Chapter 199 Antifungal Therapy
INTRODUCTION
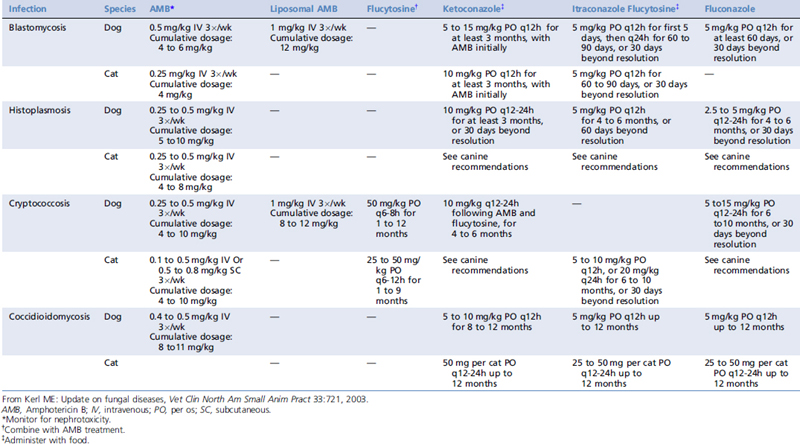
Limited classes of drugs are available to treat fungal infections. Antifungal drugs used to treat systemic fungal infections include polyene antibiotics and azole derivatives. Antifungal drugs are costly, require long-term administration, and have relatively high toxicity rates. In immunodeficient animals, definitive cure with any therapy is difficult or impossible. This chapter will review commonly available drugs and provide dosing information to treat various systemic fungal infections in dogs and cats (see Chapter 110, Fungal Infections).
CLASSES OF ANTIFUNGAL DRUGS
Polyene Antibiotics
Dosing protocols for AMB include intermittent administration until a cumulative dosage has been achieved, with interruption of therapy in the event of azotemia. Cats typically receive lower intermittent and cumulative dosages than dogs (Table 199-1). To reduce nephrotoxicity, AMB usually is infused in 5% dextrose and administered IV over 1 to 5 hours. Blood urea nitrogen and urine sediment evaluation should be measured before each dose. Identification of tubular casts in urine sediment is an earlier indicator of ongoing renal tubular damage than serum biochemical test results, and the treatment regimen should be altered if casts are identified. If blood urea nitrogen exceeds 50 mg/dl, the drug should be discontinued until azotemia resolves.2 Administration of 0.9% saline IV before giving AMB decreases the incidence of nephrotoxicity in people.4 Medications with known nephrotoxicity should not be given concurrently with AMB.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree