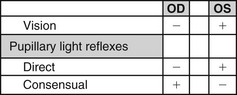
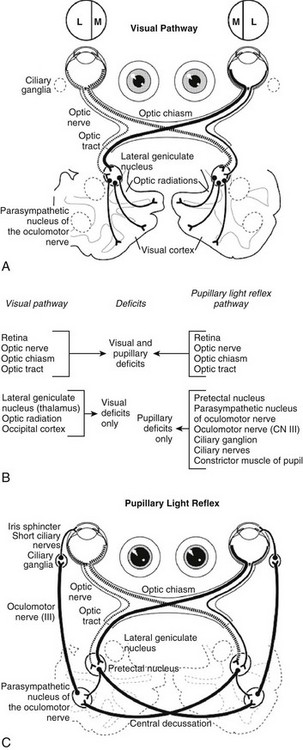
Web Chapter 80 A complete ophthalmic examination (see Chapter 242), including measurement of intraocular pressure, examination of the cranial nerves, and a full physical examination, always should be done. Recording all examination findings is essential (Web Figure 80-1) to compile the information that must be reviewed before making a decision regarding the cause of the neuro-ophthalmic defect or anisocoria. Web Figure 80-1 Grid to record visual status and pupillary light reflexes (PLRs). Possible entries include +, normal; −, absent; I, incomplete; and M, minimal. The latter two entries are used to designate degrees of constriction in the PLRs (e.g., the “incomplete” designation may be used in cases of iris atrophy). The example in the chart depicts the responses for a lesion of the right retina or prechiasmal optic nerve. OD, Right eye; OS, left eye. Pupil size (and shape in the cat) is determined by the balance between parasympathetic and sympathetic innervation of the iris. Although emotional and other non–neuro-ophthalmic factors can affect this aperture, pupil size depends in large part on the amount of light illuminating the retina and the afferent and efferent pathways of the PLR. An understanding of the anatomy of the PLR is essential (Web Figure 80-2, B and C), along with recognition that the PLR reflex is subcortical (without cerebral cortical involvement) and that the reflex is not an indicator of vision. The response of only a few photoreceptors is required for the PLR to occur. Web Figure 80-2 Deficits caused by lesions of the visual and pupillary light reflex pathways. (B, From Oliver JE, Lorenz MD, Kornegay JN: Blindness, anisocoria, and abnormal eye movements. In Handbook of veterinary neurology, ed 3, Philadelphia, 1997, Saunders, p 274, with permission.) The afferent arm of the PLR for each eye consists of the retina, optic nerve, optic chiasm, and optic tract. Nerve fibers originating in the medial retina decussate to the opposite optic tract, whereas fibers from the lateral retina remain in the ipsilateral tract. In the dog approximately 75% of the optic nerve fibers decussate to the contralateral optic tract. In the cat approximately 65% of the optic nerve fibers decussate. The optic tracts carry impulses beyond the decussation and include both sensory visual fibers and pupillomotor fibers that differ according to their destinations. This fact is useful for localizing lesions by noting the presence or absence of vision and PLR in each eye. The pupillomotor fibers progress to the pretectal nucleus, and from there the majority of these fibers decussate to the parasympathetic nucleus of the oculomotor nerve (previously known as the Edinger-Westphal nucleus) on the contralateral side. This second decussation marks a return to the side of the originating (light) impulse. In contrast, the visual fibers proceed from the optic tract sequentially to the ipsilateral lateral geniculate nucleus, the optic radiation, and the occipital (visual) cortex. Therefore lesions that cause anisocoria and affect both PLRs and vision can be localized to the retina, optic nerve, optic chiasm, or optic tract (see Web Figure 80-2). By contrast, lesions affecting vision, but not PLRs, are located in the lateral geniculate nucleus, optic radiation, or occipital cortex.
Anisocoria and Abnormalities of the Pupillary Light Reflex
The Neuro-ophthalmic Examination
Functional Anatomy of the Pupillary Light Reflex
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


