13 Advanced Veterinary Dental Procedures
Periodontal Surgery, Endodontics, Restorations, and Orthodontics
When you have completed this chapter, you will be able to:
• Describe indications for periodontal surgery and list instruments needed for these procedures.
• Discuss indications, contraindications, and general procedure for performing gingivoplasty.
• Discuss the indications and general procedure for performing open flap and root planing and mandibular frenoplasty.
• Define oronasal fistula and list three techniques for repair of this condition.
• Define endodontics and describe equipment and supplies needed to perform these procedures.
• List and describe commonly performed endodontic procedures.
• Describe the general procedure for performing conventional, nonsurgical root canal therapy.
• List and describe restorative materials used in veterinary dentistry.
• Describe the stages for performing orthodontic procedures.
Periodontal Surgical Techniques
Instruments and Materials
Periodontal surgery requires various instruments and materials (Box 13-1). The No. 3 handle is the standard type for scalpels. A variety of different blades may be used, including special periodontal knives. The No. 15c blade is extremely fine and therefore useful in periodontal surgical procedures. In addition, small tissue scissors, such as LaGrange scissors, are helpful in trimming periodontal tissue. Periosteal elevators are used to lift the gingiva away from the bone. Several types are available. The Molt elevator is one type; the Molt No. 9 is particularly popular. Many practitioners also like the ST-No. 7 instruments. Having a variety of periodontal surgical instruments available makes treating various anatomic and pathologic conditions less difficult.
Box 13-1
Instruments and Materials for Periodontal Surgery
No. 3 (or similar) scalpel handle
Small tissue scissors (LaGrange)
Periosteal elevator: Molt (No.2, No.4, or No.9), ST-No.7
Chlorhexidine 0.1% to 0.2% diacetate or gluconate (gluconate preferred)
Needle holders, spring locking (Castroviejo)
4-0 or 5-0 absorbable or nonabsorbable suture material with reverse FS-2 cutting needle
#2 or #4 round burs, appropriate for handpiece used
Treatment Techniques
Hyperplastic gingiva
Gingivoplasty technique
The pocket depth and contour is determined by inserting a probe to the depth of the pocket at several areas around the tooth. The corresponding depth is measured on the outside of the gingiva, also with the probe. A bleeding point is made by placing the tip of the probe perpendicular to the gingiva and applying slight pressure to make a small hole or by using a small-gauge needle. Bleeding points are made around the contour of the pocket and are used as a guide for the gingivectomy. The gingivectomy is made at an angle apical to the bleeding point to create a beveled margin. At least 2 mm of healthy, attached gingiva must be present apical to the base of the incision. A multifluted bur, laser, scalpel blade, or electrosurgery blade is used to excise the gingiva by cutting below the bleeding points, with the blade held at approximately a 45-degree angle and the tip of the blade toward the crown. The ends of the excision should be tapered into the surrounding gingiva to create the normal scalloped contour, particularly if several adjacent teeth are treated. Gingival tags can be removed with the blade or a sharp curette. The exposed tooth and root surface can now be scaled and planed smooth. Hemorrhage is controlled by applying pressure with wet gauze pads or hemostatic agents. If electrosurgery is being performed, caution must be exercised because the collateral damage may extend past the desired surgical line. In Figure 13-1, a periodontal probe is used to measure and mark the pocket depth. Once marked, a scalpel blade is used to perform the gingivoplasty.
Deep periodontal pocket
Endodontics and Restorations
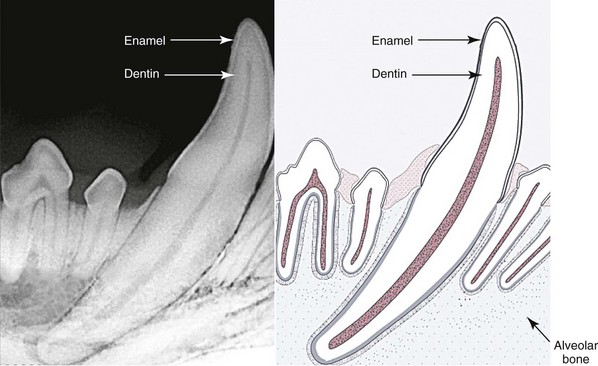
At one time, veterinarians did not treat fractured teeth. Consequently, many patients suffered silently as the tooth first died and then became abscessed. Endodontic therapy is a better option. Endodontic therapy is a general term for treatment of the dental pulp and may be used to save vital pulp, remove live or dead pulp, and prevent or treat infection (Figure 13-2).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree