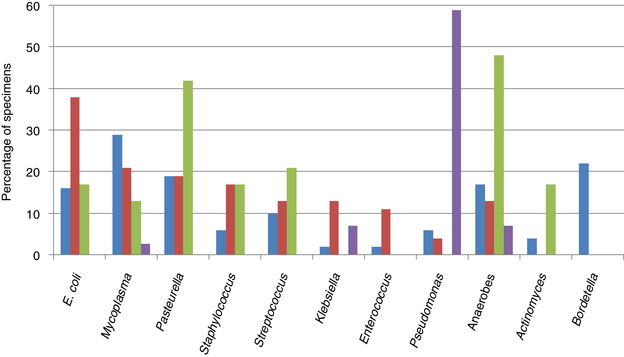
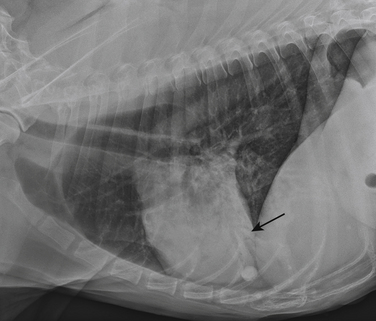
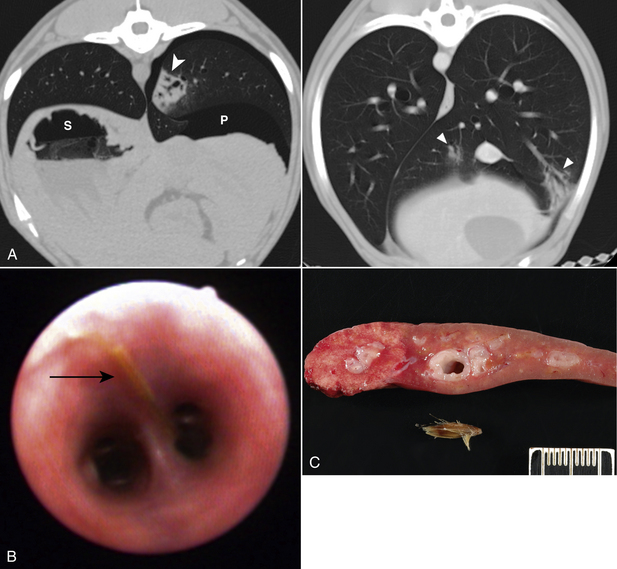
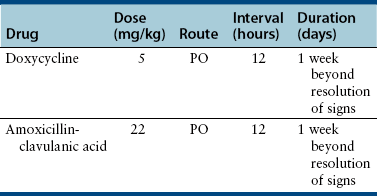
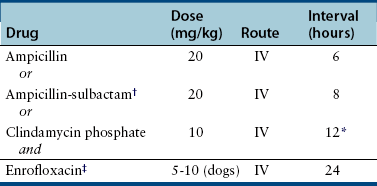
Chapter 87 Etiology, Epidemiology, and Pathogenesis Bacterial tracheobronchitis or bronchopneumonia may be acute or chronic and varies considerably in severity from subclinical through to fulminant and immediately life threatening. Infection of the airways and pulmonary parenchyma can occur secondary to (1) aspiration of gastrointestinal or oropharyngeal bacteria; (2) opportunistic invasion of commensal bacteria as a result of impaired bronchopulmonary immune defenses; (3) hematogenous spread of bacteria to the bronchopulmonary tree from extrapulmonary sites; or (4) aerosol or oronasal transmission of primary respiratory pathogens. Bronchitis and bronchopneumonia that result from invasion by commensal bacteria are the focus of this section. Organisms maintained in the environment (and/or in reservoir hosts) such as Nocardia, Mycobacterium, Leptospira, Rickettsia rickettsii, and Yersinia can also cause pneumonia in dogs or cats. The reader is referred to Chapters 30, 43, 44, 50 and 55 in Section 2 for more information on these infections. Information on Bordetella, Mycoplasma, and Streptococcus infections (as part of Canine Infectious Respiratory Disease Complex) is provided in Chapters 34, 38 and 40 in Section 2. Bordetella, Mycoplasma and some Streptococcus strains have the potential to be contagious pathogens that most often cause disease in young (or young adult) dogs and cats and those housed in overcrowded environments. Many aerobic and anaerobic commensal bacterial species have been isolated from dogs and cats with opportunistic tracheobronchitis and bronchopneumonia (Figure 87-1 and Box 87-1).1–13 The relative prevalence of each bacterial species may be affected by the underlying condition(s) that predisposes to bacterial invasion, the population of animals studied (see Figure 87-1), and the methods used to collect and culture specimens from the respiratory tract. FIGURE 87-1 Prevalence of bacterial species isolated from respiratory lavage specimens from dogs with lower respiratory infection (BAL, blue), aspiration (transtracheal lavage or BAL, red), foreign body pneumonia (BAL, green), and dogs with bronchoscopically diagnosed tracheal collapse (BAL, purple). (Compiled from references 7, 9, 10, and 13.) Secondary bacterial infection after aspiration of gastrointestinal or oropharyngeal contents is a common underlying reason for bacterial bronchopneumonia in adult dogs, but is rare in cats. Chemical damage to the lungs results from inhalation of acidic gastric fluid and particulate matter (“aspiration pneumonitis”). In some cases this is followed by development of bacterial bronchopneumonia. Conditions that predispose dogs to aspiration pneumonitis include brachycephalic obstructive syndrome; laryngeal paralysis, laryngeal surgery, or laryngeal foreign bodies; esophageal disorders such as megaesophagus, decreased esophageal motility, or esophageal foreign bodies; hiatal hernia; decreased mentation, seizures, or recumbency secondary to neurologic disease, sedation, or anesthesia; tracheostomy tube placement; vomiting; and swallowing disorders such as cricopharyngeal achalasia.11,13–15 More than 30% of dogs in one study had more than one abnormality that predisposed to aspiration; the combination of esophageal and neurologic disease was most common.11 In cats, most bacterial pneumonia follows viral infections or hematogenous spread of bacteria to the respiratory tract; aspiration