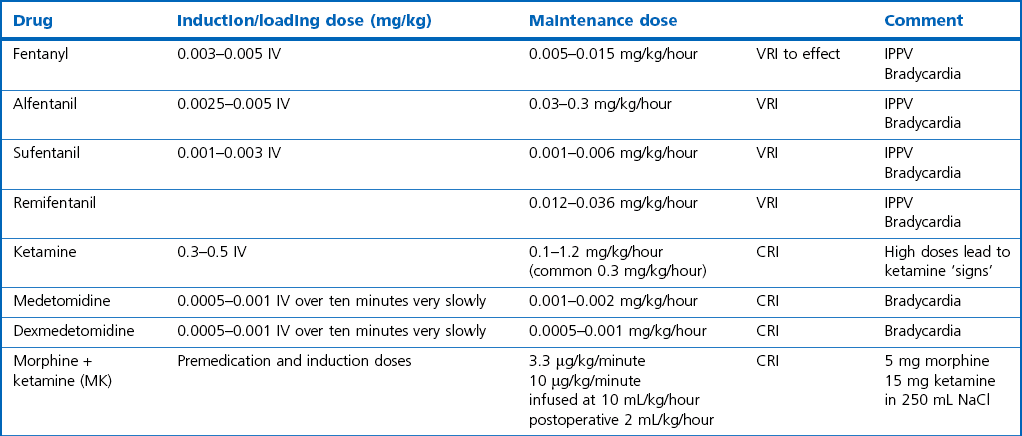
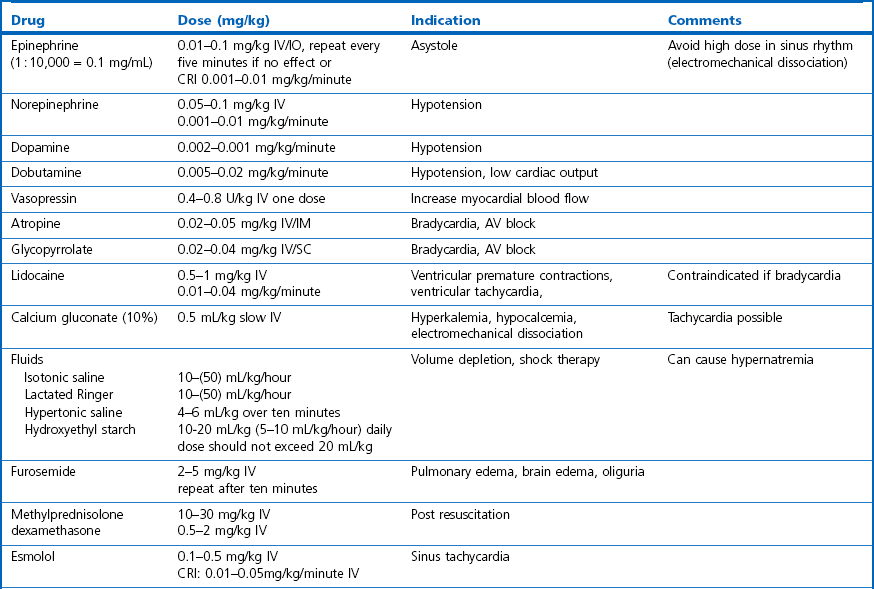
Chapter 2 Choosing an anesthetic protocol for a specific patient depends on the pre-anesthetic examination, the presence of systemic disease, and type and duration of the intended procedure. When anesthetizing a diseased cat it is important to take the disease process and its pathophysiology into consideration. A young healthy cat might be able to compensate for the effects of drugs, whereas a compromised animal might not be able to compensate. For a more detailed description of general anesthesia techniques, drugs, and equipment the reader is referred to Chapters 17 and 18 of Feline Orthopedic Surgery and Musculoskeletal Disease.1,2 This chapter is designed to augment the previously mentioned chapters. To avoid repetition this chapter will concentrate specifically on anesthesia and analgesia of cats with intercurrent systemic disease that might have implications for anesthetizing them for surgery and cats with diseases of specific organ systems and the different considerations that might arise in such situations. Excitement or stress caused by excessive restraint will induce high levels of circulating catecholamines, which will not be tolerated by severely compromised cats. Stress will lead to increased anesthetic requirements and consequently more severe cardiovascular depression. Pre-medication can help alleviate this stress. A full description of drugs that can be administered in cats and their indications is described in Feline Orthopedic Surgery and Musculoskeletal Disease.1 Injectable anesthetics can be used for induction of anesthesia followed by inhalational anesthesia for maintenance or they can be used as the sole anesthetic agent (total intravenous anesthesia [TIVA]). Inhalation anesthesia is still the preferred technique for producing general anesthesia for prolonged and invasive surgical procedures because the depth of anesthesia can easily be adapted and drug accumulation is not a problem with modern inhalation anesthetics. Modern protocols use the principle of balanced anesthesia, with a combination of different analgesic, sedative–hypnotic and muscle-relaxing drugs, with the aim of reducing the concentration of volatile anesthetics required (Table 2-1). Since the recent publication of the Feline Orthopedic Surgery and Musculoskeletal Disease textbook,1,2 the variety of drugs available for anesthesia and analgesia in cats has changed very little. However, the use of tramadol in small animal practice has risen dramatically. It has the advantage of oral administration. A new non-steroidal anti-inflammatory drug (robenacoxib) is licensed for use in cats,and anti-epileptic agents (gabapentin and pregabalin) are being used more commonly in small animal practice. These drugs will be described below. Tramadol is an atypical opioid with weak µ-receptor binding activity in combination with serotonin and noradrenaline reuptake inhibition as its analgesic mechanism. Cats produce the active metabolite, which is responsible for the opioid analgesia, more effectively than dogs. Oral bioavailability is high in cats (93%). For cats a dose of 1–2 mg/kg IV and oral dosing of 2–4 mg/kg twice a day has been recommended clinically. In experimental animals 2–4 mg/kg was effective and dosing every six hours seemed to be necessary to maintain analgesia at a maximal effect.3 The liquid formulation often contains peppermint oil, which induces copious salivation and is not well liked by cats. Robenacoxib is a selective COX-2 inhibitor in the cat (ex vivo and in vivo) and is licensed for the treatment of acute musculoskeletal pain and postoperative pain after soft tissue surgery in the cat. Because of the high degree of COX-2 selectivity the gastrointestinal toxicity is low. Maximal plasma concentrations in the cat are reached after 0.5 hours and one hour after oral and subcutaneous application, respectively.4,5 In a systemically healthy patient any isotonic crystalloid solution (i.e., lactated Ringer solution, saline) can be used at a rate of 5–10 mL/kg/hour depending on the expected fluid and blood loss during the planned procedure. For prolonged procedures without opening major body cavities the lower rate should be chosen in cats to avoid overzealous dilution and disturbance of colloid osmotic pressure and pulmonary edema formation. A large study on small animal perioperative mortalities found an increased anesthetic risk for cats receiving intravenous fluids.6,7 This might be related to the fact that in practice only diseased, high-risk feline patients will be treated with infusions; however, it might also indicate overinfusion when the rate is not controlled properly which can occur when using large giving sets. Whole blood is recommended with acute hemorrhage and erythrocyte concentrate for treatment of chronic normovolemic anemia, to avoid volume overload. If stored blood is used in planned procedures the transfusion should be scheduled the day before surgery to allow for compensation for the changes in oxygen-carrying capacity of the stored products. In cats, blood transfusion requires blood typing or cross-matching even with the first transfusion because of preformed antibodies (Chapter 5). Insulin administration after fasting increases the risk of hypoglycemia. However, insulin activity is necessary to enable metabolism and uptake of nutrients by the tissues. In addition, preoperative stress with the release of catecholamines and corticosteroids increases glucose levels and insulin requirements. Therefore, insulin should not be withheld in the preoperative period. The usual recommendation on the proportion of the animal’s usual insulin dose varies from one half to one quarter of the usual dose. Ideally this is adapted according to the glucose levels on the morning of surgery (Table 2-3). Table 2-3 Blood glucose management during anesthesia in diabetic patients The glucose target range during surgery lies between 8.3 and 14 mmol/L; glucose monitoring during surgery is recommended every 30 to 60 minutes. A 2.5–5% dextrose infusion is given according to the cat’s systemic glucose concentrations (Table 2-3). There is an increasing incidence of obesity in domestic cats8 (Fig. 2-1). In obese animals the veterinarian is faced with a variety of general problems as well as specific anesthesia-related problems. Venous access as well as palpation of arterial pulses is impaired. Increased fat in the throat region may make endotracheal intubation more difficult and may also increase the risk of airway obstruction. Increased superficial fat obtunds thoracic auscultation and obscures landmarks for locoregional techniques and may act as a thermal insulator and increase the risk of heat stress. The goals of the anesthetic protocol in obese cats are listed in Box 2-1. Patients with skin and adnexal problems (Chapters 17 to 22) may not have any specific anesthetic requirements related directly to the lesions. However tumors are often seen in older cats who are prone to problems such as hyperthryroidism, diabetes and obesity. Wounds or masses may be infected or ulcerated and therefore cause systemic illness and require preoperative stabilization prior to anesthesia (Chapter 1). If masses are large then analgesia after resection is essential. Consideration can be given to using wound infusion catheters (Chapter 11) in addition to multimodal analgesia with non-steroidal anti-inflammatory drugs, opioids and other adjuncts such as ketamine and the alpha-2 agonists. A brachial plexus block in the cat is performed under general anesthesia. A brachial plexus block at the height of the shoulder is suitable for operations on the front limb within or distal to the elbow. A 22G 5 cm needle is inserted medial to the shoulder joint and advanced parallel with the spine directed towards the costochondral junction of the ribs. If no blood can be aspirated, lidocaine or bupivacaine diluted to a volume of 5 mL to facilitate spread is injected during withdrawal to reach the radial, ulnar, median and musculocutaneous nerves (RUMM block). The use of a nerve stimulator to locate the nerves and set specific depots improves the results (Fig. 2-2). Fenestrated wound catheters (Chapter 11), can be used for analgesia of defined wound regions, for example after ear canal ablation or large tumor excisions like fibrosarcoma removal (Chapter 17). Commercial systems come in different lengths with bacterial filters, a flow restrictor and a balloon pump (i.e., ON-Q PainBuster, Kimberly Clark or Diffusion/Wound catheter, MILA International Inc. Erlanger, KY, USA), but it is also possible to purchase the catheter and filter without the pump. The catheter can also be constructed from red rubber or polyethylene tubing (Fig. 2-3). The elastomeric reservoir (pump) delivers fluid at a rate of 0.5–5 mL/hour; alternatively, a syringe pump can be used in non-ambulatory patients. The catheter is usually placed subcutaneously during surgery in the desired area and can either be continuously perfused with a local anesthetic (lidocaine (1%) 0.2–0.4 mg/kg/hour) or repeated boluses of a long-acting local anesthetic can be given intermittently (1 mg/kg bupivacaine [0.25%] first dose followed by 0.5 mg/kg every six hours for one to two days).9 This provides useful adjunctive analgesia for both abdominal and thoracic procedures. Contraindications for epidural anesthesia are septicemia, coagulation disorders, hypovolemia, shock, skin infections at the puncture site and deformity, dislocations or fractures of the spine or pelvis. Possible complications include local skin infection, meningitis and trauma to the spinal cord, but these are rare. The procedure is described in Chapter 18 of Feline Orthopedic Surgery and Musculoskeletal Disease.2
Anesthesia and analgesia for general surgery
General considerations
Sedation
Anesthesia
New drugs
Tramadol
Robenacoxib
Fluid administration
Systemic and metabolic disorders
Anemia
Diabetes
Blood glucose in the morning (pre insulin)
Insulin
Dextrose (2.5–5%) infusion
<5.5 mmol/L
No
Start 2–4 mL/kg/hour
5.5–11 mmol/L
One-quarter of the usual dose
Start 2–4 mL/kg/hour
>11 mmol/L
Half the usual dose
No infusion necessary until glucose <8 mmol/L
Obesity
Skin and adnexa
Brachial plexus block
Wound catheter infusion systems
Abdominal surgery
Epidural anesthesia
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree