Chapter 64 Daily Intravenous Fluid Therapy
INTRODUCTION
Intravenous fluid therapy is vital for the management of shock, dehydration, and maintenance in animals that require parenteral fluid therapy (see Chapters 61, 62, and 63, Peripheral Venous Catheterization, Intraosseous Catheterization, and Central Venous Catheterization, respectively, and Chapter 65 and 66, Shock Fluids and Fluid Challenge and Transfusion Medicine, respectively). This chapter focuses primarily on the distribution of total body water, patient assessment, and the delivery of synthetic intravenous fluids to maintain normal water, electrolyte, and acid-base status in critically ill dogs and cats that are hemodynamically stable. Because critically ill animals often have fluid and electrolyte balance derangements, overall recovery often depends on recognition and appropriate treatment of these disorders, in addition to diagnosing and treating the primary disease process.
TOTAL BODY WATER
Living organisms are predominantly composed of water. Total body water content is approximately 60% of body weight in a nonobese adult dog or cat. Total body water is distributed between two main compartments: intracellular fluid (ICF) and extracellular fluid (ECF) (Figure 64-1). Each compartment consists of solutes, primarily electrolytes, dissolved in water. The most important determinant of the size of each body fluid compartment is the quantity of solutes contained in that compartment.1,2
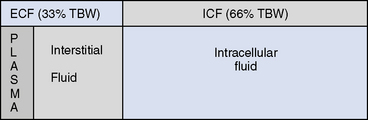
Figure 64-1 The distribution of total body water (TBW). ECF, Extracellular fluid; ICF, intracellular fluid.
MOVEMENT OF FLUIDS WITHIN THE BODY
Hypotonic Fluid Loss
Hypotonic fluid losses, as seen with diabetes insipidus or excessive panting, will cause hypernatremia and an increase in ECF osmolality. This will lead to movement of water out of the ICF space. Consequently, there is a depletion of both the ICF and ECF compartments. Isotonic fluid therapy may be sufficient if the hypernatremia is not severe, but in animals with significant hypotonic fluid losses, free water administration is indicated. Care must be taken to lower serum sodium slowly to avoid causing potentially life-threatening cerebral edema (see Chapter 54, Sodium Disorders).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