pneumonia is rarely reported.4,6,12 Aspiration pneumonia has been described rarely in association with dysautonomia16 and arytenoid lateralization for treatment of laryngeal paralysis.17 Systemic immune compromise can predispose to life-threatening bacterial infection after aspiration in both dogs and cats. In a study of 47 dogs with aspiration that had airway lavage specimens cultured (primarily by transtracheal wash), 77% of specimens yielded bacterial organisms.13 The most prevalent species was Escherichia coli. Other frequently isolated organisms from dogs with aspiration pneumonia were Mycoplasma spp., Pasteurella spp., Staphylococcus spp., Klebsiella spp., and Enterococcus spp.13 Overall, gram-negative aerobes are more likely to be present than gram-positive aerobes in dogs with aspiration pneumonia. Anaerobes are also frequently isolated, and many dogs have mixed bacterial infections. Infections with Pseudomonas aeruginosa, Acinetobacter baumannii, and Corynebacterium species such as Corynebacterium ulcerans have also been described.13,18 Some of these infections may be acquired from the hospital environment. Conditions that impair local airway defenses predispose to opportunistic invasion of the tracheobronchial tree and pulmonary parenchyma by commensal bacteria. These conditions include ciliary dyskinesia, viral infections (especially persistent viral infections such as canine distemper virus or feline calicivirus infection), tracheobronchial collapse, tracheal stent placement, eosinophilic bronchopneumopathy, airway foreign bodies or neoplasia, chronic bronchitis, and bronchiectasis.5,7,9,12,18–21 Chronic bronchitis and bronchiectasis either may be sterile inflammatory processes that predispose to opportunistic bacterial invasion, or alternatively they occur secondary to chronic bacterial infections of the airways (e.g., as a result of chronic low-grade aspiration secondary to laryngeal paralysis). However, in many dogs with disorders such as tracheobronchial collapse, eosinophilic bronchopneumopathy, or chronic bronchitis, concurrent bacterial infection is not present. In one study of dogs with tracheal collapse that underwent bronchoscopy and bronchoalveolar lavage (BAL), Pseudomonas was the most prevalent opportunistic bacterial species isolated (see Figure 87-1).9 In contrast, Pseudomonas is an uncommon isolate from dogs with opportunistic lower respiratory infection.10 In dogs with airway foreign bodies (usually grass awns), anaerobes, Pasteurella, gram-positive cocci, and Actinomyces predominate.7 Signs and Physical Examination Findings Dogs with bacterial bronchitis may have no clinical signs, or cough may be present. Other systemic signs such as fever, lethargy, or inappetence are usually absent. Involvement of the pulmonary parenchyma may be associated with more severe signs such as fever (as high as 107°F [41.6°C]), anorexia, lethargy, dehydration, weakness, weight loss, a moist and/or productive cough, serous to mucopurulent nasal discharge, tachypnea, tachycardia, respiratory distress, increased or harsh lung sounds on thoracic auscultation, crackles, wheezes, reduced lung sounds (due to lung consolidation), and/or cyanosis.13,22 Some animals with pneumonia show no signs or only a few of these signs. Uncommonly, hemoptysis is reported.23 Clinical signs of the underlying illness (such as vomiting, regurgitation, neurologic signs, or septic shock) may also be identified.13 Cats with bacterial bronchopneumonia may show only fever, lethargy, and/or inappetence. Respiratory signs, and especially cough, are often absent.12 Bacterial bronchitis or bronchopneumonia