CHAPTER 40 Cardiovascular Pharmacology
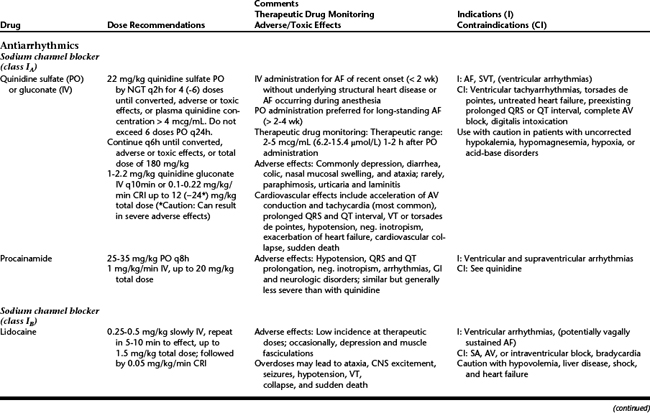
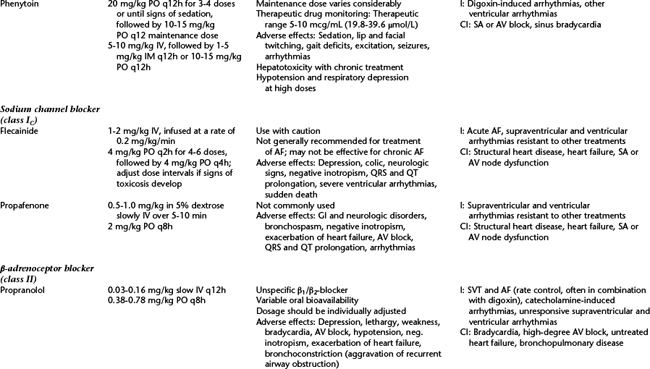
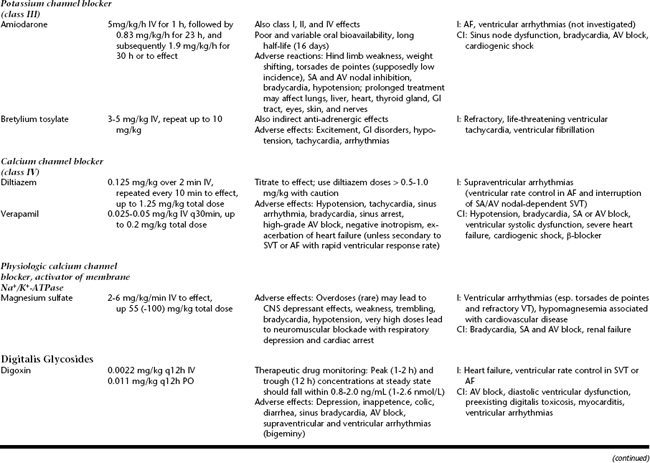
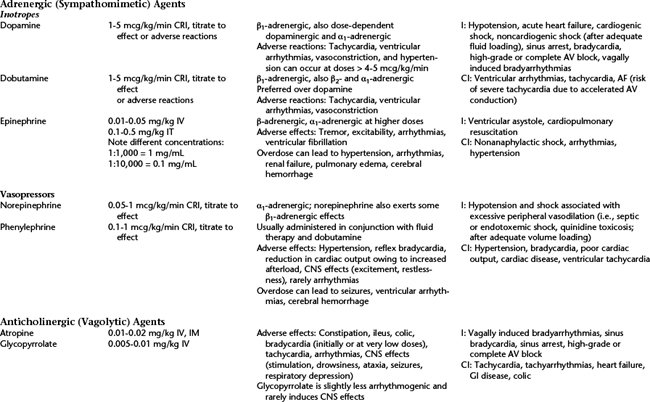
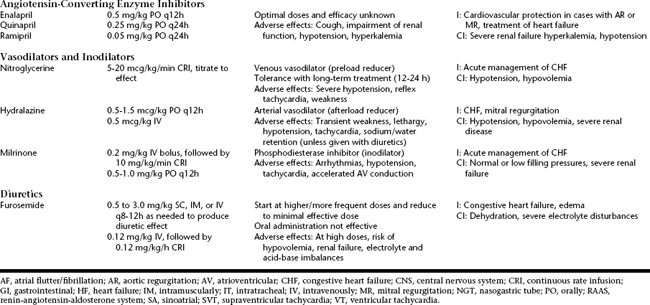
Compared with human medicine, the therapeutic options for the treatment of cardiovascular disease in horses are limited to a relatively small group of agents (Table 40-1). Most recommendations for the use of cardiovascular agents in horses are based on empirical data rather than scientific evidence, and the efficacy and safety of most drugs have not been well investigated in horses. Generally, cardiovascular drugs are used for treatment of arrhythmias, treatment of heart failure, and support of cardiovascular function in a variety of clinical situations. Prophylactic therapy or long-term treatment of horses with subclinical disease (to slow progression of disease) is rarely performed, mostly because of a lack of evidence of clinical efficacy, doping concerns in sports horses, and financial constraints.
ANTIARRHYTHMICS
Class IA Drugs
Quinidine
Quinidine is used primarily for conversion of atrial flutter or atrial fibrillation (AF) to sinus rhythm, with a reported efficacy as high as 80% to 90%. Horses with AF and high resting heart rate, evidence of impaired left-ventricular systolic function (based on echocardiography), or congestive heart failure should be pretreated with furosemide (to control edema) and digoxin (to control heart rate and improve systolic left-ventricular function) as necessary. Adverse effects of quinidine are common, even at therapeutic plasma concentrations. Prolongation of the QRS complex of greater than 25% of baseline indicates toxic plasma concentrations (i.e., greater than 5 mcg/mL). In horses with an accelerated atrioventricular conduction (heart rate greater than 100 beats/minute), the rate may be controlled by intravenous (IV) administration of digoxin, diltiazem, or propranolol with close monitoring of clinical response, ECG changes, and blood pressure. Diltiazem and propranolol may enhance hypotension and negative inotropism and should be administered with caution. If the rate is sustained in excess of 150 beats/minute or severe hypotension occurs, administration of IV sodium bicarbonate (1 mEq/kg) should be considered to antagonize the sodium channel blocking effects of quinidine. Forced diuresis using fluids and diuretics may enhance renal excretion of the drug. Severe hypotension is treated with IV fluids or colloids and phenylephrine or norepinephrine. Ventricular arrhythmias are treated with lidocaine and magnesium sulfate. Hypokalemia and hypomagnesemia may increase the risk of torsades de pointes and should be prevented.