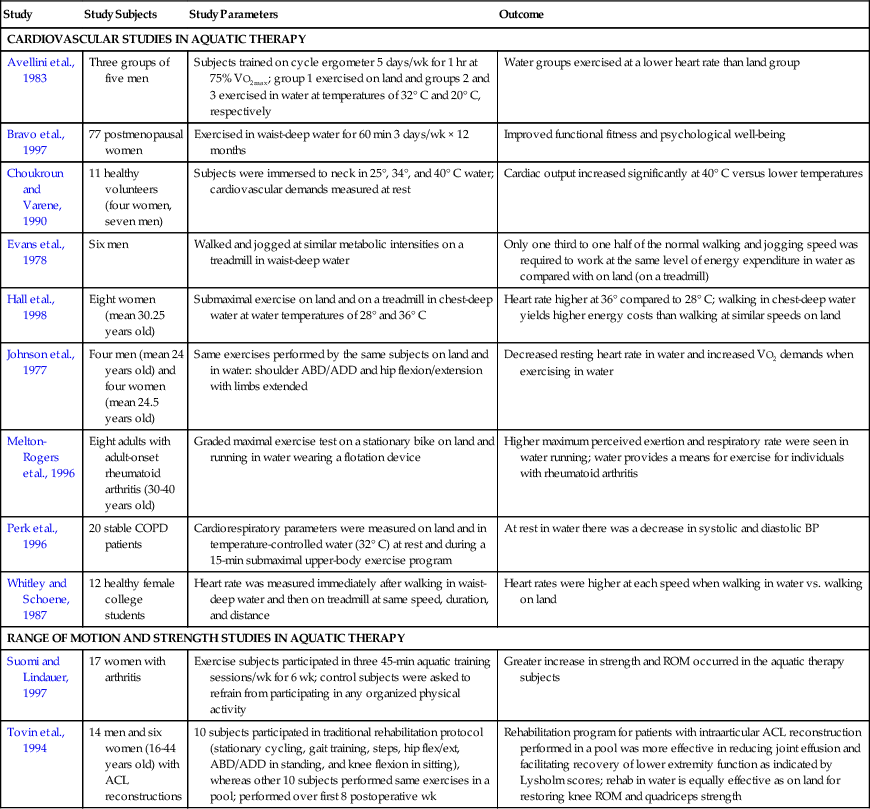
David Levine, Darryl L. Millis, Jeffrey Flocker and Lauren MacGuire The relative density of an object is the ratio of the weight of the object to the weight of an equal volume of water.1 Relative density depends on the composition of an object. Densities of various substances are defined by a pure number value called specific gravity. The specific gravity of pure water is 1.0.2 The specific gravities of fat, lean muscle, and bone are 0.8, 1, and 1.5 to 2, respectively.3 The relative density and specific gravity of an object determine how well an object will float. If the ratio of an object’s specific gravity to that of water is greater than 1, the object will tend to sink, and if the ratio is less than 1, the object will tend to float.4 The specific gravity of an object also determines how much of the object’s volume will float under water.4 For example, the specific gravity of ice is approximately 0.92; therefore 92% of ice will be submerged to displace enough water so that the upward force of buoyancy will equal the downward force of gravity, and 8% will float above the surface of water.2,5 A lean person’s specific gravity may be as high as 1.10, whereas an obese person’s specific gravity may be as low as 0.93.4 An object whose specific gravity is equal to that of pure water (1) will float just below the surface of the water. If a person’s specific gravity is greater than 1, that person will tend to sink. The greater the specific gravity, the faster the sinking velocity.2 Thus a lean animal that is not moving will have a tendency to sink faster than an obese animal. A body immersed in water is subjected to two forces, gravity and buoyancy. Buoyancy is defined as the upward thrust of water acting on a body that creates an apparent decrease in the weight of a body while immersed.2 Buoyancy stems from Archimedes’ principle: When a body is fully or partially submerged in a fluid at rest, it experiences an upward thrust equal to the weight of the fluid displaced.1,2,4,6 The amount of water displaced depends on the density of the body immersed relative to the density of water.2 An immersed limb or body with a relative density less than that of water will be assisted to the surface by buoyant forces.7 An object with a relative density less than 1 floats because the weight of the object is less than the weight of the water displaced.5,8 Buoyancy acts directly through the center of buoyancy.3 The center of buoyancy is the centroid of the displaced volume of water and depends on the distribution of the displaced volume of fluid relative to the body.9 Problems arise when the center of gravity and the center of buoyancy are not in the same vertical line. This can occur with the use of improperly placed floating devices, which can disrupt the vertical line, causing an animal to tilt or flip over so as to reach a state of equilibrium.3 The location of the center of buoyancy varies depending on the percent of body fat and distribution of adipose tissue. The more caudal the distribution of adipose tissue (which tends to occur more often in human females than males), the closer the center of buoyancy is located to the center of mass. Buoyancy aids in the rehabilitation of weak muscles and painful joints. It allows the patient to exercise in an upright position and may decrease pain by minimizing the amount of weight bearing on joints. For example the percentage of weight borne by human females when immersed in water is approximately 5.9% to 8.7% at the seventh cervical vertebral level, 25% to 31% at the level of the xiphoid, and 40% to 51% at the level of the anterior superior iliac spine.10 Males bear 6.8% to 10%, 30% to 37%, and 50% to 56% of their body weight in the upright position at these same levels.10 Other studies of humans have also found similar percentages of weight bearing at these same levels.11,12 In a study performed on dogs the amount of body weight borne when immersed in water (as a percentage of body weight on dry ground) was approximately 91% when the water was at the level of the lateral malleolus of the tibia, 85% at the level of the lateral condyle of the femur, and 38% at the level of the greater trochanter of the femur (Figure 31-1).13 This information may be particularly useful when treating patients with arthritis because joints may be unloaded as a result of the buoyant properties of water. Pascal’s law states that fluid pressure is exerted equally on all surfaces of an immersed body at rest at a given depth. This fluid pressure is directly proportional to both the depth and density of the fluid.4 Therefore the deeper a body is immersed in water, the greater the pressure exerted. The atmospheric pressure at the surface of water is 1.00 kPa (15.7 psi), and fluid pressure increases by 0.029 kPa (0.43 psi) per foot of depth.3 It can be estimated that the pressure exerted on a part of the body immersed 3 feet below the surface will experience a fluid pressure of 1.09 kPa (17 psi). Because hydrostatic pressure provides constant pressure to a body or limb immersed in water, it may provide an improved environment for working with swollen joints or edematous tissues.7 Hydrostatic pressure opposes the tendency of blood and edema to pool in the lower portions of the body and can therefore aid in reducing swelling.3 The benefits of edema reduction because of hydrostatic pressure are used by pregnant women who exercise in water to help minimize swelling in their lower extremities during exercise. The reduction in edema is probably caused by several factors, including a general increase in circulation with exercise, and the prevention of further pooling of fluids in the lower extremities by the pressure exerted on them by water. Hydrostatic pressure may also decrease pain during exercise. It is theorized that hydrostatic pressure provides phasic stimuli to the skin afferents (sensory receptors) that cause a decrease in nociceptor hypersensitivity. This acts to decrease a person’s or animal’s pain perception, which may allow the patient to perform a variety of movements with less pain.7,14 Viscosity is a measure of the frictional resistance caused by cohesive or attractive forces between the molecules of a liquid.15 The viscosity, or resistance to fluid flow, is significantly greater in water than in air,7 making it harder to move through water than to move through air. Water can therefore provide resistance that may strengthen canine muscles and improve cardiovascular fitness. Viscosity is important in aquatic therapy for several other reasons. Viscosity may increase sensory awareness and assist in stabilizing unstable joints.7 It can also help prevent falling by increasing the time span for patients to react,7 which may reduce patient anxiety. For example dogs with paraparesis, obesity, osteoarthritis, or severe deconditioning may be more willing to walk in water than on land because of water’s combined properties of buoyancy and viscosity, which help to support the dog. Any body movement occurring in water must overcome water viscosity.16 The resistance created by the viscosity of the liquid is proportional to the velocity of movement through a liquid. With increased velocity of movement in water, there is a uniform increase in resistance. Various movements in water may increase or help reduce resistance. Streamline flow is the steady, continuous movement of fluid. There is little friction between layers of fluid in streamline flow because the layers separate to move around the object and smoothly rejoin behind it.5 Turbulent flow consists of irregular movements of the layers of fluid.1,5 The irregular movement in turbulent flow causes increased friction between the molecules of the fluid and between the object and the fluid.5 Eddies are a form of turbulent flow in which the layers of fluid following a moving object in water move in circular directions.5 Eddies resist an object’s movement in water by pulling the object backward. Because of all these factors, resistance in aquatic exercise may be increased by increasing the velocity of movement of the patient, increasing the surface area of the object or body part moving in water, or by increasing the length of the lever arm of the object moving in water.16 The tendency for water molecules to adhere to each other is known as cohesion.2 Water molecules have a greater tendency to adhere together on the surface. Resistance to movement is slightly greater on the surface of water because there is more cohesion on the surface of water.2 Surface tension is the force of attraction between surface molecules of a fluid.3 Surface tension is not a factor if the moving body part is completely submerged in water. It becomes a significant factor when a limb breaks the surface of the water. Therapeutically if a patient is extremely weak, movements may be performed more easily in the water just beneath the surface rather than at or on the surface. There are many benefits of aquatic therapy. Exercising in water is effective for improving strength, muscular endurance, cardiorespiratory endurance, range of motion (ROM), agility, and psychological well-being, while minimizing pain.17–19 The purpose of this section is to provide the reader with information regarding human studies of the benefits of aquatic therapy. Table 31-1 provides a summary of these studies. It is likely that similar principles apply to animals. Table 31-1 Summary of Human Studies on the Benefits of Aquatic Therapy Gravity is the primary resistant force to exercise on land, whereas viscosity, friction, and turbulence are the primary resistant forces to exercise in water; these properties have a direct effect on heart rate and oxygen uptake.20 Arm exercises on land produced an increase in heart rate from a resting rate of 77 beats per minute to 92 beats per minute in men (age 21 to 27) and from 74 to 96 beats per minute in women (age 20 to 29). Exactly the same arm exercises in water produced an increase in heart rate from 60 to 99 beats per minute in men and from 60 to 98 beats per minute in women. Compared with the subjects exercising on land, the subjects exercising in water exercised at slightly higher heart rates and had a greater overall increase in heart rate because of the initial lower resting heart rate. Subjects in this study had lower resting heart rates in water than on land because of two factors: the reflex response of the cardiovascular system to the cold receptors of the skin, and the effect of hydrostatic water pressure exerted on the submerged body.20 The water temperature ranged from 26° to 26.5° C (78.8° to 79.7° F) during aquatic exercise. As discussed later, water temperature directly affects heart rate. Leg exercises further increased heart rate during water exercises: 76 (resting) to 124 (exercise) beats per minute for men on land versus 60 (resting) to 139 (exercise) beats per minute in water, and 73 (resting) to 126 (exercise) beats per minute for women on land versus 60 (resting) to 126 (exercise) beats per minute in water. The increased weight of legs as compared with arms may increase the necessary energy expenditure for exercises performed on land because of the increased mass and pull of gravity. This study demonstrated that heart rate and oxygen uptake were greater when performing exercises in water compared with performing the same exercises on land.20 The metabolic requirements are also greater for exercises performed in water than for exercises performed on land. In a study by Johnson et al.,20 men and women performed the same arm and leg exercises in water and on land. Oxygen uptake during exercise in water was 34% greater in men and 27% greater in women as compared with the same exercises on land.20 The differences between men and women are probably owing to different body compositions (male body composition tends to be more muscular, which requires more oxygen) and heights (men tend to be taller and have longer extremities, thereby having a longer lever arm, which requires more exertion to move). Another study found that subjects could walk or jog at slower speeds in water than on land while expending the same amount of energy as measured by oxygen consumption. In this study subjects walked at 2.6 to 3.5 km/hour (1.6 to 2.2 mph) in water, whereas subjects on land walked or jogged at speeds of 5.5 to 13.4 km/hour (3.4 to 8.3 mph). Both expended the same amount of energy, despite the greater velocity of people walking on land.21 A study by Whitley and Schoene19 supports these data with the observation that various types of exercises performed in water (aquatic calisthenics, shoulder and leg exercises, bicycle ergometry exercises, walking, and jogging) require a significantly greater amount of energy expenditure compared to the same exercises performed on land. Subjects in a study by Hall et al.22 also expended more energy walking in water than on land at speeds greater than 4 km/hour (2.5 mph). When aerobic exercise is used in the rehabilitation process, it may aid in improving cardiovascular fitness and weight reduction. Melton-Rogers et al.23 compared exercise during land bicycle ergometry with running in water with a flotation device in individuals with rheumatoid arthritis. Higher ratings of perceived exertion (RPE) by the subjects and respiratory exchange ratios were seen during water running.23 These studies demonstrate that walking in water at specific speeds may be sufficient to meet heart rate requirements for developing and maintaining cardiorespiratory fitness. Aquatic exercises are also beneficial for muscle strengthening. Bravo et al.17 performed a study on postmenopausal women who exercised in a pool with waist-deep water for 60 minutes, three times a week for 12 months. The average strength gain as a component of functional fitness was approximately 18%. Because of buoyancy water walking can provide an excellent alternative method of achieving and maintaining muscle strength and ROM in individuals with lower limb joint problems such as osteoarthritis (OA). Although exercise in water may not be as effective in achieving maximum muscle performance as land exercises, rehabilitation in water may minimize the amount of joint effusion and lead to greater functional improvement.24 Closed-chain exercises such as walking in water are more closely associated to movements in everyday activities than open-chain exercises because they recruit muscles in a more functional manner.25 Performing closed-chain exercises in an environment in which weight-bearing forces are decreased may minimize or eliminate damage and inflammation to the soft tissues, while maximizing functional training. The aqueous environment may also aid in reducing knee pain and joint effusion,24 which may facilitate the recovery of lower-extremity function after cranial cruciate ligament (CCL) stabilization in dogs. Water’s buoyancy can ease the performance of exercise activities while also providing proprioceptive feedback to aid in the rehabilitation process. The effect of buoyancy allows for gentler active exercises by decreasing the loads placed on the injured tissues compared with exercises performed on land.18 Aquatic exercises may be used as a transition to land-based exercises in postsurgery or postinjury rehabilitation. Water exercises are generally less painful than land exercises because of the support that buoyancy provides. Therefore water exercises may result in less discomfort maintain ROM and functional movement, and provide a better sense of security when initiating active movements.18 There are many physiologic effects resulting from exercise in heated water. Among them are increased circulation to muscles, increased joint flexibility, and decreased joint pain.26 Templeton et al. performed a study to determine whether subjects with rheumatic diseases experienced changes in joint flexibility and functional ability following an aquatic therapy program.26 Subjects exercised in water for 8 weeks. Exercises consisted of therapeutic games emphasizing both isotonic and isometric exercises of the trunk, neck, and upper and lower extremities. Water temperature was maintained at 32.9° C (91.3° F), and the air temperature was maintained at 31.7° C (89° F). Active ROM and a Functional Status Index test that recorded the degree of assistance, pain, and difficulty experienced in the performance of 18 tasks were measured before and after the 8-week aquatic therapy session. The results of the study indicated that pain decreased with therapy, and active ROM and functional ability increased. The decreased pain and improvement in performing daily activities had a significant impact on the overall increased functional ability of the subjects.26 These findings support aquatic therapy as an effective rehabilitation technique for increasing functional ability and joint flexibility in people with severe joint disease. Osteoarthritic and rheumatoid arthritic patients participated in another study of the effects of aquatic exercise on ROM and strength.27 Control subjects were asked to refrain from participating in any new physical activity throughout the duration of the study, whereas the exercise group participated in an aquatic exercise program. After 6 weeks, hip strength and ROM were measured. Hip strength in the aquatic exercise group increased 10.9%, whereas ROM increased 11.8% as compared with the control group.27 Water temperature may have a significant effect on the cardiovascular response to exercise. Subjects in cool water exercise at lower heart rates than those exercising on land at the same workload for several reasons.28 If the water temperature is low, peripheral vasoconstriction occurs, blood moves centrally, venous return is enhanced, and stroke volume increases. Therefore to maintain the same cardiac output, heart rate decreases. In one study, subjects training in cool water (20° C [68° F]) had enhanced stroke volume and decreased heart rate, thereby increasing exercise efficiency.28 It is also our experience that dogs exercise at lower heart rates walking on underwater versus land treadmills at the same velocity and length of time (unpublished data, Millis DL, 2000). Blood pressure is also affected by water temperature. In a study of subjects at rest while submerged in 32° C (89.6° F) water, systolic blood pressure decreased 14 ± 14 mm Hg and diastolic pressure decreased 6 ± 10 mm Hg because of peripheral arterial dilation. On the other hand, exercising in water at temperatures that exceed body temperature may increase cardiovascular demands above those of exercise alone.12 In one study, cardiac output was measured at rest while people were immersed in water temperatures of 25°, 34°, and 40° C (77°, 93.2°, and 104° F).30 Cardiac output of those immersed in 40° C water increased significantly. The authors of this study recommend that elite athletes train in water temperatures between 26° C and 28° C (78.8° F and 82.4° F) to prevent any heat-related complications.30 This temperature range is also recommended by the authors for pools in which healthy dogs are training. Lower temperatures are also apparently tolerated quite well by dogs, especially those with thicker hair coats. This section provides the reader with information concerning the types of aquatic therapy and equipment currently available for dogs. The anticipated use, size of the dogs receiving therapy, and funds available help determine the type of equipment best suited for rehabilitation. Some of the available forms of aquatic therapy include underwater treadmills, pools of various sizes, and whirlpools (Figure 31-2). Other forms of aquatic therapy include hot tubs or whirlpools used in hospitals (Figure 31-3). Cost-effective forms of aquatic therapy for smaller dogs include bathtubs, large basins, and plastic pools. Taking a dog to a lake or river is also a cost-effective means of providing aquatic therapy, but caution must be exercised when swimming dogs with recent incisions in these environments. Strong water currents and natural hazards must also be avoided.
Aquatic Therapy

Principles of Aquatic Therapy
Relative Density
Buoyancy
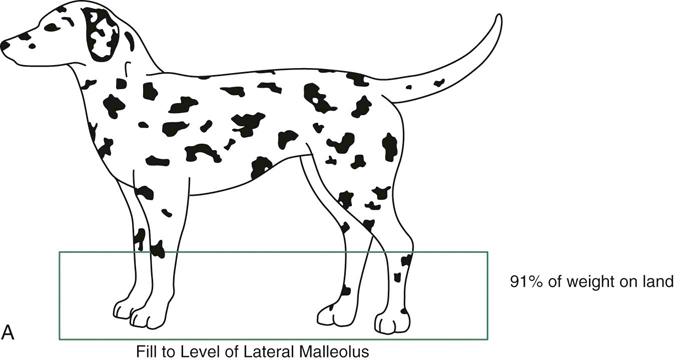
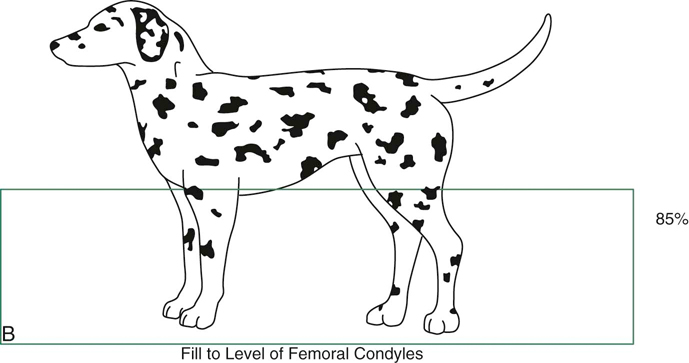
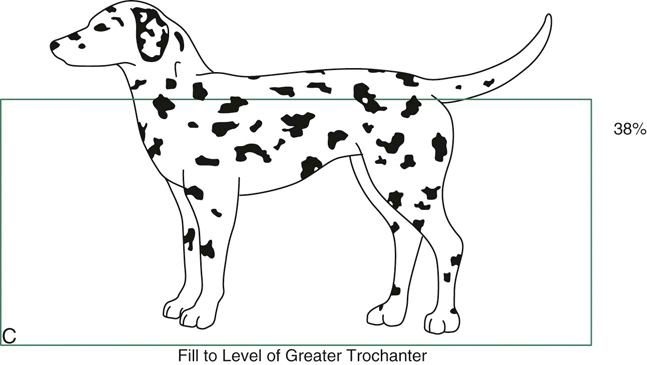
Figure 31-1 A, Dog in water to the level of the lateral malleolus. B, Dog in water to the level of the lateral epicondyle. C, Dog in water to the level of the greater trochanter. (Data from Levine D, Marcellin DJ, Millis DL et al: Effects of partial immersion in water on vertical ground reaction forces and weight distribution in dogs, Am J Vet Res 71:1413-1416, 2010.)
Hydrostatic Pressure
Viscosity and Resistances
Surface Tension
Aquatic Exercise Research
Study
Study Subjects
Study Parameters
Outcome
CARDIOVASCULAR STUDIES IN AQUATIC THERAPY
Avellini et al., 1983
Three groups of five men
Subjects trained on cycle ergometer 5 days/wk for 1 hr at 75% VO2max; group 1 exercised on land and groups 2 and 3 exercised in water at temperatures of 32° C and 20° C, respectively
Water groups exercised at a lower heart rate than land group
Bravo et al., 1997
77 postmenopausal women
Exercised in waist-deep water for 60 min 3 days/wk × 12 months
Improved functional fitness and psychological well-being
Choukroun and Varene, 1990
11 healthy volunteers (four women, seven men)
Subjects were immersed to neck in 25°, 34°, and 40° C water; cardiovascular demands measured at rest
Cardiac output increased significantly at 40° C versus lower temperatures
Evans et al., 1978
Six men
Walked and jogged at similar metabolic intensities on a treadmill in waist-deep water
Only one third to one half of the normal walking and jogging speed was required to work at the same level of energy expenditure in water as compared with on land (on a treadmill)
Hall et al., 1998
Eight women (mean 30.25 years old)
Submaximal exercise on land and on a treadmill in chest-deep water at water temperatures of 28° and 36° C
Heart rate higher at 36° compared to 28° C; walking in chest-deep water yields higher energy costs than walking at similar speeds on land
Johnson et al., 1977
Four men (mean 24 years old) and four women (mean 24.5 years old)
Same exercises performed by the same subjects on land and in water: shoulder ABD/ADD and hip flexion/extension with limbs extended
Decreased resting heart rate in water and increased VO2 demands when exercising in water
Melton-Rogers et al., 1996
Eight adults with adult-onset rheumatoid arthritis (30-40 years old)
Graded maximal exercise test on a stationary bike on land and running in water wearing a flotation device
Higher maximum perceived exertion and respiratory rate were seen in water running; water provides a means for exercise for individuals with rheumatoid arthritis
Perk et al., 1996
20 stable COPD patients
Cardiorespiratory parameters were measured on land and in temperature-controlled water (32° C) at rest and during a 15-min submaximal upper-body exercise program
At rest in water there was a decrease in systolic and diastolic BP
Whitley and Schoene, 1987
12 healthy female college students
Heart rate was measured immediately after walking in waist-deep water and then on treadmill at same speed, duration, and distance
Heart rates were higher at each speed when walking in water vs. walking on land
RANGE OF MOTION AND STRENGTH STUDIES IN AQUATIC THERAPY
Suomi and Lindauer, 1997
17 women with arthritis
Exercise subjects participated in three 45-min aquatic training sessions/wk for 6 wk; control subjects were asked to refrain from participating in any organized physical activity
Greater increase in strength and ROM occurred in the aquatic therapy subjects
Tovin et al., 1994
14 men and six women (16-44 years old) with ACL reconstructions
10 subjects participated in traditional rehabilitation protocol (stationary cycling, gait training, steps, hip flex/ext, ABD/ADD in standing, and knee flexion in sitting), whereas other 10 subjects performed same exercises in a pool; performed over first 8 postoperative wk
Rehabilitation program for patients with intraarticular ACL reconstruction performed in a pool was more effective in reducing joint effusion and facilitating recovery of lower extremity function as indicated by Lysholm scores; rehab in water is equally effective as on land for restoring knee ROM and quadriceps strength
Aquatic Therapy Equipment
< div class='tao-gold-member'>
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree




