Chapter 45 Bradyarrhythmias and Conduction Abnormalities
• Conduction abnormalities that lead to bradyarrhythmias are due to conduction delays or conduction blocks within the specialized conduction system.
• Dogs and cats with persistent bradyarrhythmias causing clinical signs such as syncope generally require implantation of an artificial pacemaker.
SPECIFIC BRADYARRHYTHMIAS
ATRIAL STANDSTILL
Definition, Causes, and Electrocardiographic Findings
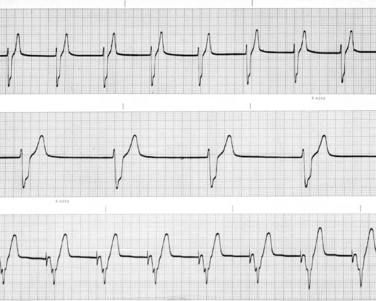
Atrial standstill is the rhythm diagnosis when no P waves are visible on the ECG and atrial fibrillation is not evident (Figure 45-1). Atrial standstill occurs when the atrial myocardium is unable to depolarize. This occurs for two broad general reasons: (1) either the atrial muscle is destroyed by disease or (2) the serum potassium concentration is increased to a level at which the resting membrane potential of atrial cells is so low (i.e., closer to zero) that they no longer depolarize.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree