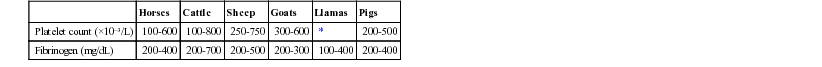
Jennifer L. Johns *, Consulting Editor The standard diagnostic test panel to evaluate coagulation in large animals includes platelet count, plasma fibrinogen, prothrombin time (PT), partial thromboplastin time (PTT), and serum fibrin and fibrinogen degradation products (FDPs). Proper collection and preparation of blood samples are paramount in obtaining accurate results (see Chapter 23). Platelet counts are routinely performed as part of the complete blood cell count (CBC). Citrated blood is required for coagulation testing and can also be used for platelet analysis. It is critical to have a 1 : 9 ratio of citrate to whole blood. The patient’s hematocrit can affect coagulation results when whole blood is used. When the hematocrit is over 55%, correction to a lower citrate volume is recommended to prevent overcitration and prolonged coagulation times.1 If the laboratory does not have reference intervals for a particular species, plasma from two or more healthy animals should be collected and assayed in a similar manner for comparison. Table 27-1 shows reference values for platelets and fibrinogen, but laboratory-specific values are preferable for these analytes and are necessary for other coagulation parameters. TABLE 27-1 Normal Values for Hemostatic Data in Ruminants and Horses * Insufficient data available. Modified from Duncan JR, Prasse KW, Mahaffey EA (eds). 1994. Veterinary laboratory medicine, ed 3. Iowa State University Press, Ames, IA; and Kaneko JJ, Harvey JW, Bruss ML (eds). 1997. Clinical biochemistry of domestic animals, ed 5. Academic Press, San Diego, CA. The platelet count is technically the platelet concentration in whole blood. Units = [platelets] × 103/µL; SI units = [platelets] × 109/L. Automated analyzers are routinely used to generate a platelet count. A rough estimate can be made via manual smear review: at 100× oil objective, the total number of platelets in 10 fields is counted. This count is then divided by 10 to yield an average number. This average is multiplied by a 15,000 to 20,000 conversion factor to yield [platelets]/µL.2 Both this estimate and the automated platelet count will be artifactually decreased if platelet clumps are present. Cattle normally average around 8 to 10 platelets per 100× oil objective field, and horses normally have 5 platelets or more per field.2 The mean platelet value (MPV) is the mean or average platelet volume and is measured in femtoliters (fL). This value is an average and does not represent the range of platelet volumes. Increased MPV is consistent with increased release of large/giant platelets and usually indicates a platelet regenerative response. The measurement of reticulated platelets (analogous to reticulocytes) may become widely accepted as another index of platelet regeneration. The platelet distribution width (PDW) is a calculated range of platelet volumes (representing anisocytosis), analogous to the red blood cell (RBC) distribution width. It is expressed as a percentage, and a higher percentage indicates a greater variation in platelet volume. The PDW in combination with the MPV value can indicate whether there are increased numbers of smaller and/or larger platelets. Also called the platelet-crit, the thrombocrit value is a function of the platelet count and the mean platelet volume. It is a better indicator of the total platelet functional potential than the platelet count, as a result of the greater functional capacity of larger platelets.3 A decrease in the circulating platelet count is termed thrombocytopenia. Thrombocytopenia is caused by one of three basic mechanisms: platelet sequestration, decreased platelet production, and decreased platelet lifespan caused by consumption or destruction (Boxes 27-1 and 27-2). Spurious thrombocytopenia occurs occasionally in horses when blood is collected into EDTA anticoagulant, causing in vitro platelet clumping.4 Platelet clumps are visible in the stained blood smear and may be indicated by error messages on an analyzer. Collection of a second sample into sodium citrate can yield an accurate platelet count and confirm a suspicion of spurious thrombocytopenia. Heparinized samples are not recommended for platelet counts because heparin-induced clumping can occur in any species. If citrated samples are used for platelet counts, the count must be corrected for citrate dilution (i.e., multiplied by 1.1). Splenic platelet sequestration can occur as a result of splenomegaly. Splenomegaly occurs due to various disorders including infiltrative diseases such as lymphoma, leukemia and multiple myeloma, and infectious and other inflammatory diseases such as immune-mediated hemolytic anemia that result in splenitis, lymphoid hyperplasia, and/or splenic extramedullary hematopoiesis. In addition, congestive splenomegaly occurs when the venous outflow is occluded by torsion, intestinal displacements, or congestive heart failure. Platelet sequestration is a relative thrombocytopenia resulting from redistribution (vs. an absolute thrombocytopenia), is reversible, and does not result in increased bleeding tendency. Decreased platelet production can occur with various bone marrow disorders, including myelophthisis (replacement of normal marrow). Myelophthisis is often due to marrow infiltration with neoplastic cells (e.g., plasma cells in multiple myeloma) and can result in pancytopenia. Familial myelofibrosis was reported in pygmy goats and resulted in marked pancytopenia, including thrombocytopenia with myelophthisis.5 Toxic damage to the marrow (e.g., from bracken fern toxicosis or nonsteroidal antiinflammatory drug administration) can result in myelosuppression and potentially aplastic anemia. Immune-mediated destruction of megakaryocytes, a variant of immune-mediated thrombocytopenia, causes decreased platelet production and release. Infectious agents can cause decreased platelet production via either indirect effects on megakaryocytes (e.g., equine infectious anemia virus) or by direct infection of megakaryocytes (e.g., acute bovine viral diarrhea infection).6,7 Evaluation of a bone marrow aspirate and core biopsy is indicated to evaluate megakaryocyte numbers and assess for dysplasia in a patient that is either persistently thrombocytopenic without evidence of peripheral consumption or destruction, or pancytopenic. Blood loss is a rare cause of thrombocytopenia; it is more likely that any concurrent bleeding is the result rather than the cause of severe thrombocytopenia. Studies in dogs found that acute severe blood loss induces a mild to moderate thrombocytopenia, with up to 50% reduction in platelet count.2 Rapid dilution of the blood volume with aggressive fluid therapy can decrease the platelet count as well as other hemostatic elements. The decrease is generally mild to moderate. Platelet lifespan can be reduced by destruction of platelets or by platelet consumption in widespread coagulation. Immune-mediated platelet destruction is a common cause of thrombocytopenia in horses. Immune-mediated thrombocytopenia (IMT) can be either idiopathic or a result of various etiologies including viral and bacterial infections, drug administration, and hemic neoplasia.7–10 Thrombocytopenia caused by idiopathic IMT is often marked, in contrast to thrombocytopenia from other causes. The thrombocytopenia of equine anaplasmosis resulting from infection with Anaplasma phagocytophilum is apparently multifactorial; an element of IMT is possible but not supported by experimental studies.11,12 Neonatal alloimmune thrombocytopenia has been reported in horses, mule foals, and pigs and is caused by colostral antibodies against foreign (paternal) epitopes on the neonate’s platelets.2 Excessive consumption of platelets occurs with disseminated intravascular coagulation (DIC). DIC is a clinical condition of disordered hemostasis that arises as a result of severe trauma; infectious or other inflammatory diseases, including septicemia; and disseminated neoplasia.13 Examples include DIC in horses with colic, calves with septic shock, and pigs with spontaneous heatstroke.14–17 The diagnosis of DIC in most species relies on finding evidence of both platelet and coagulation factor consumption (thrombocytopenia with one or more coagulation test abnormalities, described later) along with evidence of increased fibrinolysis (see the Increased Fibrin and Fibrinogen Degradation Products section). Snake envenomation directly causes platelet destruction in the absence of typical DIC as some snake venoms contain platelet-activating factors. Endothelial damage or necrosis (e.g., resulting from equine viral arteritis infection) can also result in platelet destruction with or without concurrent DIC.18 Thrombocytopenia is characterized by petechial or ecchymotic hemorrhages on the oral, nasal, and/or vaginal mucous membranes and the nictitans, sclerae, pinnae, and ventral abdomen. Epistaxis, melena, hyphema, and/or hematuria may occur, although spontaneous hemorrhage is rare unless the platelet count drops below 10,000 to 20,000/µL. Concurrent inflammation can increase a thrombocytopenic patient’s propensity for spontaneous hemorrhage.19 Prolonged bleeding from injections or wounds and a propensity to form hematomas with minor trauma are relatively common with a platelet count below 40,000/µL. Thrombocytosis is an increase in platelet count over the reference interval. A physiologic increase in platelet count can occur at high altitude.2 Relative thrombocytosis resulting from redistribution from splenic and other tissue stores can occur with exercise or epinephrine release. Splenectomy can result in thrombocytosis for several weeks because of both increased production as well as decreased platelet sequestration and destruction in the absence of the spleen.2 Absolute thrombocytosis can occur in a number of conditions as a secondary reactive change. Thrombocytosis resulting from any cause does not result in increased risk of thrombosis or any other clinical abnormalities; it is a reflection of the underlying disease(s). Many infectious and other inflammatory disorders including immune-mediated diseases can cause reactive thrombocytosis, as can surgery, neoplasia, and other inflammatory disorders. One infrequent cause of thrombocytosis in some species is iron deficiency, but this is not well documented in large animal species; chronic blood loss can be associated with thrombocytosis, and iron deficiency may be one factor. Administration of vincristine or vinblastine can result in thrombocytosis. Thrombocytosis can also occur as a rebound effect following prior thrombocytopenia. A rare cause of persistent severe thrombocytosis is primary thrombocythemia or other chronic myeloproliferative disease; bone marrow evaluation is indicated in this situation. Defects in platelet function have been described in large animals, but diagnosis can be challenging. The template bleeding test is routinely performed in small animals to assess primary hemostasis (e.g., platelet number/function and von Willebrand factor [vWF] function), but it is criticized for poor reproducibility in both humans and animals, including horses.20 Template bleeding tests have been useful for monitoring effects on aspirin therapy on hemostasis in horses, and may be suitable for serial monitoring of a patient if other factors such as platelet count remain constant. Aggregometry is considered a gold standard assay for platelet function but can be cumbersome; automated platelet function analysis with the PFA-100 device has become a standard platelet function assay in human medicine and is emerging as a valuable assay in veterinary medicine. More specific assessment of platelet function can require specialized assays. Glanzmann’s thrombasthenia is a disorder resulting in poor platelet aggregation and clot retraction in humans and animals, and it is caused by one or more defects in quantity or quality of platelet surface glycoprotein IIb/IIIa. A Peruvian Paso mare was diagnosed with hereditary Glanzmann’s thrombasthenia; the mare was 17 years old at the time of diagnosis.21 Other hereditary thrombopathias are infrequently described in animals. Chediak-Higashi syndrome is reported in Hereford, Japanese Black, and Brangus cattle. The bleeding diathesis associated with this syndrome is defined by substantial impairment of platelet aggregation in response to collagen.22 A hereditary thrombopathy in Simmental cattle is characterized by impaired platelet aggregation, with clinical signs including periodic epistaxis and severe hemorrhage following surgical procedures.23 Inheritance of this thrombopathy appears to be multigenetic, and aggregometry was not useful at differentiating carrier versus clear animals. A variant form of von Willebrand disease has also been described in a Simmental calf.24 Von Willebrand disease has been reported in Quarter Horses and consisted of a deficiency in high-molecular-weight multimers of vWF, consistent with type 2 von Willebrand disease in other species.25 Acquired defects in platelet function are common as a result of drug administration. Drugs that impair platelet function include aspirin, phenylbutazone, sulfonamides, estrogens, and phenothiazines.14 Several underlying medical conditions can also negatively affect platelet function, including uremia and liver disease. Production of high levels of immunoglobulins, particularly IgM, in monoclonal gammopathies hinders platelet function via protein coating of platelet surfaces.
Alterations in Hemostasis

Horses
Cattle
Sheep
Goats
Llamas
Pigs
Platelet count (×10−3/L)
100-600
100-800
250-750
300-600
*
200-500
Fibrinogen (mg/dL)
200-400
200-700
200-500
200-300
100-400
200-400
Platelet Parameters
Mean Platelet Volume
Platelet Distribution Width
Thrombocrit
Thrombocytopenia
Clinical Signs of Thrombocytopenia
Thrombocytosis
Platelet Function Defects and Von Willebrand Disease
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Alterations in Hemostasis
Chapter 27
