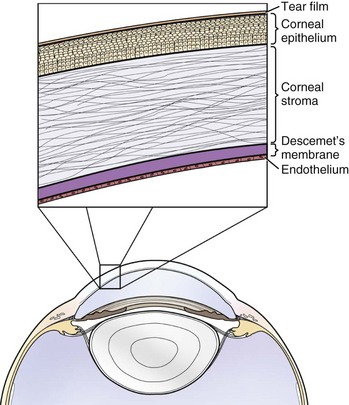
Chapter 246 The cornea and sclera make up the tough and protective fibrous tunic of the eye. The cornea is composed of five layers: precorneal tear film, epithelium with basement membrane, stroma, Descemet’s membrane, and endothelium (Figure 246-1). The cornea can be described as a “fat-water-fat” sandwich; the epithelium and endothelium–Descemet’s membrane are hydrophobic, whereas the collagenous stroma is hydrophilic. Figure 246-1 Diagram of equine cornea. Enlarged inset demonstrates relative proportions of corneal epithelium, stroma, and Descemet’s membrane/endothelium. (From Gilger B: Equine ophthalmology, ed 2, St Louis, 2011, Saunders.) Corneal transparency is maintained by the following five mechanisms: 1. The corneal epithelium contains no pigment. 3. The corneal epithelium is nonkeratinized. 4. The stromal collagen lamellae have a precise anatomic arrangement. Simple ulcers are defined by the following criteria: 1. Superficial. Only epithelium has been lost, with no loss of stroma. 2. No evidence of infection. Infection in the cornea usually appears as stromal infiltrate, which is caused by inflammatory cells migrating within the cornea that give it a yellow, white, or tan appearance. 3. Healing in an appropriate amount of time. Epithelium is very mitotically active, and even an ulcer that encompasses 90% of the corneal surface (provided it involves loss of epithelium and no loss of stroma) can be expected to be healed in 7 to 10 days. Ulcers usually take about 1 day to heal for every 1 mm of width. 4. No complicating factors. No underlying cause for the ulcer can be identified that would need to be corrected.
Corneal Ulcers
Corneal Anatomy
Physiology of Corneal Transparency
Simple Corneal Ulcers
< div class='tao-gold-member'>
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


