cat.
of a 30-mg tablet per cat is given; extended-release versions also are available and typically are dosed at 15 mg per cat every 12 hours PO, although adverse gastrointestinal and hepatobiliary effects, and unpredictable pharmacokinetic effects, make these versions undesirable in the cat.