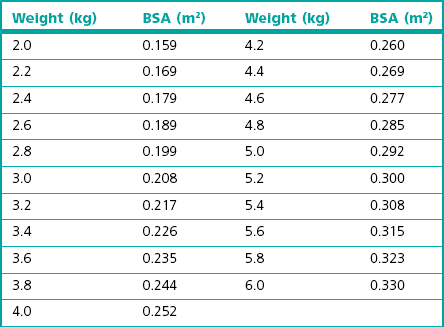
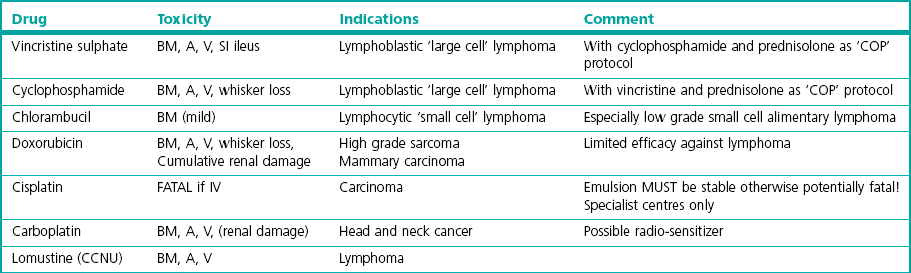
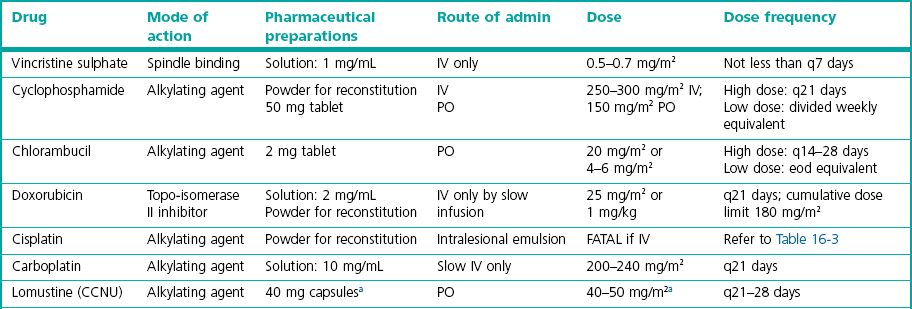
Chapter 16 Having given this stark introduction, chemotherapy can help control certain cancers and thereby benefit those individuals with an improved quality of life. This chapter therefore aims to give an insight into some of the drugs that are used, their potential side effects and the management of such problems, and the situations where cytotoxic drugs have been shown to have efficacy in cats. For further information the reader is referred to specialist oncology textbooks.1–4 Another property of tissues that influences efficacy of cytotoxic drugs is the growth rate (Box 16-1). The rate of clinical tumor growth and the mitotic index given by histology may provide surrogate information about the tissue growth rate. In theory, tumors with a high growth fraction and short cell cycle time are the most sensitive to cytotoxic agents. Lymphoblastic lymphoma is an example of a sensitive cell type of this nature, as the cells often exhibit a high mitotic rate, and hence this form of tumor in cats frequently responds to chemotherapy. Cytotoxic drugs are used in several scenarios (Box 16-2). In practice, the probability of curing most cancer in dogs or cats with cytotoxic drugs is low because the actual range of tumors that respond to chemotherapy is quite limited, a fact especially true in cats. There are several principles that should be followed when selecting drugs for chemotherapy (Box 16-3). The surface area is derived from the weight by equation in Box 16-4 (see also Table 16.1).The dose interval depends on which drug is being used, the dose given and the recovery time from adverse effects. For most cytotoxic drugs given as a ‘high dose’ bolus the average time to complete recovery is day 21 following the neutropenic nadir at day 5 to 7, and therefore a dose interval of three weeks is appropriate. However, some drugs (e.g., lomustine and, to a lesser extent, carboplatin)5,6 have a second weaker nadir around day 20 and may warrant a four week cycle, so it is important to be aware of these individual drug variations when designing a therapeutic plan for individual patients. Drugs may also be given at a lower dose more frequently to give a chronic exposure. There is a long list of drugs that have anti-cancer effects. Although a dose for many of the drugs suitable for cats can be found in the literature, actual documented evidence of efficacy is either non-existent or at best limited to anecdotal single case reports so this chapter will focus only on the agents which have a reasonably good evidence base for their recommended use. Table 16-2 summarizes the pharmaceutical aspects and dosing issues; Table 16-3 lists the toxicity and indications of the drugs that are used with some frequency in cats. Table 16-2 Summary of anti-cancer drugs: dosing aspects IV, intravenous; PO, per os; eod, every other day. aSpecialist re-formulation to 10 mg capsules is necessary for clinical use.
Chemotherapy
Cancer chemotherapy
How anti-cancer drugs work
When chemotherapy is indicated
Drug dosing issues
Anti-cancer drugs
Side effects and their management
Chemotherapy