It is critical that articular fractures be treated surgically with anatomic reduction and rigid stabilization of the articular surfaces. This is generally achieved using implants such as screws, wires, pins, or small plates. Nonsteroidal antiinflammatory drugs (NSAIDs), other analgesics, passive range of motion (PROM) exercises, and short leash walks are used for the first few weeks after surgery. The goal of the early postoperative period is to maintain and improve joint range of motion (ROM), limit periarticular fibrous tissue, and allow time for adequate bone healing to support more vigorous active weight-bearing exercises. After adequate healing has occurred, physical rehabilitation consists of continued ROM exercises with stretching if needed, and active weight-bearing exercises such as progressive leash walking and aquatic therapy (Table 32-1). Table 32-1 Rehabilitation After Surgical Repair of Articular Fracture Osteochondrosis is a developmental disease affecting the growth plates and joint cartilage in medium and large breed dogs. Abnormal endochondral ossification of the deep layers of articular cartilage results in focal areas of thickened cartilage that are prone to injury. Normal activity may cause enough stress to create a fissure in the articular cartilage. Contact of the synovial fluid with the deep layers of degenerating cartilage may cause synovitis. In the absence of further stress, the lesion may heal. However, further stress on the cartilage may result in formation of a cartilage flap. This condition is termed osteochondritis dissecans (OCD). Osteochondritis dissecans has been described in various joints of the dog, but occurs most commonly in the caudal aspect of the humeral head. The etiology is multifactorial in all species. Risk factors in dogs include young age, large and giant breeds, rapid growth (high calorie diet), and excess calcium consumption.1 Dogs are typically presented with mild to moderate weight-bearing lameness between 4 and 8 months of age. Many dogs have bilateral lesions, although one side may be clinically more severe. Muscle atrophy may be apparent in the affected limb if the dog has had a chronic lameness. Pain may be elicited on extreme flexion or extension of the shoulder. Radiographs may demonstrate a defect in the subchondral bone under the cartilage flap on the caudal aspect of the humeral head (Figure 32-1). Uncommonly, advanced imaging or arthroscopy is needed to confirm the diagnosis.2 If shoulder osteochondrosis is diagnosed early, decreased activity may prevent cartilage flap formation. Cryotherapy and NSAIDs may be used to limit inflammation. Use of disease-modifying osteoarthritis agents (DMOAs), such as glucosamine and chondroitin sulfate, may support cartilage health. Passive range of motion exercises help to maintain joint range of motion and provide joint nutrition and stress along normal lines of movement.3 Once a flap has formed it will not heal and should be removed. If the dog is more than 7 months of age or the lameness has persisted more than 4 to 6 weeks, surgery is indicated.4 Surgery is generally the treatment of choice in dogs with clinical signs. It is performed via arthrotomy or arthroscopy to remove the defective cartilage and forage or curettage the bed of the lesion (Figure 32-2). This encourages vascular ingrowth and healing by the formation of fibrocartilage. After surgery NSAIDs, cryotherapy, PROM, and controlled leash walks are instituted for the first 2 to 4 weeks (Table 32-2). After this initial healing period the duration of the leash walks is progressively intensified. In addition treadmill walking, UWTM exercise, and swimming may be initiated. By 6 weeks, light jogging usually can be started.3 Seroma formation is a common complication after shoulder surgery by arthrotomy, but is usually self-limiting and resolves with rest. If a shoulder seroma is observed, the activity level should be reduced until it resolves. The value of treating a seroma with hot packs or cold packs has not been documented, but is commonly recommended. Long-term management of OCD is focused on limiting or treating osteoarthritis (OA). The long-term prognosis for shoulder OCD is excellent in most cases.2,5 Table 32-2 Joint Rehabilitation After Osteochondritis Dissecans Surgery Bicipital tenosynovitis is a degenerative or failed healing response of the tendon and tendon sheath of the biceps brachii muscle.6,7 Inflammation is not consistently present. Tendonitis implies the presence of inflammation in the tendon and musculotendinous junction, and may not be accurate for many cases of tendon pain.8,9 Tendinopathy is an inclusive term used to describe tendon pathologies such as tendonitis, tendinosis, or paratenonitis. Tendon injuries may be caused by acute trauma or repetitive loading. Repetitive tendon overload tends to respond with tendon sheath inflammation, tendon degeneration, or both. There is some evidence that acute tendinitis is quickly replaced by tendon degeneration.10 Tendon pain should not be assumed to be caused by inflammation, but can occur with tendinosis as well. Conservative management of tendinopathies or tendinitis in humans primarily consists of rest, icing, and eccentric strengthening exercises. There are little data to support the use of therapeutic ultrasound, shock wave therapy, orthotics or massage,8 but these are used in some cases. Analgesics are indicated, but not necessarily NSAIDs or corticosteroids. Deep transverse friction massage has been advocated as part of the treatment for tendinopathy pain. Studies of the effectiveness of deep transverse friction massage for the treatment of tendinopathies in humans are inconclusive.11 Common recommendations for the conservative management of tendinopathies in dogs include 4 to 12 weeks of rest and NSAIDs as needed (Table 32-3). As an alternative to oral NSAID therapy, intraarticular corticosteroids may be administered because the shoulder joint communicates with the biceps tendon sheath. Pulsed-mode 3-MHz therapeutic ultrasound is advocated over the tendon and musculotendinous junction to promote tissue healing. Because of the close proximity to bone, the dog must be monitored for any signs of pain, and the ultrasound intensity adjusted accordingly. Pulsed-mode ultrasound should not result in significant tissue temperature increase. Laser therapy may also be used to decrease pain and aid healing. Cryotherapy may be prescribed to reduce inflammation and pain. Response to conservative therapy varies, and may be related to the inciting cause of the tendinopathy.12,13 Full recovery can be expected to require 3 to 6 months of therapy.8 Table 32-3 Rehabilitation for Tendinopathies Surgical treatment is recommended for dogs that do not respond to medical treatment or have significant tears of the tendon. Surgical techniques include tenodesis or tendon release, both of which have been described as arthroscopic or open procedures.12,14–16 Cryotherapy, PROM, and short leash walks (preferably with a harness that does not rub over the surgical site) are used for the first 3 postoperative weeks to promote normal joint movement while the tendon has minimal strength. Joint mobilizations may also help increase joint ROM. Exercises to gradually increase limb strength and promote remodeling of the peritendinous scar are performed after 3 weeks. Exercises should emphasize strengthening of the brachialis muscle, to improve the dog’s ability to flex the elbow joint. Shake hands exercises with limb weights that are gradually increased, as well as walking over cavaletti rails with limb weights, are specific exercises to increase the strength of elbow flexor muscles. Aquatic therapy and treadmill exercises may be beneficial. Superficial heat therapy may be used before exercise to facilitate tissue extensibility. Neuromuscular electrical stimulation may be applied to the brachialis muscle. Cross-fiber frictional massage can be used to prevent or diminish adhesions. Cryotherapy may help to minimize postexercise inflammation. Most surgically treated dogs regain near normal function and gait.12,13 Supraspinatus tendinopathy may cause mild to moderate lameness in medium and large breed dogs. The etiology of supraspinatus tendinopathy is unknown, but it is speculated to be caused by overuse and repetitive trauma.17 Affected dogs typically have chronic, intermittent, unilateral lameness. Palpation of the greater tubercle, near the tendon insertion, is usually painful. Mineralization may be observed on radiographs, and may contribute to bicipital tenosynovitis or impingement of the biceps tendon. However, the presence of mineralization can also be asymptomatic and may be an incidental finding. Diagnostic ultrasound or MRI may be needed to identify nonmineralized tendinopathy. Medical treatment includes rest, PROM, NSAIDs, local steroid injection, heat or cold therapy, deep massage therapy, and therapeutic ultrasound. Response to these treatments is limited. However, pulsed therapeutic ultrasound resulted in some clinical improvement in one study of calcific tendonitis in humans.18 Extracorporeal shock wave therapy may decrease the size of the mineralized region in dogs.19 If medical treatment is inadequate, surgical excision of the mineralized tissue is recommended.17,20–22 After surgery, a carpal flexion bandage may be applied for 2 weeks to prevent weight bearing. Activity is limited for an additional 2 to 3 weeks. Swimming may cause too much tendon stress and is not advised for several months. The prognosis varies with the severity of the mineralization.17 Most dogs will be sound within 3 to 4 weeks. Lameness may recur with persistent bicipital tenosynovitis or recurrence of supraspinatus mineralization. Medial glenohumeral instability is thought to result from chronic repetitive activity or overuse, such as jumping. Dogs typically develop a chronic, intermittent weight-bearing lameness that is nonresponsive to treatment with NSAIDs. Instability may be assessed subjectively by palpating for increased translocation of the humerus.23 Medial instability can be confirmed by goniometric measurements of shoulder abduction,24 although the clinician should consider the role of pain-related muscle atrophy as a potential cause for increased shoulder abduction as opposed to true instability of the shoulder. The normal abduction angle in a large breed dog is approximately 30 degrees.24 The affected shoulder will have a much larger abduction angle as compared with the normal shoulder.24 The degree of instability may be characterized as mild, moderate, or severe.25 Mild