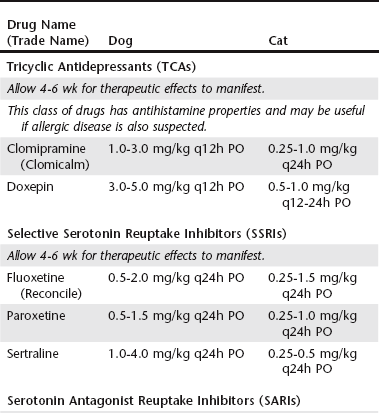
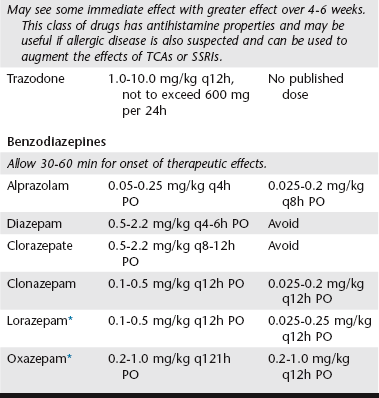
Chapter 117 When a concurrent pruritic disease is being treated, the antihistamine properties of TCAs offer an additional benefit. Doxepin has the most potent antihistamine properties of any of the TCAs and, in fact, has 600 to 800 times the antihistamine effects of diphenhydramine. Unfortunately, the serotonin-enhancing effects of doxepin are the lowest in its class, which makes it a poor choice when anxiety or compulsion is the primary cause for the dermatosis. Each clinician should weigh the effects of both anxiety/compulsion and pruritus when choosing a TCA that will affect skin and behavior. See Table 117-1 for dosing recommendations. TABLE 117-1 Systemic Drugs and Suggested Dosages for the Treatment of Behavioral Dermatoses *No active hepatic metabolites—may be safer in geriatric and feline patients.
Drugs for Behavior-Related Dermatoses
Classes of Psychotropic Medications
Tricyclic Antidepressants
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Drugs for Behavior-Related Dermatoses
Only gold members can continue reading. Log In or Register to continue
