Chapter 20 Cardiovascular emergencies associated with anaesthesia
INTRODUCTION
Despite the utilization of new anaesthetic drugs, techniques and equipment and improved patient monitoring, the risk associated with general anaesthesia in horses has not significantly decreased over the past 10 years. The Confidential Enquiry into Perioperative Equine Fatalities (CEPEF), a prospective epidemiological multi-centre study, has furnished accurate perioperative mortality rates after extensive analysis of over 50 000 anaesthetic records.1–5 The overall perioperative mortality rate is 1.6–1.9% and if anticipated “high-risk” horses that underwent emergency abdominal surgery (“colics” and dystocias) are excluded from the analysis, the anaesthetic-related death rate is still alarmingly high at 0.9%.3–5 This is 4 to 5 times higher than the mortality rate recently established for dogs and cats using a similar data collection technique6. Further analysis of the unanticipated deaths in healthy horses undergoing elective procedures reveals that the commonest cause of death (32–33%) is due to cardiac arrest or irreversible cardiovascular collapse, with fractures and myopathies being the second and third reasons.4,5 Cardiac arrest represents one extreme end of the spectrum of cardiac emergencies that can occur in horses. Other common anaesthetic-related complications include cardiac dysrhythmias, hypotension and hypertension. The causes, recognition, prevention and treatment of these problems will be discussed.
RISK FACTORS
The CEPEF identified several risk factors that should influence the anaesthetic management of horses. These factors include the choice of premedicant agent and the maintenance technique4; these will be discussed in greater detail later in this chapter. Risk of dying increased with duration of anaesthesia;3 therefore, speed is of the essence and all procedures should be well planned and all stages expedited efficiently. Other risk factors included age; young foals and older horses were at higher risk.4
PREOPERATIVE EVALUATION AND PREMEDICATION
Most horses scheduled for surgery, whether for an elective or emergency procedure, do not have cardiac disease and these patients are the focus of this discussion. Horses with cardiac disease are not good candidates for surgery. However, any patient with heart disease should be stabilized as much as possible prior to anaesthesia (these conditions including atrial fibrillation are discussed comprehensively elsewhere in this book, see Chapters 13 and 14). Standing sedation and local anaesthetic techniques should always be considered in these animals and the advent of laparoscopic surgery has expanded the scope of procedures that can be performed in conscious horses.
Before anaesthetizing any equine patient a thorough clinical examination with an emphasis on the respiratory and cardiovascular system is mandatory. Bradydysrhythmias may be detected in as many as 25% of horses at rest but most are categorized as physiological and considered benign. The resting adult horse has high vagal tone with normal heart rates ranging from 25 to 45 bpm. At low heart rates, first- or second-degree atrioventricular (AV) block, sinoatrial (SA) block, wandering atrial pacemaker, sinus bradycardia and sinus arrhythmia are often present (see Chapters 6 and 13). In a pre-anaesthetic work-up, one should confirm that exercise or excitement increases the heart rate and abolishes these dysrhythmias; careful auscultation and palpation of a peripheral pulse is usually sufficient. If they are not easily overridden, an electrocardiogram (ECG) and further investigation is warranted. The administration of atropine is not recommended as a first step to counteract vagal tone because of the CNS excitement and gastrointestinal stasis that may result from its use.7 If surgery is elective, it should be postponed until a definitive diagnosis is reached. In an emergency situation there is no option but to proceed with caution. If an anticholinergic is used, glycopyrrolate would be preferable as it has fewer undesirable side effects.
Horses, including foals, should be adequately sedated prior to induction of anaesthesia. Omitting premedication is associated with a striking increase in the risk of death.4 The benefits of sedation include a more manageable patient and increased safety for personnel, decreased excitement and release of endogenous catecholamines that may produce dysrhythmias, a reduction in requirements of induction and maintenance agents that have potent cardiopulmonary depressive effects, smoother maintenance of anaesthesia and a calmer recovery. Does the choice of premedicant agent matter? The most commonly used premedicants are the phenothiazine acepromazine and the α2-adrenergic agents xylazine, detomidine and romifidine. More recently medetomidine has been used in horses although it has no market authorization in this species.8,9 These drugs have cardiovascular actions that are important to consider in the equine patient.
The use of acepromazine alone or in combination with α2-agonists was correlated with a lower anaesthetic risk compared to other commonly used drugs.3,4 Acepromazine has antiarrhythmic properties and may offer some myocardial protection. In dogs10 it reduces the sensitivity of the myocardium to catecholamines. Acepromazine can cause a decrease in arterial blood pressure as a result of CNS depression, α-adrenergic blockade and decrease in total peripheral resistance. A decrease in after-load may decrease the workload of the myocardium thereby improving blood flow and oxygen delivery to peripheral tissues, which would be beneficial during the maintenance phase of anaesthesia. Steffey demonstrated a significant fall in arterial blood pressure but an increase in cardiac output in halothane anaesthetized horses given acepromazine.11 Acepromazine has marked anaesthetic sparing effects; 0.05 mg/kg reduced the minimum alveolar concentration of halothane in ponies by approximately 37%12 and this is likely to contribute to its beneficial cardiovascular effects. Recently acepromazine was shown to improve the haemodynamic variables associated with romifidine, butorphanol and tiletamine-zolazepam anaesthesia in horses.13 In addition acepromazine decreased the shunt fraction and ventilation-perfusion mismatch with resultant improvement in PaO2 during recumbency.13 There is unequivocal evidence that acepromazine exerts a positive benefit on horses that are anaesthetized.
Acepromazine is unlikely to produce satisfactory tranquillization in an excited animal and may cause a profound fall in blood pressure in these animals because α-blockade is superimposed on pre-existing β-mediated vasodilatation from endogenous catecholamines;14 the same could happen in horses that have very recently been exercised. Acepromazine is likely to cause an exaggerated cardiovascular response in the face of hypovolaemia so should be reserved for healthy, hydrated elective surgery candidates.
The α-adrenergic agonist agents produce reliable sedation,15 predictable, dose-related cardiovascular effects16 and a decrease in the requirements for inhalant agents.17 Bradycardia and first- or second-degree AV blocks are common. Initially, total peripheral resistance and arterial blood pressure rise, but this is followed by a period of hypotension secondary to a significant decrease in cardiac output. The cardiovascular effects of the α2-adrenergic agents are most obvious when given intravenously. In a fit racehorse with a low resting heart rate and pre-existing AV block, high doses of intravenous α2-adrenergic drugs can cause syncope. Under these circumstances, intramuscular administration would be preferable. Slow intravenous administration of lower doses of xylazine (<0.03 mg/kg) combined with the opioid analgesic butorphanol (0.02 mg/kg) will often provide excellent sedation with fewer cardiovascular problems. If syncope does occur, atropine or glycopyrrolate will usually, but not always, increase the heart rate. Fortunately the acute bradycardia and AV block are short lived (<5 minutes).
Collapse following injection of premedicant agents can result from inadvertent intra-carotid injection; this is easily differentiated from syncope by the violent nature in which the horse collapses to the ground. If it is possible to safely approach the animal, intravenous access should be confirmed, and diazepam, acepromazine or xylazine administered in an attempt to sedate the animal. Additional therapy includes fluids and respiratory support. The final outcome depends on how much CNS damage has occurred. Intra-carotid injections can be fatal, particularly with phenothiazine agents18 (personal observation).
INDUCTION OF ANAESTHESIA
Anaesthesia is most safely and easily induced with injectable agents and indeed induction of anaesthesia with inhalant agents, a technique which has been used in foals, is associated with an increased anaesthetic risk.4 None of the commonly used induction drugs or protocols (diazepam/ketamine, guaiphenesin/ketamine, guaiphenesin/thiopentone, thiopentone) have an effect on outcome4 and therefore this choice can be based on the anaesthetist’s personal preference, experience and availability of drugs.
MAINTENANCE OF ANAESTHESIA
The choice of maintenance agent and technique does have important implications – the use of volatile agents carries a three times higher risk of death than total intravenous (TIVA) maintenance (0.99% versus 0.31%, respectively).4 Although procedures conducted under TIVA tended to be shorter this did not fully explain the discrepancy in outcome. Intravenous agents cause less cardiovascular depression and a decreased stress response (less adrenocortical activity).19,20 The cardiovascular depression associated with volatile inhalant agents seems to be implicated in the high incidence of anaesthetic complications in horses. For these reasons TIVA techniques should be used when possible and these have recently been reviewed.21 The most popular technique is guaiphenesin-ketamine-xylazine (“triple drip”) which can be used for procedures up to 2 hours with minimal cardiorespiratory effects.22,23 Newer techniques that include propofol have been reported and provide remarkable cardiovascular stability for up to 4 hours9 but the high cost of propofol currently limits its use in clinical practice.
Another approach is to use anaesthetic sparing agents in combination with inhalant agents. Infusions of lignocaine produce a dose-dependent decrease in the minimum alveolar concentration (MAC) of halothane,24 but unlike other species including human beings, opioids are less consistent at reducing the requirements of inhalant agents in horses.25 If the procedures involve surgery of the pelvic limb epidural anaesthesia should be considered; morphine and ketamine both reduced the MAC of halothane in the pelvic but not thoracic limbs of ponies.26
If inhalant agents are used the question must be is one better than the other? In an attempt to answer this question a large randomized study was undertaken to compare isoflurane and halothane in equine anaesthesia.5 Overall (>8000 horses) there was no difference in outcome between the two agents; however, the mortality rate was significantly reduced in horses aged 2 to 5 years and the incidence of cardiac arrest was reduced by 60%, especially in high-risk cases if isoflurane was used. This is likely related to a lesser degree of cardiovascular depression reported with isoflurane compared to halothane in horses.27–29 More recently sevoflurane has been used in equine anaesthesia and although it has not undergone a large head to head clinical trial with other inhalants, its cardiovascular depressant effects are similar to other inhalant agents and are dose related.30,31
Regardless of the technique employed, the problems faced by the anaesthetist are similar. Throughout anaesthesia, cardiac rhythm and arterial blood pressure must be closely monitored, even during short procedures. Careful attention to the ECG may show trends that forewarn of serious complications. Severe myopathy resulting in the inability to stand and euthanasia is a complication of the post-anaesthetic period in some equine patients (third cause of death in the CEPEF study3,4). It has been shown unequivocally that the initiating factors of this disease originate during anaesthesia, with arterial hypotension (mean arterial blood pressure (MAP), less than 70 mmHg), even for short periods of time, being the most significant contributing factor.32–35
CARDIOVASCULAR MONITORING IN THE ANAESTHETIZED PATIENT
Obviously, before one can avert or treat a cardiovascular problem its presence must be detected. Ideally cardiac output (CO) should be measured as this reflects the volume of blood pumped by the heart per minute and available for perfusion of vital organs and tissues. The normal CO of 70 mL/kg/minute in conscious horses can fall by 30–50% in patients anaesthetized with volatile agents especially if mechanically ventilated.36 Cardiac output measurement is not commonly performed in a clinical setting although newer technologies in both adult horses and foals now make it more feasible.37–39 A description of the technologies involved is beyond the scope of this chapter but the interested reader is directed to a review by Corley and others.37
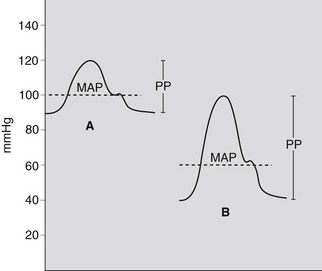
Much can be learnt about the cardiovascular status of the horse by touch and careful observation. The peripheral pulse should be palpated frequently and is easily felt at the facial artery, digital arteries of the front and hind limbs, or dorsal metatarsal artery. The pulse rate in an anaesthetized adult horse is usually 25–50 bpm. It must be emphasized that it is pulse pressure (PP), the difference between systolic (SBP) and diastolic pressure (DBP), that is being felt when palpating a pulse and that even if it feels strong it does not necessarily equate to an adequate MAP. For example, a horse with a SBP/DBP of 100/40 has a pulse pressure of 60 and a MAP of 60 mmHg using the formula MAP = (SBP + (2 × DBP)/3). An animal with a SBP/DBP of 120/90 has a pulse pressure of only 30 which may feel soft, yet its MAP (100 mmHg) is much better (Fig. 20.1). The relationship between blood pressure and cardiac output must also be considered when interpreting blood pressure values:
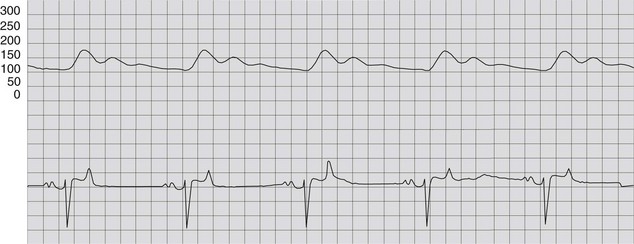
Electrocardiography is useful for determining rate, rhythm and conduction times but one must be cognizant that an ECG only reflects electrical events and not mechanical function of the heart. The ECG can be obtained using a standard lead system, but during anaesthesia a simple monitor lead such as the base-apex lead may be more practical and less likely to interfere with the surgical site (see Chapter 13). A recorder is useful so that a reference ECG can be obtained at the start of the case for future comparison.
Arterial blood pressure can be measured indirectly (noninvasively) or directly (invasively). Noninvasive methods are attractive, because they are usually less expensive and simple. The Doppler method has been extensively used in horses; this involves placing a piezoelectric probe over an artery, the coccygeal being the most popular. The probe detects blood flow, which is amplified and emitted at an audible frequency from the Doppler unit. A blood pressure cuff and sphygmomanometer are applied proximally; the cuff is inflated until no blood flow is heard then slowly deflated. The first sound occurs when SBP equals cuff pressure. Unfortunately, this technique cannot accurately define MAP, which is the primary determinant of perfusion pressure. In addition, studies show that this method leads to large measurement errors in dorsally recumbent horses.40 Commercially available oscillometric instruments may have similar limitations and are often unable to measure at the normal slow heart rate of adult horses. The accuracy of an indirect oscillometric monitor has been reported in both awake and anesthetized foals.41 There was good agreement between this technique (cuff placed around the tail) and direct measurement (greater metatarsal artery) for mean and diastolic blood pressure but less so for systolic blood pressure. Giguere and others also concluded that indirect oscillometric techniques were acceptable for measuring MAP in foals but in that study blood pressure did not correlate with cardiac output.42 Another disadvantage of these techniques is the frequency of recording; it may take several minutes for the machine to complete its cycle, resulting in a delay in important information reaching the anaesthetist.
In all but the shortest of procedures, direct blood pressure monitoring is recommended. This requires catheterization of a peripheral artery and a site is chosen that gives the anaesthetist free access without interfering with the surgical field. The arterial catheter can be connected to a pressure transducer placed at the level of the atrium (point of the shoulder in dorsal recumbency, at the level of the xiphoid if in a lateral position) and displayed on an oscilloscope, usually along with the simultaneously recorded ECG (Fig. 20.2). This system will provide beat-by-beat information on systolic, diastolic and mean blood pressure. Interpretation of the arterial wave form may indicate if there is peripheral vasoconstriction; a long slow decline in the waveform suggests resistance to run off (vasoconstriction, waveform A in Fig. 20.1) and a steep and rapid decline would suggest that peripheral resistance is low (waveform B in Fig. 20.1); vasoconstriction and increased afterload may be associated with a lower cardiac output. Pulse contour analysis is an emerging noninvasive technology for assessing cardiac output and has been studied in horses.43
Arterial blood gas monitoring is also recommended in anaesthetized horses because hypoxaemia due to shunting and ventilation-perfusion mismatch is common and will impact on oxygen delivery to vital organs and tissues.44,45
INTRAOPERATIVE CARDIOVASCULAR COMPLICATIONS
Hypotension
Hypotension associated with a decreased cardiac output is probably the commonest problem facing the equine anaesthetist. Undetected and untreated hypotension may lead to cardiovascular collapse and serious postoperative consequences including myopathies. Mean arterial blood pressure in awake horses is usually between 105 and 135 mmHg. Below a MAP of 60 mmHg autoregulation of blood flow to vascular beds is lost. Blood pressure must be monitored under anaesthesia and it is desirable to maintain a MAP greater than 70 mmHg to avoid muscle hypoperfusion and postanaesthetic mypopathy in adult horses.35 If only indirect systolic pressure (SAP) can be measured, one must be cognizant of its limitations,40 but a SAP greater than 90 mmHg, especially in a laterally recumbent animal, should reflect an adequate MAP. There are many possible causes of hypotension (Table 20.1), and often more than one problem is present. These include continued influence of premedicant and induction agents, potent inhalant agents, positive pressure ventilation, hypovolaemia, too deep a plane of anaesthesia and bradycardia. Positive pressure ventilation retards cardiac return and can lead to a drop in cardiac output and blood pressure. If ventilation seems to be the cause, check that the peak inspiratory pressure is ≤20 cmH2O, and that the expiratory pause is as long as possible. Administration of antibiotics, especially sodium penicillin, may cause a significant drop in arterial blood pressure.46
Table 20.1 Possible causes and specific treatments of hypotension in anaesthetized horses
| CAUSE | TREATMENT(S)* |
|---|---|
| Premedicant agents | |
| Acepromazine | |
| α2-adrenergic agents | |
| Inhalant agents | < div class='tao-gold-member'> Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|