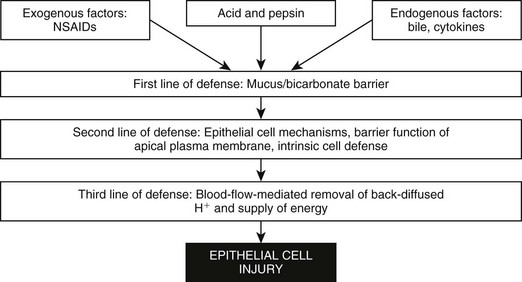
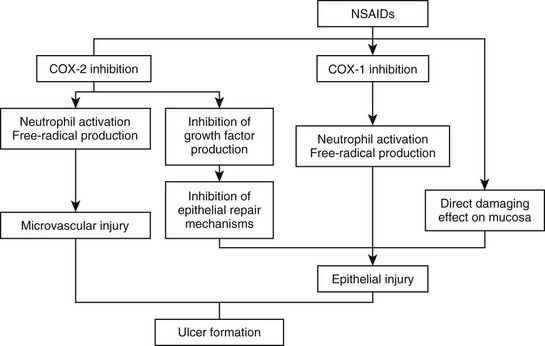
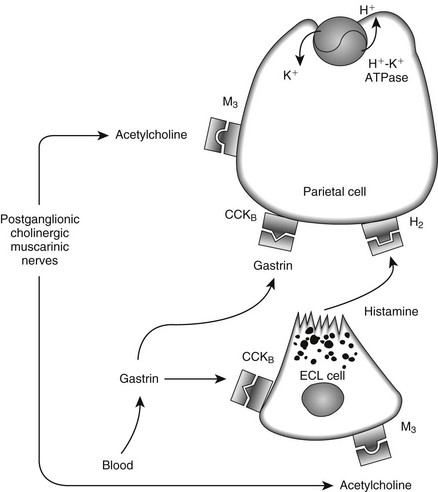
Web Chapter 52 Understanding the treatment and prevention of peptic ulcers requires an understanding of gastric secretion and mucosal protection. Acid is produced by the H+-K+-adenosine triphosphatase (ATPase) enzymes in parietal cells, which are located in the oxyntic glands. H+-ions are pumped into the lumen in exchange for K+; the latter accumulates in the cell and moves down the electrochemical gradient, leaking across the luminal and basolateral cell membranes. Stimulation of the parietal cell occurs via acetylcholine (M3), gastrin (CCKB), and/or histamine (H2) receptors on the basolateral membrane via second messengers (Web Figure 52-1). A further hormone, tentatively named enterooxyntin, seems to stimulate acid secretion as well (Johnson, 2001). There are several interactions between these secretagogues, and potentiation occurs if two or more stimulants act simultaneously, meaning that the sum of the response exceeds that of each individual response. Histamine is found in enterochromaffin-like (ECL) cells within the lamina propria of the gastric glands. ECL cells have receptors for gastrin and acetylcholine. Web Figure 52-1 Physiologic mechanism of gastric acid secretion. The parietal cell contains receptors for gastrin, acetylcholine, and histamine. In addition, gastrin and acetylcholine release histamine from the enterochromaffin-like cell (ECL cell). Several mechanisms underlie the remarkable abilities of normal gastroduodenal mucosa to defend itself against injury from acid/pepsin activity in gastric juice and to rapidly repair injury when it does occur. These mechanisms entail three lines of defense: preepithelial, epithelial, and subepithelial (Web Figure 52-2). Factors that play a role in maintaining mucosal protection against the ulcerogenic effects of acid and pepsin are mucus; blood flow; bicarbonate secretion; cellular renewal; and chemical factors such as prostaglandins, gastrin, and epidermal growth factor. Surface mucus cells secrete mucoproteins in response to chemical or physical stimuli. This secreted gel entraps alkaline components, neutralizes a certain amount of acid, and prevents pepsin from coming into contact with the mucosa. Prostaglandins play a key role in protecting the gastric mucosa against injury caused by a variety of necrotizing agents. Prostaglandins exert two actions: inhibition of acid secretion and enhancement of mucosal resistance to injury by mechanisms independent of acid secretory inhibition, also called cytoprotection. A variety of causes for peptic ulcers in dogs and cats have been reported. Although nonsteroidal antiinflammatory drugs (NSAIDs) are thought to be the most common cause, the true incidence of gastrointestinal side effects of NSAIDs in dogs is unknown. Only one case of NSAID-induced ulceration has been reported in a cat. NSAIDs are thought to cause gastrointestinal mucosal injury by several mechanisms. Primarily these drugs impair prostaglandin-dependent mucosal protective mechanisms by nonselective inhibition of two isoforms of cyclooxygenase (COX), COX-1 and COX-2. However, a direct correlation is lacking between the extent of COX inhibition and NSAID-induced gastrointestinal damage (Web Figure 52-3). COX-1 inhibition leads to reduced bicarbonate secretion, reduced mucus formation, and vascular actions. Other effects unrelated to prostaglandin synthesis include a “topical” action of NSAIDs on the gastric mucosa, involving mitochondrial injury (“uncoupling”) by a direct toxic action. All commonly used NSAIDs, whether COX-2–specific or not, have been found to cause gastric lesions, although true ulcers with sufficient depth to reach or penetrate the muscularis mucosa seem to be rare. In the largest study of gastric ulcers in dogs, only 4 of 43 cases were thought to have peptic ulcers caused primarily by NSAIDs (Stanton and Bright, 1989). However, close temporal association of various NSAIDs and steroids must be avoided because an increased likelihood of gastric ulceration has been reported (Lascelles et al, 2005).
Gastric Ulceration
Physiology
Causes
< div class='tao-gold-member'>
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree