Chapter 12 Diseases that Affect the Pinna
Most skin diseases may affect the pinna in dogs and cats, but other parts of the body can also be involved. Other than neoplasia, few dermatoses are restricted to the pinnae. Dermatoses restricted to the pinnae include aural hematoma, physical dermatoses (e.g., trauma, solar dermatitis, frostbite), arthropod bites, neoplasia, vasculitis, contact dermatitis, fissure or seborrhea of the ear margin, pinnal alopecia, and psoriasiform-lichenoid dermatitis of Springer Spaniels. Many other dermatoses may induce lesions that begin or stay confined to the pinna for some time, but they usually involve other body sites at some point of their evolution (e.g., sarcoptic mange, dermatophytosis, atopic dermatitis, pemphigus complex).
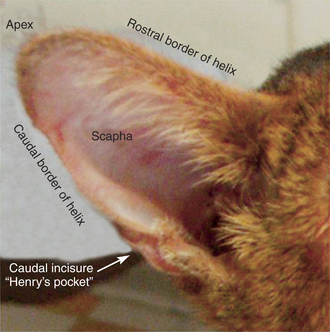
Pinna Anatomy
The pinna, or auricle, consists of the flat part of the auricular cartilage, covered by skin on both sides. The convex surface is haired, even in some hairless breeds such as the Chinese Crested dog. Most of the concave surface is glabrous in cats and is variably haired in dogs, depending on the breed. In the most hirsute breeds such as the Cocker Spaniel the area around the ear canal opening is glabrous. The proximal part of the auricular cartilage folds into different tubercles and ridges and forms the ear canal opening, which includes the anthelix (medial), tragus (lateral), and antitragus (caudal) (Figure 12-1). (See also Chapter 1.)
Aural Hematoma
Clinically, aural hematomas result in large fluctuant swellings of various sizes, but usually they affect most of the ear pinna above the anthelix. During the first days, the swelling is warm to hot to the touch, and the overlying skin is erythematous. The animal is greatly bothered by the increased weight of the ear and sometimes seems to experience pain. Aspiration fluid obtained within hours of hematoma formation is sero-hemorrhagic and usually rich in fibrin. The presence of fibrin can prevent aspiration of any fluid later in the disease. The normal evolution of a hematoma is resorption of the fluid and healing. Fibrosis is always a major feature of the aural hematoma healing process, especially if left untreated. The pinna becomes thick, hard, and permanently distorted as the fibrosis in the wound contracts. Because aural hematoma is rarely seen in dogs and cats with major trauma to their pinna, minor ear trauma and/or pruritus is more likely a precipitating factor than a primary cause. Most studies reveal the following:1
In one study, results were in favor of an autoimmune cause.2 Joyce and Day could not confirm these results, even though they did find histopathologic evidence of cartilage degeneration associated with fibrovascular granulation tissue filling the cartilage defect.1 They presumed that their samples (incisional biopsies of affected pinna) reflected the end process of cartilage degeneration that might have been caused by the mediators released by macrophages earlier in the process. These considerations are in favor of a process, most probably immune-mediated, that began several weeks before the aural hematoma was observed by the owner. Diagnosis of aural hematoma is usually straightforward and is based on history, clinical presentation, and fluid collection. Because the disease is self-limiting and heals spontaneously, some owners may choose not to treat their animal. Nevertheless, the hematoma greatly bothers the animal. Cosmetic considerations are also in favor of surgical treatment.
Several surgical techniques have been described. Fluid drainage (aspiration, indwelling drain, partial or whole-length incision) and flushing are effective in relieving the animal but usually result in post-treatment deformity of the ear pinna. Griffin found that surgical procedures aiming at prevention of immediate relapse by compression (without necrosis) and at restoration of the pinna’s initial shape and carriage are the most cosmetically effective and have the least recurrences.3 This can be achieved by several techniques. The most commonly used are multiple mattress sutures placed after incision or multiple punch holes made through the skin (see Chapter 19). Mattress sutures may also be placed through a soft but rigid device (several types are marketed that usually contain foam).
Because the healing of aural hematomas is highly fibrotic, glucosteroids are flushed into the hematoma cavity. They are also given orally with antibiotics, at least until the sutures are removed and the incision has healed.2 Even though trauma is probably only a precipitating factor, it should be avoided as much as possible to prevent relapses. It is mandatory to identify and correct the cause. Otitis externa and pinnal skin diseases are most commonly encountered (Figure 12-2).6
Pinnal Trauma
The most common causes of pinnal trauma are pruritus or fight wounds; they also may be related to common dog habits such as earth digging and chasing other animals (Figure 12-3). Complications at the surgery site, including infection and tearing of the stitches, are common where ear cropping is still allowed. Pinnal trauma is usually associated with prolific bleeding. Routine wound cleaning and topical hemostatic application (peroxide, epinephrine, or collagen) are usually sufficient treatment. In severe cases, cauterization under anesthesia and/or compressive bandage might be necessary. Due to the thin edges of the pinna, laceration of the ear margin can be a permanent sequel.
Pruritic Dermatoses
Pruritus is probably the most common cause of pinnal lesions in dogs and cats. The origin of the pruritus can be the pinna itself, as in arthropod-related dermatoses, atopic dermatitis, or contact dermatitis.4 Nevertheless, pinnal pruritus is most commonly caused by otitis externa (e.g., otodectic mange, foreign body, Malassezia otitis externa, atopic dermatitis) or facial diseases (e.g., intertrigo, food allergy, atopic dermatitis, conjunctivitis).4 Pruritus results in pinnal alopecia, excoriation, and crusting.
Sarcoptic Mange
The pinna is one of the favorite habitats of the mite. Early pinnal lesions are abundant, with yellowish crusts that adhere between hairs. The entire border of the pinna may be involved. Pruritus is usually intense and results in pinnal trauma, hair loss, excoriation, and erythema. Because the pathogenesis of scabies involves a hypersensitivity reaction, some dogs may experience only mild pruritus. An anergic form is described where affected animals are almost nonpruritic in spite of the presence of hundreds of mites.5 More commonly, clinical signs of scabies can be more subtle or have a different localization in dogs treated for fleas and ticks with drugs used against acarids (permethrin, other pyrethroids, fipronil, amitraz) that are not completely efficient due to their spectrum, the formulation used (spot-on, collars, shampoo), the amount used, or the frequency of application.
Notoedric Mange
Treatment of the premises is mandatory because the mite can survive for more than 2 weeks in the environment.5
Trombiculiasis
Treatment should aim at killing the mites present on the animal, relieving the pruritus, and preventing subsequent infestation. If infestation is localized, topical application of an otic ointment containing steroids and an insecticide is sufficient. Otherwise, an acaricidal spray should be associated with a 5- to 8-day course of oral prednisolone (1 mg/kg). If free roaming cannot be prevented, the prevention of reinfestation is difficult. An acaricidal spray with a strong repellent effect such as permethrin is an option for dogs but is toxic in cats. In one study on a small number of animals, fipronil spray applications seemed to achieve a more effective and lasting result in dogs than in cats.6 Trombicula autumnalis adults are found in the outside environment. Compost areas should be enclosed so that the pet cannot access them. Treatment of other favorable areas (under trees, under the house, in bushes) with insecticides should be discouraged because of the toxicity to invertebrates (pollinating insects, honeybees) and children and the presence of residue on fruits or vegetables grown in the garden.
Insect Bite Dermatitis
Insect bite dermatitis can be caused by various hematophagous insects due to the mediators or toxic products present in their saliva; it is sometimes associated with hypersensitivity reactions. Cats are more commonly affected than dogs, perhaps because they roam more and because of their “lie and wait” way of hunting. Papules, erythema, erosion, and alopecia are seen mainly on the thickened tip of the pinna. The border and the dorsal side can also be affected. In dog breeds with pendulous or broken ears, lesions are seen on the surface of the pinna where the ear folds down. In severe cases, multiple small ulcers covered with hemorrhagic crusts are present.
The causative insects vary with the season, environment, and climate.
Atopic Dermatitis
Erythema of the concave pinna is seen in more than 50% of atopic dermatitis cases in dogs and is the only symptom for a year or more before the development of other symptoms in at least 3% of canine cases.10–12 Associated pruritus is intense (Figure 12-4).
Lichenification and thickening of the concave pinna usually occur. Seborrhea and Malassezia dermatitis are common complications. This frequent feature might be explained in part by the observation made on 10 normal dogs, where mast cell counts were found to be highest in the medial and lateral pinna.7 Otitis externa, cheilitis, and conjunctivitis are also frequently encountered in canine atopic dermatitis and also cause pinnal pruritus and trauma.
Food Allergy
Food allergy is commonly associated with auricular disease both in dogs and cats (see Chapter 6). The pathogenesis of cutaneous nontoxic adverse reaction to food can involve immune-mediated or non–immune-mediated mechanisms. They are respectively called food allergy/hypersensitivity and food intolerance. The precise mechanisms are not elucidated in animals and are a point of controversy in humans.
In one study of 51 food-allergic dogs, Rosser8 stated that 80% of cases had otitis externa and that it was the only symptom in 20%. Pinnal lesions mainly result from otitis externa–related pruritus (Figure 12-5). Improvements in pruritus and skin lesions during the food trial may not be obvious if the perpetuating factors of the otitis externa are not treated initially (bacteria or yeast proliferation, inflammation associated ear canal or pinna changes).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree