Chapter 15 Children’s Zoo Medicine
Zoonoses
This chapter is a general overview of common zoonotic diseases, diseases that may be transmitted from animal to human that are seen in children’s zoo and education animals. Although zoonotic disease is a concern for all areas of the zoo, it is most worrisome in areas in which the public has direct contact with the collection animals. The Association of Zoo and Aquariums has guidelines regarding the risk of disease transmission in animal contact areas developed over 10 years ago that still apply today.4 Topics discussed in this chapter are the responsibilities of the zoo veterinarian, general zoonotic disease transmission and prevention, and the most common zoonotic diseases found in children’s zoo and education animals, including discussion of the clinical signs, diagnostic modalities, and the means or mode of disease transmission. The material in this chapter should be regarded as a general overview of those diseases; the reader is encouraged to contact further sources for additional details and treatment options. The diseases presented in this chapter should in no way be considered the only diseases of concern because new zoonotic diseases and modes of transmission are continually being discovered.
Zoonotic Disease Transmission and Prevention
Transmission of zoonotic organisms from animal to person may occur through direct or indirect contact. Direct transmission includes contact with an animal’s mouth, saliva, contaminated coat, or feces. Indirect transmission includes contact with a contaminated environment, water, or food sources. Transmission may occur through ingestion, referred to throughout this chapter as fecal-oral, or through aerosol or skin contact.16
In animals, zoonotic organisms may be carried asymptomatically, making it impossible to determine when the animal is infected and infective. Zoonotic organisms may only be shed intermittently in the feces or through respiratory secretions, making it difficult to diagnose infectivity, and it may be impossible to clear animals of zoonotic organisms. Therefore, prevention of zoonotic disease transmission to the public is of utmost importance. The cornerstones of prevention are education of the staff and public, appropriate hand hygiene facilities (hand washing and hand sanitizer stations), appropriate exhibit design, and clear signage (Figs. 15-1 and 15-2). A retrospective study of hygiene and zoonotic disease transmission1 has found that hand hygiene education is the most important factor in the prevention of disease transmission. The study showed that nonantibacterial soap is more protective than antibacterial soap and that benzylalkonium chloride–based hand sanitizers are more protective than alcohol-based hand sanitizers for the prevention of respiratory disease. Therefore, the recommendation to wash hands immediately after leaving an animal exhibit is the most important step to reduce and prevent disease transmission.17
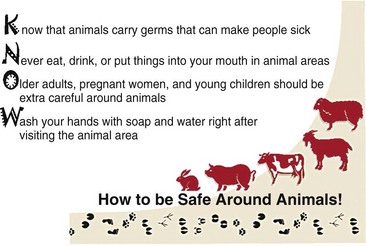
Figure 15-1 Educational poster for contact animal exhibits.
(Centers for Disease Control and Prevention: MMWR 58 (RR-5): 1-21, 2009, http://www.nasphv.org/Documents/AnimalsInPublicSettings.pdf).

Figure 15-2 Hand washing poster for contact animal exhibits.
(Centers for Disease Control and Prevention: MMWR 58 (RR-5): 1-21, 2009, http://www.nasphv.org/Documents/AnimalsInPublicSettings.pdf).
Ruminants
Bacterial Diseases
Enteric Bacterial Disease
This group of animals is usually asymptomatic carriers of enteric bacterial pathogens and will shed these organisms intermittently, contaminating the environment.16 At this time, laboratory testing is limited and culturing fecal specimens in an attempt to identify, screen, and remove infected asymptomatic animals may reduce the risk of transmission but cannot eliminate it. Antimicrobial treatment also does not eliminate the infection, does not prevent shedding, and cannot protect against reinfection; it may even prolong shedding and contribute to antimicrobial resistance.
Escherichia coli O157:H7 Infection
E. coli is a gram-negative, motile or nonmotile, facultatively anaerobic bacillus of the family Enterobacteriaceae. This discussion will focus on the enterohemorrhagic E. coli O157:H7, which is most commonly a food-borne pathogen but has been observed in petting zoos and farms. E. coli O157:H7 is part of the normal flora of ruminant livestock,6 with cattle being a major source of infection but sheep, goats, deer, and New World camelids are also asymptomatic carriers. Clinical signs are usually inapparent in adults and only rarely are clinical signs associated with disease in neonatal calves.21 The organism is shed in the feces, with shedding higher in the summer months, leading to more outbreaks from May to November. Any change in feed, feeding practice, or any stress that disturbs the normal intestinal flora could promote transient colonization with E. coli O157:H7, resulting in increased shedding. Diagnosis is difficult because the organism is part of the normal intestinal microflora and because fecal shedding is transient and intermittent. Transmission occurs via the fecal-oral route (e.g., contact with manure-contaminated hair coats, contact with environmental structures contaminated with feces).
Salmonella Infection
Salmonella spp. is a gram-negative, motile, facultatively anaerobic bacteria of the Enterobacteriaceae family. Clinical signs in children’s zoo ruminants range from asymptomatic carriers in adults to diarrhea and sepsis in kids, lambs, fawns, and calves. Salmonella spp. may also cause abortions, especially in sheep and goats, but does not appear to be a major problem in New World camelids.8 Ruminants may be latent carriers—bacteria lodge in the lymph nodes or tonsils so that the organism is not shed in the feces—or they may be passive carriers and shed Salmonella spp. intermittently in the feces, contaminating the environment. Latent carriers may become active shedders during times of stress.20 Diagnosis in ill animals is via fecal culture but it may not be possible to identify asymptomatic carriers. Transmission is via the fecal-oral route, similar to E. coli.
Campylobacter Infection
Campylobacter jejuni and C. fetus are curved, non–spore-forming, gram-negative, microaerophilic bacteria. C. jejuni is carried asymptomatically in ruminants and C. fetus is the most significant cause of abortion in sheep. Clinical signs in sheep include late-term abortions, stillbirths, and weak lambs. Ewes abort and then become immune but some may become persistently infected and shed the organism in feces. Diagnosis from ewes is by culture of the organism from placenta, fetal abomasal contents, and maternal vaginal discharge. Diagnosis of C. jejuni is through fecal culture but the organism maybe a normal inhabitant and be shed intermittently. Transmission to humans is through handling aborted fetuses or fecal-oral.15
Nonenteric Bacteria of Zoonotic Concern
Tuberculosis
Tuberculosis is a term that encompasses various diseases caused by bacteria of the Mycobacterium tuberculosis complex, including M. tuberculosis, M. bovis, and M. africanum, with M. bovis being the most common cause of human tuberculosis attributable to animals.12 All ruminants are susceptible to mycobacterial diseases and New World camelids appear to be very susceptible.8 Animals may be asymptomatic for long periods before clinical signs of enlarged lymph nodes, wasting, or emaciation become apparent. Diagnosis is via acid-fast staining of tissues, tissue culture, and the tuberculin skin test. The intradermal skin test may not be effective or practical for use in all species, but has been accepted by the USDA for identification of M. bovis in cattle, bison, goats, and captive cervids. Other diagnostic methods rely on the cellular immune response and are performed in vitro (e.g., lymphocyte blastogenic assays or interferon gamma tests), with results comparable to those obtained with intradermal tests. Mycobacterial culture is still considered to be the gold standard diagnostic test. Transmission of the disease is via aerosol or ingestion but may be spread through the contamination of cuts and abrasions. Mycobacteria are viable for several months in feces or in animal carcasses.
Q Fever
The causative agent of Q fever is Coxiella burnetii, a gram-negative coccobacillus. Clinical signs in cattle, sheep, and goats range from asymptomatic carriers to animals with mild fevers and abortion. Diagnosis is based on placental findings, serology, and isolation of the organism. Transmission is via inhalation, handling contaminated animals, and contact with contaminated body fluids.14 This organism is mostly problematic for institutions with indoor birthing exhibits.
Other Nonenteric Bacteria
The following organisms have the ability to cause disease in humans but the risk of transmission from animals is low. Leptospira interrogans and its serovars infect cattle, sheep, goats, deer, and New World camelids. Clinical signs range from asymptomatic to abortions, anorexia, and sepsis (especially in neonates), with signs of intravascular hemolysis. Diagnosis may be made by changes in laboratory values (e.g., anemia, hyperbilirubinemia, hemoglobinuria, hemoglobinemia), identifying spirochetes on dark field microscopy of urine or plasma, or rising antibody titers. Transmission occurs by contact with infected urine, aborted tissues, contaminated ponds and water sources, and other body fluids.15 Listeria monocytogenes occurs equally in sheep, goat, cattle, and New World camelids. Clinical signs include depression and anorexia, which progress to more complex neurologic signs, including facial and vestibular lesions. There are no specific diagnostic tests. Listeria may be shed by sick, recovering, or clinically normal animals in milk and feces for long periods.8 This is usually a food-borne pathogen but may be transmitted through the fecal-oral route. Brucellosis is caused by Brucella melitensis in goats and sheep and B. abortus in cattle. It is not considered a major disease of New World camelids but is a problem in reindeer. Abortion is the most common clinical sign but ruminants may also present with mastitis, lameness, and/or orchitis.9 Diagnosis is made primarily by serology. Transmission is via contact with infected materials through breaks in the skin, ingestion, or inhalation. Chlamydophila psittaci is found in sheep, goats, and cattle and may cause abortion, pneumonia, keratoconjunctivitis, epididymitis, and polyarthritis.7 Diagnosis is through culture of the organism and serology. Transmission is fecal-oral or through contact with infected placentas, but the mammalian forms of Chlamydiophila do not appear to be as zoonotic as avian strains.
Viral Diseases
Rabies
Rabies, a lyssavirus, may infect all mammals. Ruminants and New World camelids display a variety of clinical signs, including depression, anorexia, nystagmus, muscle tremors, lameness, ataxia, and posterior paresis. These animals rarely exhibit the aggressive forms of rabies and the disease will usually progress as an ascending paralysis. Fortunately, New World camelids are not able to spit when suffering from rabies.8 Diagnosis is via direct fluorescent antibody testing on the brain of a suspect case. Rabies always needs to be included on a rule-out list in an animal with neurologic signs. Transmission to people is via a bite or saliva from infected animals that gets into an open wound.16 All animals demonstrating neurologic signs should immediately be removed from animal contact areas.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