is usually suspected based on a history of underlying predisposing conditions, clinical signs, and radiographic findings. Antemortem diagnosis of infection is most often based on cytologic examination in conjunction with culture and susceptibility of airway lavage specimens. Procedures for collection of airway lavage specimens include transtracheal wash, endotracheal wash, or BAL. Fine-needle aspiration of consolidated lung tissue may also be useful to rule out other disorders such as neoplasia or fungal pneumonia but carries some risk of iatrogenic pneumothorax.4,24,25 The risk of pneumothorax may be reduced if ultrasound guidance is used. Assessment of laryngeal function (with doxapram stimulation) should be considered in any dog anesthetized for bronchoscopy and airway lavage. In some instances, the diagnosis of bacterial bronchopneumonia is made by histopathology and culture of a lung biopsy specimen collected during surgery or tissue specimens collected at necropsy. Complete Blood Count, Serum Biochemistry Profile, and Urinalysis Most dogs and cats with bacterial bronchopneumonia have leukocytosis due to a neutrophilia, often with bandemia and toxic neutrophil changes.4,5,12,13,22 Leukopenia may also occur, but some animals have a normal leukogram. Anemia of inflammatory disease may also be present. The serum biochemistry profile and urinalysis can be unremarkable or may have changes that reflect the presence of concurrent systemic disease. Arterial blood gas analysis provides the most accurate assessment of oxygenation status in animals with bronchopneumonia. Hypoxemia (PaO2 ≤80 mm Hg at sea level) can be detected in around 75% of dogs with aspiration pneumonia,13,22 with a mean PaO2 of 69 to 77 mm Hg.5,13,22 Hypocapnia may also be present. The alveolar-arterial (A-a) oxygen gradient may be increased (up to 83 mm Hg with a median around 41 mm Hg; for room air, values >15 mm Hg indicate lung dysfunction).13,22 Dogs with aspiration bronchopneumonia may have bronchointerstitial to alveolar changes in one or more lung lobes. Most often an alveolar pattern is present (Figure 87-2).13,22 The most commonly affected lung lobe is the right middle lung lobe, and so a left lateral projection as well as right lateral and ventrodorsal projections in full inspiration are important to identify changes in this lobe. The left and right cranial lung lobes are also frequently affected.13,22 Radiographic changes can lag behind the aspiration event for up to 24 hours. Clues to underlying causes of bronchopneumonia, such as megaesophagus or situs inversus (ciliary dyskinesia), may also be evident. FIGURE 87-2 Left lateral thoracic radiograph from a 12-year-old male neutered German shepherd dog with a history of regurgitation, cough, and pyrexia. Air bronchograms (arrow) can be seen overlying the cardiac silhouette, which were less apparent on the right lateral view. The presence of an alveolar pattern in the ventral portions of the left and right cranial lung lobes in this dog was consistent with a diagnosis of aspiration pneumonia. Air is also visible in the esophagus. Dogs and cats with plant awn pneumonia may have a focal interstitial to alveolar pattern that tends to involve the caudal and accessory lung lobes, and to a lesser extent the right middle and left and right cranial lung lobes.26 Less often, pneumothorax, consolidation of affected lung lobes, and/or pleural effusion (see Pyothorax) are identified. Because of increased sensitivity over plain radiography, computed tomography (CT) may be useful to evaluate the airways and pulmonary parenchyma when thoracic radiographs are unremarkable or underlying plant awn pneumonia is suspected. Airway thickening and bronchiectasis may be evident in dogs with bronchitis. Focal interstitial to alveolar pulmonary opacities and pleural thickening are the most common finding in animals with migrating plant foreign bodies; other findings include pneumothorax and/or pneumomediastinum, mild enlargement and contrast enhancement of thoracic lymph nodes, lung lobe opacification, mediastinal or thoracic wall masses, and/or pleural effusion (Figure 87-3).26 CT may be useful to guide subsequent bronchoscopy and BAL fluid collection for animals with focal bronchopneumonia. FIGURE 87-3 Migrating plant awn foreign bodies. A, CT scan images from a 1-year-old female spayed German shorthaired pointer dog. Pneumothorax (left, P) and multifocal pulmonary opacities (white arrowheads) are present (S = stomach). B, Bronchoscopic image showing a plant awn in a bronchus of a 2-year-old male neutered Belgian Malinois. C, Portion of the right middle lung lobe of a 2-year-old female spayed Labrador retriever, which was removed during thoracotomy. A 1-cm plant awn was removed from a pocket of mucoid material within a bronchus. (C, Image courtesy University of California, Davis, Veterinary Anatomic Pathology Service.) On bronchoscopic examination, dogs and cats with bacterial bronchitis or bronchopneumonia may have edematous and hyperemic airways, accumulation of mucus or mucopurulent secretions, and/or mucosal irregularity.5,6 Other findings include airway collapse, airway stenosis, and bronchiectasis. Foreign bodies such as plant awns may be identified and removed (see Figure 87-3, B);7 if not, identification and localization of a focal accumulation of pus in an airway may direct subsequent surgical removal of a lobe affected by a migrating plant awn. Ideally, airway lavage specimens should be collected and submitted for aerobic, anaerobic, and Mycoplasma cultures before treatment with antimicrobial drugs is commenced, although this may not be feasible if severe respiratory compromise is present. The need for anaerobic cultures is controversial because anaerobes are difficult to isolate and tend to have predictable susceptibilities. Anaerobes are most likely to be present in dogs with aspiration pneumonia or grass awn foreign bodies. Mycoplasma species may also be difficult to isolate (see Chapter 40). False-negative culture results can also occur if low numbers of bacteria are present, if the specimen is small, fastidious organisms are present, or if antimicrobial drugs have recently been administered. Because a variety of gram-positive and gram-negative bacteria as well as Mycoplasma spp. can be found in low numbers in the lower respiratory tracts of healthy dogs and cats,3,27–29 a positive culture on a respiratory lavage specimen alone is not diagnostic for bacterial bronchitis or bronchopneumonia. However, a positive culture in conjunction with cytologic evidence of leukocytosis with intracellular bacteria supports the presence of infection. When quantitative bacterial cultures on BAL fluid can be performed, it has been suggested that growth greater than 1.7 × 103 CFU/mL is likely to be clinically significant.5 BAL is more likely to identify clinically significant bacteria, but collection of specimens by transtracheal wash is sufficient if diffuse disease is present and bronchoscopy is not available or not affordable.30 Care should be taken not to overinterpret the significance of few organisms, or minimally pathogenic organisms (e.g., Bacillus spp. or coagulase-negative staphylococci) that may represent airway contaminants. Some animals with bacterial pneumonia may have positive blood cultures. If airway lavage is not possible because of severe respiratory compromise, blood cultures should be considered in order to obtain information about the identity and susceptibility of bacteria involved. Further study is required to determine the sensitivity and specificity of blood culture for diagnosis of bacterial pneumonia in dogs or cats. Selection of antimicrobial drugs for treatment of secondary bacterial tracheobronchitis and bronchopneumonia in dogs and cats should ideally be based on the results of culture and susceptibility testing. For dogs with secondary bacterial tracheobronchitis, treatment should be withheld until the results are available, or empiric treatment with doxycycline (first choice) or amoxicillin–clavulanic acid (second choice) is suggested (Table 87-1). Amoxicillin–clavulanic acid is not active against Mycoplasma, so if Mycoplasma infection is suspected, doxycycline is a more appropriate choice. The optimal duration of treatment is unknown, but if a clinical response to treatment occurs in the first 7 to 10 days, treatment could be continued for a week beyond resolution of clinical signs.30 TABLE 87-1 Antimicrobial Drugs That May Be Useful to Treat Secondary Bacterial Tracheobronchitis in Dogs Animals with severe bronchopneumonia may require hospitalization and parenteral treatment with broad-spectrum antimicrobial drugs such as a combination of a fluoroquinolone and a β-lactam (ampicillin, ampicillin-sulbactam) or clindamycin (Table 87-2). Clindamycin may be a good choice if lung consolidation is present and/or anaerobes are suspected, because of its good tissue penetration, although some anaerobes and Pasteurella are resistant to clindamycin. If fluoroquinolone resistance is likely based on the regional prevalence of bacterial resistance, drugs other than a fluoroquinolone with activity against gram-negative bacteria may be indicated based on culture and susceptibility test results or the regional prevalence of bacterial resistance. Examples include aminoglycosides, third-generation cephalosporines, carbapenems such as meropenem, or ticarcillin–clavulanic acid. The spectrum of antimicrobial activity should be narrowed once the results of culture and susceptibility are available. TABLE 87-2 Suggested Empiric Antimicrobial Drug Choices for IV Use in Dogs or Cats with Bacterial Bronchopneumonia Pending the Results of Culture and Susceptibility∗ ∗Spectrum should be reduced once the results of culture and susceptibility are available. †Dose based on ampicillin component. ‡Other fluoroquinolones such as pradofloxacin (which also has activity against anaerobes) should be considered for treatment of cats because of the risk for retinal toxicity in this species, although parenteral formulations are not available. Other drugs with activity against gram-negative bacteria (e.g., meropenem, third-generation cephalosporines, aminoglycosides) could also be considered for parenteral treatment of cats or if the regional prevalence of fluoroquinolone resistance is high. See also Chapter 86.
Bacterial Bronchopneumonia and Pyothorax
Bacterial Tracheobronchitis and Bronchopneumonia
Aspiration Pneumonia
Tracheobronchitis and Bronchopneumonia Secondary to Impaired Local Airway Defenses
Clinical Features
Diagnosis
Laboratory Abnormalities
Arterial Blood Gas Analysis
Diagnostic Imaging
Advanced Imaging
Bronchoscopy
Microbiologic Tests
Culture
Treatment and Prognosis
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Bacterial Bronchopneumonia and Pyothorax
Only gold members can continue reading. Log In or Register to continue
