Chapter 13 Endoscopic Knot Tying and Suturing
Endoscopic suturing is not difficult and expands the capabilities of the laparoscopic surgeon, enabling more difficult procedures to be performed without conversion to open or laparoscopically assisted surgery. This chapter will focus on the indications for endoscopic knot tying and suturing and 10 practice tips for surgeons to successfully accomplish endoscopic suturing. An in-depth discussion of endoscopic suturing and knot tying can be found in another text.1 Step-by-step instructions for specific techniques are included on the companion website.
www.tamssmallanimalendoscopy.com
Practice Tip 1: Commit to Learning
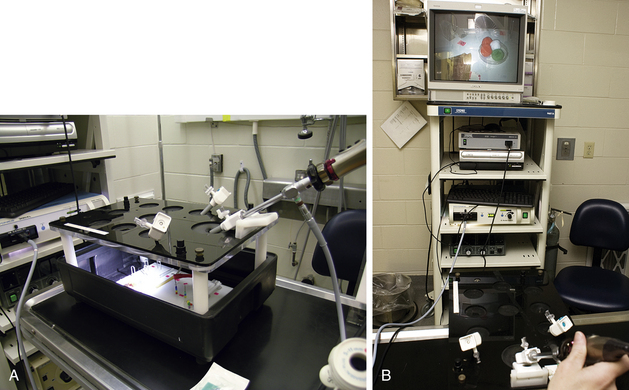
Endoscopic suturing presents challenges similar to microscopic suturing and thus requires diligence to master. The operating environment presents unique challenges that must be overcome. The field of view is smaller than with open surgery, there is loss of three-dimensional viewing, points for instrument insertion are fixed, and the surgeon is working with less familiar equipment. These challenges can be overcome by employing the techniques presented in this chapter and developing experience with your surgical team in performing minimally invasive procedures. Properly positioning the instrument ports, taking advantage of the technology to magnify the surgical field, and utilizing a good light source will address some of the challenges associated with minimally invasive surgery. After basic skills are learned, the only requirement to gain mastery of intracorporeal suturing is practice. Several endoscopic training systems are available for practice, but a simple cardboard or plastic box can also suffice. Set the trainer at table height, connect the light source to the laparoscope, insert a few trocars, and practice (Figure 13-1).
Practice Tip 2: Invest in Laparoscopic Needle Holders
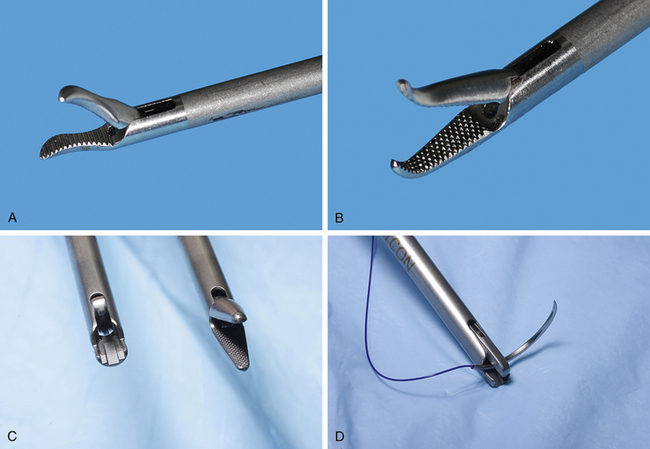
Reusable 5-mm needle holders are available from several equipment manufacturers. They may be obtained with straight or curved jaws (Figure 13-2, A-B). Curved jaws provide the advantages of assisting with loop formation, helping to keep the suture from slipping off the jaws, and providing better visibility of the suture site. A “self-righting” needle holder has a feature that will assist the needle in assuming the correct orientation for suturing (Figure 13-2, C-D). Laparoscopic needle holders have a handle that is in axial alignment with the shaft of the device. Axial alignment provides flexibility with respect to port location and makes it possible to rotate the shaft 360 degrees. Finally, laparoscopic needle holders need a ratchet mechanism that is adjustable so that secure fixation of the needle in the jaws of the instrument is ensured; however, the mechanism must be easily locked and released during the procedure. Experienced laparoscopic surgeons prefer a pair of needle holders so that either device can be used for suturing. Recommended instrumentation is listed in Box 13-1.
Practice Tip 3: Plan the Operative Approach
The ideal setup for laparoscopic suturing is similar to that for other laparoscopic procedures. Using the baseball diamond analogy, think of the camera port being positioned at home plate, the wound positioned at second base, and the working ports for insertion of the needle holder and grasping forceps at first and third bases. The video monitor represents the outfield (Figure 13-3). Whenever possible, position the wound to be sutured in the 12-o’clock to 6-o’clock orientation. The surgeon will be using the needle holder and grasping forceps inserted through the working ports, and the camera holder typically reaches under the surgeon’s arm to hold the laparoscope. Evaluate the length of the needle holder shaft to ensure that it will reach the wound site, and whenever possible, separate the working ports by 15 to 20 cm, placing each of them about 10 cm from the camera port. Keep the instrument tips close to the wound surface to minimize depth perception issues.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree