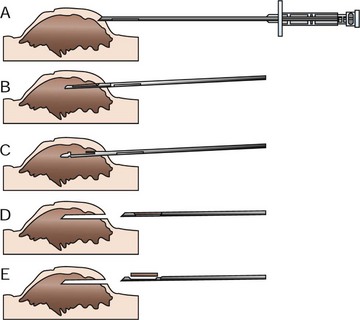
9 Fine-needle aspiration cytology (FNAC) is a simple and rapid way to obtain information about a tumor and is often the first step in the diagnostic work-up (see Chapter 7). Results of FNAC help guide the diagnostic tests for staging. Studies have shown that FNAC is a reliable and useful method to guide further work-up when neoplasia is suspected or, in many cases, to help rule out neoplasia altogether.1,2 Nonetheless, FNAC gives only limited information and may be nondiagnostic or equivocal. Inflammation, necrosis, and hemorrhage may result in cytopathologic changes that do not accurately represent the underlying disease process. Histologic confirmation is therefore required for definitive diagnosis of neoplasia. Specific indications for pretreatment biopsy are as follows: 1. When fine-needle aspirate cytology is nondiagnostic or equivocal. 2. When the type of recommended treatment (radiation versus chemotherapy versus surgery) would be altered by knowledge of the tumor type or grade. 3. When the extent of recommended treatment (ablative surgery versus wide excision versus marginal excision) would be altered by knowledge of the tumor type or grade. 4. When the tumor is in a difficult area to reconstruct (maxillectomy, locations requiring extensive flaps, head and neck) and planning is needed to prepare the patient and client appropriately. 5. When knowledge of the tumor type or grade would change the owner’s willingness to go forward with curative-intent treatment. If any one of the listed criteria is met, a pretreatment biopsy should be pursued. Needle core biopsy utilizes various types of needle core instruments (e.g., Tru-Cut [Baxter General Healthcare, Deerfield, IL] or ABC needle [Kendall Sherwood-Davis & Geck, St. Louis, MO]) to obtain soft tissue (Figure 9-1). Most of these needles are manually operated, although spring and pneumatically powered needles are available as well. Specialized core instruments are used for bone biopsies and will be covered in Chapter 24. These instruments are generally 14-g in diameter and procure a piece of tissue that is about 1 mm wide and 1.0 to 1.5 cm long. In spite of this small sample size, the structural relationship of the tissue and tumor cells can usually be visualized by the pathologist. Virtually any accessible mass can be sampled by this method. It may be used for externally located lesions or for deeply seated lesions (e.g., in the kidney, liver, or prostate) with image-guidance via closed methods or at the time of open surgery.
Biopsy Principles
Biopsy Methods
Needle Core Biopsy
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Veterian Key
Fastest Veterinary Medicine Insight Engine