instability is associated with minimal pathologic changes and abduction angles of 35 to 45 degrees. Dogs with moderate instability have abduction angles of 45 to 65 degrees and more advanced pathology is seen arthroscopically. Dogs with severe instability typically have shoulder abduction angles greater than 65 degrees. Severe disruption of the medial glenohumeral ligament, subscapularis tendon, and joint capsule are seen arthroscopically.25 Conservative treatment with the shoulder supported and restricted by shoulder hobbles can be used in mild cases. Extracorporeal shockwave treatment to the medial shoulder structures may be beneficial. As healing progresses, strengthening of the medial supporting muscles may be achieved by walking on a treadmill with lateral tension supplied by an elastic band during the swing phase of gait. As strength improves progressively stiffer elastic bands may be used. Dogs with moderate shoulder instability are treated arthroscopically with imbrication, thermal capsulorrhaphy, reconstruction of the medial glenohumeral ligament, or transposition of the biceps tendon.26,27 After surgery a shoulder support wrap with hobbles is applied to protect the surgical repair. Cryotherapy, PROM, and strictly controlled activity are instituted for the first 3 postoperative weeks.25 After 3 weeks weight-bearing exercises are gradually introduced. Function improves within three to four months, and optimal function is not attained until 5 to 6 months following thermal capsulorrhaphy.26 Severe shoulder instability is usually caused by trauma and is treated as for acute shoulder luxation. Contracture is a shortening of the tendon-muscle unit that is not caused by active muscle contraction. Most or all of the muscle and/or associated tendon is replaced by fibrous tissue. Most cases of contracture have a history of acute injury with lameness and inflammation that subsides with supportive care. Weeks to months later the animal is presented with clinical signs, which may include pain, weakness, firmness within the muscle, and an abnormal posture and gait.28 Proposed causes include infection, trauma, repetitive strains, fractures, infectious diseases, immune-mediated diseases, ischemia, and eosinophilic myositis. Muscle contracture leads to permanent shortening of the affected muscle and can limit ROM of the associated joint. Muscle contracture can occur in any muscle, but has been reported in the infraspinatus, supraspinatus, teres minor, brachialis, quadriceps, semitendinosus, gracilis, and sartorius.28 If the contracture is not severe, splinting with the muscle and tendon in tension and stretching activities may lengthen the tendon-muscle unit. In many cases, surgery is recommended to lengthen or transect the tendon. Contracture in the front limb has been most commonly reported in the infraspinatus muscle. Infraspinatus contracture causes a mild weight-bearing lameness mainly in hunting or working dogs. The cause is hypothesized to be acute muscle trauma, which results in incomplete rupture of the infraspinatus muscle. The injury leads to inflammation and subsequent compartment syndrome.28–30 Replacement of muscle fibers by fibrous tissue occurs over days to weeks. The supraspinatus and deltoid muscles also may be involved and undergo atrophy or contracture.31 The humerus is held in adduction, whereas the antebrachium is externally rotated with the foot abducted. The scapulohumeral joint cannot fully extend. There is a weight-bearing lameness in which the limb circumducts as it is advanced during the stride and the paw flips into extension before foot placement. Physical rehabilitation may be beneficial if the condition is diagnosed early. Continuous mode therapeutic ultrasound with stretching exercises may help to lengthen contracted tissues, but the degree of contracture is usually so severe at the time of diagnosis that it is difficult to improve the condition.3 When the dog is presented with contracture, the treatment of choice is surgical transection of the infraspinatus tendon and associated fibrous tissue.31 This immediately restores motion of the shoulder joint and the prognosis is good. Postoperatively full weight bearing is allowed, but activity should be restricted for the first few weeks. Uncontrolled activity may cause tissue damage and recurrence of fibrous tissue.3 Passive ROM exercises to the forelimb joints several times daily maintain joint ROM and promote normal alignment of the healing tissues.3 Cryotherapy may be used to reduce inflammation after exercise. In cases in which there is significant disuse atrophy of the forelimb muscles, general conditioning exercises for the limb are used to gradually return the muscle to normal size and strength. Conditioning exercises include walking, jogging, and aquatic therapy. Neuromuscular electrical stimulation (NMES) may be used if the atrophy is severe and the dog is too weak to use the leg well. Teres minor strain has been reported in athletic dogs of various breeds.32 All dogs in one report had front limb lameness that was improved by rest, but recurred with return to activity. The shoulder was painful on full extension and pain was elicited with direct palpation of the teres minor muscle. Treatment included ultrasound, stretching, balancing exercises, leash walking, gait retraining, and acupuncture point stimulation. All dogs returned to previous levels of activity.32 Fractures of the articular surface of the distal humerus are common and typically result from trauma. Articular fractures of the proximal radius and ulna are much less common. Salter-Harris type IV fractures of the lateral condyle of the humerus are commonly seen in skeletally immature dogs, and fractures of the lateral humeral condyle are also seen in older dogs. In spaniel breeds, such as Cocker spaniels, it is not uncommon for mature animals to present with articular fractures with minimal evidence or history of trauma (Figure 32-3). These dogs appear to have incomplete ossification of the humeral condyles, although there may be other predisposing factors.33 As with any articular fracture, decreased ROM and destruction of articular cartilage may be sequelae of an articular fracture. In addition Salter-Harris fractures in immature dogs may have alteration in bone growth that is necessary for a congruent elbow joint. Repair is accomplished with placement of a transcondylar screw with compression of the fracture site and placement of a small antirotational pin driven up the lateral epicondyle (Figure 32-4). Articular fractures demand both rigid fixation and anatomic reduction to maintain an even, stable cartilage surface. Because of the necessity for anatomic reduction, the surgical approach may be extensive, including tenotomies or osteotomies. The surgeon must carefully balance the degree of soft tissue manipulation with the need for exposure of the fracture to facilitate reduction. Extensive dissection increases postoperative pain and swelling, and may increase the degree of muscle scarring and periarticular fibrosis after surgery. In our experience excessive postoperative scarring and fibrosis leading to decreased range of motion are particularly likely after articular fractures involving the distal humerus or distal femur in the dog and cat. The use of minimally invasive techniques, such as closed reduction and fixation via the use of fluoroscopy, or arthroscopic-assisted fracture reduction should be considered (Figure 32-5).34 Whenever possible, osteotomies rather than tenotomies should be performed to gain access to the fracture because osteotomies heal by reforming normal bone, whereas tenotomies heal via scar tissue. When osteotomies are repaired the surgeon must pay particular attention to pin and wire placement. Inadvertent wire placement into the joint causes mechanical loss of range of motion and pain for the patient, rendering even the most sophisticated rehabilitation strategy useless. In addition to the demand for anatomic reduction, rigid fixation of articular fractures may rely on implants placed across a small epiphyseal segment, resulting in a somewhat tenuous repair, especially in young patients with soft bone. In the case of distal humeral fractures, particularly Salter type IV fractures in young dogs, the surgeon may be tempted to splint the limb or place a carpal flexion bandage to prevent weight bearing. Although these strategies may effectively prevent mechanical overload of the repair during the healing process, they may have the unintended effect of promoting muscle scarring around the operative site as well as cartilage atrophy.35 Although a carpal flexion bandage still allows some ROM exercises, contracture of muscles around the carpus may lead to longstanding pain, loss of ROM and poor limb use despite good fracture healing. ROM exercises should be performed frequently but are best left to professionals as excessive (or too little) ROM can cause failure of fixation or joint contractures respectively. Weight-bearing exercises should be used with extreme caution, especially during the first 3 weeks after repair to avoid fixation failure. Short leash walks may be permitted, but it is important to properly confine the patient to avoid catastrophic failure, especially if the patient appears to be doing very well. Cryotherapy, analgesic medication, massage, and passive ROM may be used for articular fractures of the elbow (see Table 32-1). In small breed dogs use of a therapy ball may be helpful to encourage limb use and flexion of the elbow without direct manipulation of the limb (Figure 32-6). It is imperative that ROM exercises continue for 3 to 4 weeks after surgery to be certain that ROM is maintained. Normal ROM may return 10 to 14 days after surgery, but fibrous tissue and other healing periarticular tissues are not yet mature. If ROM exercises are discontinued too soon, it is possible that some maturation and contracture of tissues may occur with some loss of normal joint motion. These fractures can present a very difficult challenge to the surgeon and the rehabilitation practitioner. Although overuse may result in catastrophic failure of the repair, failure to perform appropriate ROM exercises may lead to crippling loss of ROM. Elbow dysplasia includes fragmented medial coronoid process (FCP), osteochondritis dissecans (OCD), and ununited anconeal process (UAP). Dogs with elbow dysplasia usually have only one of the three conditions. Elbow incongruity may also be present. The pathogenesis is poorly understood. Factors that have been implicated include genetics, improper nutrition, and trauma. Other proposed mechanisms are osteochondrosis, trochlear notch dysplasia, and asynchronous growth of the radius and ulna.36 Elbow dysplasia usually occurs in large or giant breeds of dogs. Affected dogs typically have bilateral problems, although one elbow may be more severely affected. Dogs with FCP are presented with a mild to moderate weight-bearing lameness, which is usually noted between 4 and 7 months of age.37 Physical exam findings include pain on flexion and extension of the elbow, pain on palpation of the medial aspect of the joint, and palpable joint effusion. In dogs older than 11 months, crepitus, decreased ROM, and general joint thickening may be evident. Radiographs often show degenerative changes in the joint, but the actual lesion may not be seen (Figure 32-7). In many cases, computed tomography or arthroscopy is needed to make a definitive diagnosis. Treatment is removal of the abnormal process via arthrotomy or arthroscopy, with possible subtotal coronoidectomy or ulnar osteotomy in some cases. Postoperatively activity is limited for 2 to 4 weeks. The prognosis is good if FCP is removed before there is advanced OA. Osteoarthritis will progress regardless of treatment, but changes are thought to be more severe in untreated cases. If the OA is severe at the time of diagnosis, the value of surgical treatment must be questioned. These dogs may be better managed by conservative treatment for the OA.37 In all cases rehabilitation is directed toward preventing, slowing, or treating OA to maintain an acceptable quality of life. Therapy includes maintaining an appropriate body weight, controlled low-impact exercise, aquatic exercise, monitoring pain, NSAIDs, and chondroprotective agents. See section on OA for guidelines on rehabilitation. Dogs with elbow OCD are typically presented with mild to moderate lameness between 4 and 9 months of age. Many dogs have bilateral lesions, although one side may be clinically more severe. Atrophy of the muscles may be apparent in the affected limb if the dog has been lame for several weeks. Pain may be elicited on extreme flexion or extension of the affected joint. Chronic elbow OCD may also have signs of OA such as joint effusion, thickening of the periarticular soft tissues, decreased ROM, and crepitus. Radiographs may demonstrate a defect in the subchondral bone under the cartilage flap on the medial humeral condyle. Fragmented medial coronoid process can create an erosive lesion on the medial humeral condyle, called a kissing lesion, which can look very similar to OCD at the time of surgery (Figure 32-8). In some cases especially with elbow OCD, the diagnosis may be difficult and is best made by computed tomography or arthroscopy. Surgery is usually the treatment of choice in dogs with clinical signs. It is performed via arthrotomy or arthroscopy to remove the defective cartilage and forage or curettage of the lesion. After surgery NSAIDs, cryotherapy, PROM, and controlled leash walks are instituted for the first few weeks (see Table 32-2). After the initial healing period, the duration of the leash walks are progressively intensified. Long-term management of OCD is focused on limiting or treating OA. See section on OA for guidelines on rehabilitation. The prognosis for elbow OCD is good if surgery is performed before OA is advanced, but it is more guarded than for OCD of the shoulder. Ununited anconeal process (UAP) is a failure of the anconeal process to fuse with the olecranon by 5 months of age, and is apparent on a flexed lateral radiograph (Figure 32-9).37 Instability of the anconeal process causes inflammation and eventual OA. The dog usually is presented with a weight-bearing lameness. Decreased range of motion and joint effusion of the caudolateral aspect of the elbow may be apparent on palpation If the UAP is treated by screw fixation, the rehabilitation program should have a slower progression of weight-bearing activities until there is radiographic evidence of healing. This may take as long as 12 weeks in some cases. If the UAP was treated by removal, the rehabilitation program may progress more rapidly, as dictated by the degree of joint effusion, pain, ROM, and weight bearing. Immediately after surgery PROM, aquatic therapy, and light leash walks are recommended. Cryotherapy and NSAIDs may be used as needed to control inflammation and pain. Aquatic activity can be very beneficial because of the active ROM while weight bearing in a buoyant environment.38,39 Joint reduction and preservation of the joint may not be recommended if there are irreparable fractures involving the joint or severe congenital malformations. In these cases a joint salvage procedure, such as elbow arthrodesis, may be a better choice. Total elbow replacement surgery is relatively new in dogs and is not commonly performed, but may result in better function.41 Limb amputation may be elected in some cases. Fractures of the radius and ulna commonly occur. These injuries may be treated by closed reduction and immobilization in a cast in cases of simple fractures, or they may be repaired by open reduction and fixation with wires, plates, screws, or external skeletal fixation. In small dogs distal radius and ulna fractures have a high incidence of delayed or nonunion healing when treated with external coaptation (Figure 32-10). For optimal healing these fractures require anatomic reduction and rigid surgical fixation, while using appropriately sized implants to reduce the risk of stress protection. In addition to problems with bone healing, prolonged immobilization by splinting or casting leads to disuse atrophy of bone, cartilage, ligaments, tendons, and muscle in the affected limb. In some cases there is frank loss of bone distally in response to disuse of the leg. Following the first few weeks of physical rehabilitation, which involves reduction of pain and swelling, rehabilitation efforts can be undertaken to increase weight-bearing activities to load the bone during fracture healing and help stimulate normal healing. One of the main impediments to limb use is decreased ROM of the carpus as a result of flexural contracture of the soft tissues. Assisted extension of the carpus to a normal position is often painful and often results in a non–weight-bearing lameness, despite healing of the fracture. If a coaptation device is used, it is essential that particular attention be paid to stretching and ROM exercises of the carpus and digits. In some cases, an extension splint molded to the normal contralateral side may be placed on the affected limb, applying some tension to position the digits and metacarpals more normally in between rehabilitation sessions. It may take 10 to 14 days to achieve a normal angle of the carpus for weight bearing. After limb immobilization or prolonged disuse, the antebrachial flexor muscles may undergo contracture (shortening of the tendon-muscle unit). The result is limited extension of the joints distal to the elbow, which can impair normal weight-bearing. Methods of lengthening and stretching the contracted tendon-muscle units include 3-MHz therapeutic ultrasound or hot packs, manual stretching, exercises, and massage.42–44 If stretching is too aggressive it may cause damage to soft tissues or bone fractures. A prolonged stretch may be applied with a custom splint on the distal limb. The splint should be applied intermittently to minimize the risk of pressure injuries from the splint. The splint may be applied for longer periods each day until it can be worn all day, if desired. The goal is to stretch and realign the tissues without damaging them. Metacarpal and phalangeal fractures usually occur as a result of trauma, and phalangeal fractures are often open fractures (Figure 32-11). Carpal, metacarpal, and phalangeal fractures may be treated using closed reduction and immobilization in a coaptation device, or with a variety of implants including intramedullary pins, wires, and plates and screws (Figure 32-12). A splint or light cast is usually applied to the limb after internal fixation to protect the relatively small implants that must be used. If a cast or splint is used elbow ROM must be preserved during the time of coaptation application, and after coaptation removal. Sagittal plane ROM exercises and joint mobilization work well to restore ROM to the area. In cases of fracture and carpal instability, splinting is often used to protect the repair. If possible removing the splint on a weekly basis to perform ROM exercises to maintain joint and tendon mobility is advised. The splint is reapplied to protect the fracture after performing ROM exercises. Carpal hyperextension injuries occur after jumping or falling from a height, spraining the palmar fibrocartilage and the carpal ligaments. Damage may occur to antebrachiocarpal, middle carpal, carpometacarpal joints, or any combination of these joints. Carpal hyperextension may also be caused by immune-mediated joint disease, or endocrinopathy such as hyperadrenocortism. Affected animals are lame and walk with the carpus in hyperextension. In severe cases, the carpus may touch the ground. In general healing of a sprain (ligament injury) may take months, and occurs by the formation of fibrous connective tissue to replace the torn ligament, rather than primary healing of the ligament. Conservative management of carpal hyperextension injuries is generally unsuccessful and results in subluxation.45 The recommended treatment is panarthrodesis (surgical fusion of all three joint levels) or partial arthrodesis (fusion of only the middle and distal joints), depending on the level of the injuries (Figure 32-13). Rehabilitation is performed as for any arthrodesis, with an emphasis on gait training after the initial healing period (see General Physical Rehabilitation of Joint Arthrodesis). Although the limb function is not normal, prognosis for return to daily activity is good after carpal arthrodesis.46 The prognosis is more guarded if instability is caused by rheumatoid arthritis because multiple joints are typically affected. Carpal laxity syndrome has been described in puppies, which walk with the carpus in a hyperextended position.47 The cause is unknown but is speculated to be caused by asynchronous growth between the skeleton and the musculature. Long-term application of supportive splints for hyperextension is avoided because it may lead to muscle atrophy and increased tendon weakness (Figure 32-14). Treatment recommendations generally include balanced diet and controlled exercise on surfaces that provide good traction. Carpal arthrodesis may be a treatment option for hyperextension that does not resolve with exercise and nutrition, but this cannot be performed until the physes are closed. Carpal laxity syndrome is usually self-limiting, with a short duration and good prognosis. Weekly splint changes with ROM exercises of adjacent joints should be performed if possible.3 Passive range of motion and light activity are used to maintain normal tissue length and encourage normal joint movement. Removal of the splint is recommended within 3 weeks of the injury, because prolonged immobilization may delay healing and weaken the repaired tissue. Some tendon motion promotes remodeling of the peritendinous scar, which allows the tendon to glide. However, restricted activity must be enforced, because running or jumping could place catastrophic stress on the healing tissues and result in failure. By 6 weeks the tendons should have achieved adequate strength to sustain normal physiologic stress. At this point the focus of therapy is to restore ROM and strength. If there is contracture of muscle-tendon units, 3-MHz continuous-mode therapeutic ultrasound or hot packs with simultaneous stretching is indicated.3 Pelvic fractures account for a large percentage of fractures seen in veterinary practice. Because of the rigid, box-like anatomy of the canine pelvis, trauma usually results in two or more fractures of the pelvis (Figure 32-15, A). In general surgical repair is recommended for fractures within the weight-bearing regions of the pelvis, including the sacroiliac joint, ilial body, and acetabulum. Surgical repair is also recommended if there is neurologic impairment (e.g., possible sciatic nerve entrapment) or medial displacement of fracture fragments impinging on the pelvic canal. Surgical repair results in a quicker return to function with fewer changes secondary to tissue disuse, and the level of function will generally be superior. It is important that surgical repair be undertaken within the first 7 to 10 days after injury to minimize damage to soft tissues and nerves during reduction of the fractures. In some instances, conservative treatment in the form of cage rest may be adequate to allow healing. Examples of injuries amenable to conservative treatment include greenstick fractures of the body of the ilium, mild displacement of the sacroiliac joint with minimal pain or lameness, and fractures of the caudal 20% of the acetabulum. Although pubic and ischial fractures may appear quite severe on a radiograph, these injuries are rarely repaired because they are not part of the weight-bearing axis of the pelvic limb and will heal with rest. Repair of the injuries to the sacroiliac joint, ilium, and acetabulum generally results in adequate reduction and realignment of pubic and ischial fractures for healing. Sacroiliac joint luxations are surgically managed by placing one or more screws in lag fashion to compress the joint. The screw(s) should engage the body of the sacrum and be deeply seated into the bone, so that the screw engages at least 60% of the width of the sacrum (Figure 32-16). Fractures of the sacral body or wing can be challenging to repair, and concurrent nerve injuries are quite common.
Common Orthopedic Conditions and Their Physical Rehabilitation

Shoulder Conditions
Articular Fractures of the Shoulder
Goals
Treatment
Control inflammation
Cryotherapy immediately after surgery and then daily until inflammation resolves, particularly after exercise
Maintain range of motion and joint health
Passive range of motion and/or joint mobilizations for 3 to 4 weeks. Consider aquatic walking to minimize joint stress.
Add cavaletti walking after several weeks, depending on stability of repair.
Control pain
Nonsteroidal antiinflammatories plus other analgesics if needed. ± Transcutaneous electrical nerve stimulation
Strengthen muscle
Begin with controlled slow leash walking. Amount of activity depends on stability of repair and stage of healing. Short, slow leash walks for at least the first few weeks.
Osteochondritis Dissecans of the Shoulder

Figure 32-1 Osteochondritis dissecans of the caudal aspect of the head of the humerus. The right caudal humeral head is flattened and the linear density adjacent to the caudal humeral head is consistent with an osteochondral flap.
Goals
Treatment
Control inflammation
Cryotherapy immediately after surgery and then daily until inflammation resolves, particularly after exercise
Maintain range of motion and joint health
Passive range of motion for 1 to 2 weeks
Control pain
Nonsteroidal antiinflammatories for first few weeks, as needed
Strengthen muscles
Begin with controlled slow leash walking and progress over 2 to 4 weeks. Decrease activity if seroma or lameness develops. May begin jogging or swimming in 6 weeks.
Bicipital Tenosynovitis
Goals
Treatment
Control inflammation
Cryotherapy immediately after surgery and then daily until inflammation resolves, particularly after exercise
Promote tissue healing
Limited activity ± pulsed ultrasound ± cross-fiber frictional massage
Control pain
Analgesics ± transcutaneous electrical nerve stimulation ± laser
Strengthen soft tissues
May need several weeks of rest after acute injuries or surgery. Gradual progression of strength exercises, starting with eccentric exercises for involved muscles, such as walking downhill.
Maintain joint range of motion
Joint mobilizations or passive range of motion
Supraspinatus Tendinopathy
Medial Shoulder Instability
Fibrotic Contracture of the Infraspinatus Muscle
Teres Minor Strain
Elbow Conditions
Articular Fractures of the Elbow


Figure 32-3 Fracture of the lateral condyle of the humerus in a cocker spaniel. A, A-P view, B, Lateral view.
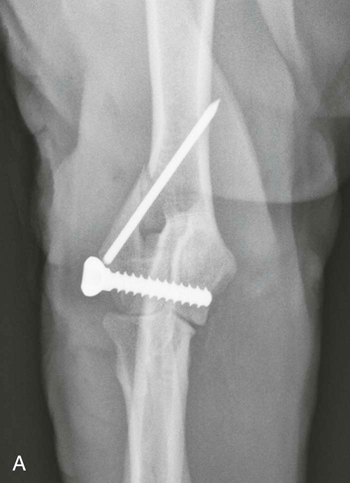

Figure 32-4 Repair of the fracture shown in Figure 32-3 with a transcondylar screw placed in lag fashion to compress the fracture fragments and a small pin in the lateral epicondyle to counteract rotational forces. A, A-P view, B, Lateral view.

Figure 32-5 Lateral postoperative radiograph of a radial fracture that was plated using a limited approach to minimize disruption of the soft tissues.
Elbow Dysplasia
Fragmented Medial Coronoid Process of the Ulna


Figure 32-7 Severe elbow osteoarthritis in a middle-aged dog suspected to be secondary to a previously unrecognized fragmented medial coronoid process. A, A-P view, B, Lateral view.
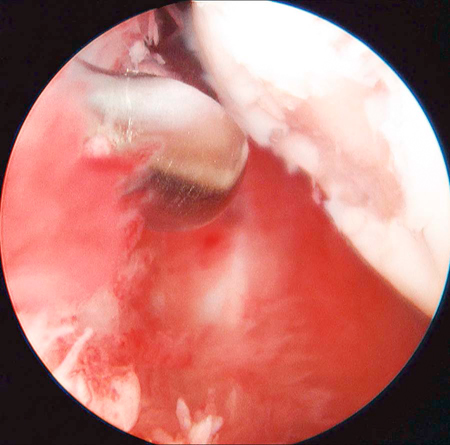
Osteochondritis Dissecans of the Elbow

Figure 32-8 Arthroscopic view of an erosion on the humeral articular cartilage that was created by a fragmented medial coronoid process. This is known as a kissing lesion and may be confused with osteochondritis.
Ununited Anconeal Process

Figure 32-9 Ununited anconeal process. An irregular radiolucent line is visible between the olecranon and the anconeal process on a flexed, lateral radiograph of the elbow, indicating that the anconeal process has not fused with the ulna.
Elbow Luxation
Antebrachial Conditions
Fractures of the Antebrachium


Figure 32-10 A, Distal radial fractures in toy breed dogs that are treated with external coaptation (splint or cast) have an increased risk of nonunion. B, In some cases, the radius and ulna may atrophy.
Contracture of the Flexors of the Antebrachium
Carpal, Metacarpal, and Phalangeal Conditions
Carpal, Metacarpal, and Phalangeal Fractures


Figure 32-11 When all four metatarsal or metacarpal bones have fractured, surgical repair is generally preferable to external coaptation. A, A-P view, B, Lateral view.


Figure 32-12 Metatarsal fractures that have been stabilized with bone plates and intramedullary pin. A, A-P view, B, Lateral view.
Carpal Hyperextension


Figure 32-13 Pancarpal arthrodesis performed in a patient with chronic carpal hyperextension. A, A-P view, B, Lateral view.
Trauma of the Superficial and Deep Digital Flexor Tendons
Pelvis and Hip Conditions
Pelvic Fractures


Figure 32-15 The pelvis usually has more than one fracture because of its box-like construction. Typically only the weight-bearing regions of the pelvis are surgically stabilized. A, V-D view prior to surgery, B, V-D view after surgical stabilization.

Figure 32-16 A sacroiliac luxation has also been stabilized with a screw. An ipsilateral hip luxation is repaired using a toggle pin as evidenced by the metal implant medial to the acetabulum and bone tunnel in the femoral head and neck.![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree