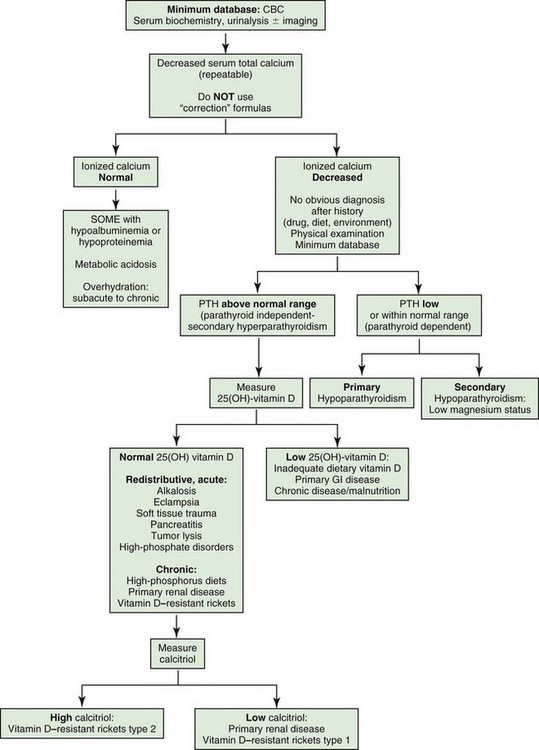
Web Chapter 22 Hypoparathyroidism is a state of absolute or relative deficit of parathyroid hormone (PTH) secretion that can be permanent or transient. Hypocalcemia and clinical signs referable to low ionized calcium concentration are the hallmarks of advanced hypoparathyroidism. This endocrine disorder is an uncommon cause of hypocalcemia in dogs and cats (Web Box 22-1), but it is the only condition requiring acute and chronic treatment to alleviate clinical signs associated with hypocalcemia. Hypoparathyroidism in dogs is most commonly an idiopathic or primary condition, whereas surgical removal or injury during thyroidectomy to correct hyperthyroidism is the most common cause in cats. Rarely, transient hypoparathyroidism can occur after correction of long-standing hypercalcemia (e.g., subsequent to removal of an adenocarcinoma of the apocrine gland of the anal sac or treatment of lymphosarcoma). In humans with idiopathic hypoparathyroidism, a variety of mutations have been identified that affect PTH production or PTH receptors (pseudohypoparathyroidism), but these conditions have not been described in dogs or cats. The treatment for hypoparathyroidism is the same, regardless of cause or genetic defect. Clinical signs of primary hypoparathyroidism from hypocalcemia include seizures, muscle tremors or fasciculations, muscle cramping, stiff gait, and behavioral changes (restlessness, excitation, aggression, hypersensitivity to stimuli, disorientation) (Web Box 22-2). Most seizures resolve without treatment but often recur despite treatment with anticonvulsants. Growling attributable to pain or behavior change and intense rubbing of the face with the paws or on the ground commonly are observed. These signs are attributed to either paresthesia or pain from facial muscle spasms. Hyperthermia may be caused by increased muscular activity; lethargy, anorexia, and weakness may be noted, especially in cats. Polyuria and polydipsia occur in some cases as a result of psychogenic mechanisms or renal injury from hypercalciuria. Anterior and posterior lenticular cataracts occur in some affected dogs and cats, and prolapse of the third eyelid sometimes is seen with acute hypocalcemia in cats. Vomiting, abdominal pain, and diarrhea occasionally have been noted in patients with primary hypoparathyroidism. Hypocalcemia has numerous causes (see Web Box 22-1). The approach to diagnosis of the cause of hypocalcemia is described in Web Figure 22-1. Primary hypoparathyroidism is the only disorder characterized by hypocalcemia, elevated serum phosphorus, and low PTH concentration, along with normal renal function. Decreased serum calcium with increased serum phosphorus may be seen in nutritional or renal secondary hyperparathyroidism, after phosphate-containing enema administration, and in tumor lysis syndrome; however, PTH concentration is increased in all of these conditions. A presumptive diagnosis of hypoparathyroidism can be made on the basis of decreased serum calcium, high serum phosphorus, normal renal function, and the absence of an obvious alternative diagnosis. The definitive diagnosis of hypoparathyroidism requires the finding of a PTH concentration below or within the reference range concurrently with hypocalcemia because hypocalcemia should provide a strong stimulus to the normal parathyroid glands to secrete PTH to a level above the reference range. Primary hypoparathyroidism requires lifelong treatment; thus confirmation of the diagnosis with PTH measurement is recommended highly. Because magnesium depletion can cause functional hypoparathyroidism measurement of serum ionized magnesium concentration also is recommended because more than 75% of dogs and cats with primary hypoparathyroidism have marginal or low serum ionized magnesium concentrations.
Treatment of Hypoparathyroidism
Pathophysiology and Differential Diagnosis
Clinical Signs
Diagnosis
< div class='tao-gold-member'>
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree