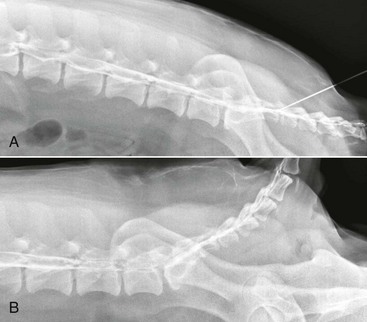
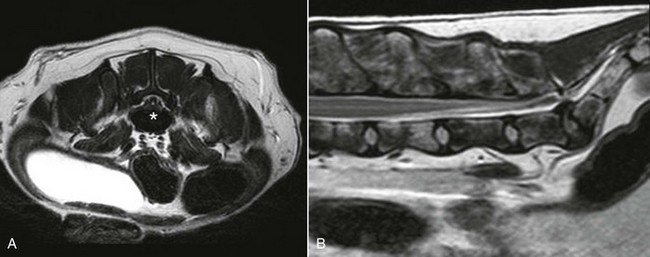
Chapter 238 Contrast studies can provide additional information beyond survey radiographs. Myelography is the least helpful of the contrast studies available. The dural sac termination site is variable in each dog. For myelography to provide diagnostic findings in cases of lumbosacral stenosis, the dural sac must extend into the sacrum. Diskography and epidurography provide better diagnostic information. Epidurography is used to evaluate neural compression (Figure 238-1). Diskographic abnormalities that confirm lumbosacral disease are intradiskal accumulation of the contrast agent, focal extravasation of contrast into the canal, and the presence of contrast within the disk. Transosseous and intravenous venography involve injection of a contrast agent into the vertebral venous sinus system to evaluate spinal cord compression indirectly. Figure 238-1 A, Lateral epidurogram for a 7-year-old neutered male Labrador retriever brought in because of back pain. He was diagnosed with a lumbosacral herniated disk. With the tail flexed there is minimal attenuation of contrast at the lumbosacral disk space. B, Epidurogram for the same dog with the tail extended. Note the bulge of the lumbosacral disk and attenuation of contrast. Magnetic resonance imaging (MRI) provides the best soft tissue resolution, allows images to be acquired in multiple planes without degradation, and can detect disk degeneration earlier (Figure 238-2). Other advantages of MRI over CT are excellent visualization of the nerve roots, intervertebral disks, and ligaments and lack of exposure to ionizing radiation. MRI tends to be the most sensitive method for diagnosis of lumbosacral stenosis, but with excellent resolution also comes the potential for overdiagnosis. It is best to correlate imaging findings with the results of clinical assessment. Figure 238-2 A, Axial T2-weighted magnetic resonance image of a 3-year-old neutered male French bulldog that became nonambulatory in the hind limbs and was diagnosed with a herniated lumbosacral disk. Note the compression of the nerve roots above the extruded disk (asterisk). B, Midsagittal T2-weighted MRI of the same dog. Note the compressive lumbosacral disk in the lumbar region.
Diagnosis and Treatment of Degenerative Lumbosacral Stenosis
Diagnosis
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


