1. Action: 100% total bodyweight. Rationale: 60% water + 40% other body structures. 2. Action: Intracellular fluid (ICF) = 2/3 of body fluid. Rationale: ICF is located within the cells. 3. Action: Extracellular fluid (ECF) = 1/3 of body fluid. 4. Action: Body fluids contain electrolytes, which yield ions. 5. Action: Ions are small water-soluble particles carrying one or more negative or positive charges. Sodium chloride (NaCl) is an electrolyte which dissociates into sodium ions and chloride ions when dissolved in water. 6. Action: Water balance and concentration need to be maintained equally within the body. 1. Action: Water intake – ingestion. Rationale: Ingestion of fluids and foods. 2. Action: Water intake – metabolism Rationale: Metabolism of fats and carbohydrates. 3. Action: Water loss – 50 ml/kg bodyweight/24 h. Rationale: This is the amount that needs to be replaced daily to ensure water balance. 4. Action: Sensible water loss – 25 ml/kg bodyweight/24 h. Rationale: Sensible loss via urine. 5. Action: Insensible water loss – 25 ml/kg bodyweight/24 h. Rationale: Insensible losses – respiratory, cutaneous and faeces. 6. Action: Water replacement = 50 ml/kg/24 h. Rationale: To balance water loss. 7. Action: Electrolyte replacement: Rationale: To balance electrolyte loss. 8. Action: Metabolic acidosis = loss of alkaline ions. Rationale: Replace loss with fluid containing alkaline ions to correct acid/base imbalance. 9. Action: Metabolic alkalosis = loss of acidic ions. Rationale: Replace loss with fluid containing acidic ions to correct acid/base imbalance. 1. Action: Normal physical appearance despite a history of fluid loss. Level (degree of dehydration as a percentage of bodyweight): Slight > 5%. 2. Action: Mild to dry mucous membranes, slight decrease in skin turgor. 3. Action: Decrease in skin turgor; dry mucous membranes; mild tachycardia; sunken eyes; slight increase in capillary refill time. 4. Action: Marked decrease in skin turgor; dry mucous membranes; sunken eyes; weak pulse; increased capillary refill time; oliguria; cold extremities. 5. Action: Very marked decrease in skin turgor; pale and dry mucous membranes; sunken eyes; tachycardia; cold extremities; muscle weakness; collapse; depression; anuria. Rationale: Equal osmotic pressure to plasma – no fluid movement thereby maintaining equilibrium. Rationale: Lower osmotic pressure than plasma – thereby encouraging movement of fluids into cells. 6. Action: Blood product – plasma. Rationale: This helps to expand plasma volume and treat hypoproteinaemia. 1. Action: 0.9% NaCl – normal saline (isotonic crystalloid). Rationale: Replace ECF. Gastric losses or loss of acidic ions from vomiting. 2. Action: 0.18% NaCl + 4% dextrose (isotonic crystalloid). Rationale: Maintenance requirements; primary water deficit replacement; neonatal ECF replacement. 3. Action: 5% dextrose (isotonic crystalloid). Rationale: Primary water deficit replacement. 4. Action: Hartmann’s solution (isotonic crystalloid). Rationale: Replace ECF. Diarrhoea and post gastric losses/alkaline ions. 5. Action: Ringer’s solution (isotonic crystalloid). Rationale: Replace ECF; gastric losses from vomiting. 6. Action: Haemaccel/Gelofusine (isotonic colloids). 7. Action: Plasma (blood product – isotonic). Rationale: Replace plasma proteins; expand plasma volume as above; clotting defects. 8. Action: Whole blood (isotonic). Hypotonic electrolyte solution or water. 1. Action: Select equipment – dosing syringe with catheter tip, towel, assistant, fluid. 2. Action: Measure correct volume of fluid in syringe. Rationale: Important to measure fluid replacement accurately to avoid excess or insufficient fluid. 3. Action: Request assistance to hold patient (see Chapter 1). Rationale: Ensure that the patient is kept at ease and feels safe. 4. Action: Support patient’s nose and mouth with left hand in normal position. 5. Action: Introduce the catheter tip syringe into the mouth between upper and lower premolars above the tongue surface. Rationale: This area is the most suitable to administer fluid safely and accurately. 6. Action: Slowly introduce 5–10 ml of fluid into the mouth and allow the patient to swallow. Stroke the ventral aspect of the pharynx to encourage swallowing. 7. Action: Continue until required volume has been delivered or the patient becomes agitated. 8. Action: Dry the patient’s mouth and surrounding area and replace in ready prepared clean kennel. Rationale: Always dry the area to help prevent heat loss and make the patient comfortable. 9. Action: Record total fluid volume given and the frequency on the hospital record. Rationale: Ensure record keeping is accurate to prevent over- or under-administration. 10. Action: Dispose of equipment safely and appropriately. Rationale: It is essential to dispose of equipment correctly to avoid contamination and accidents. 1. Action: Select and prepare equipment – prewarmed fluid, measured volume in sterile syringe with new sterile needle attached (maximum 10–20 ml/kg/site), clippers, surgical skin scrub, gloves, swabs (Fig. 4.2). 2. Action: Request assistant to restrain patient in lateral recumbency. 3. Action: Clip an area of approximately 3 × 3 cm on either side of the thorax over the ninth rib, midway between ventral and dorsal borders. 4. Action: Prepare skin aseptically with surgical scrub solution. Wear gloves. Rationale: Skin must be cleaned aseptically to reduce risk of infection. 5. Action: Infiltrate local anaesthetic into the prepared site as per veterinary surgeon instructions. Drape the area. 6. Action: Tent the skin and introduce the needle, attached to the fluid-filled syringe, subcutaneously. Rationale: Administration must be subcutaneous, avoiding any puncture of thoracic cavity. 7. Action: Withdraw the plunger of the syringe. Rationale: To check that a vein has not been punctured by accident. 8. Action: Administer the volume of fluid slowly and withdraw the needle (maximum 10–20 ml/kg/site). Rationale: Fast infusion of fluid can cause considerable discomfort. Rationale: To ensure even and effective distribution. 10. Action: Repeat the procedure on the other side of the thorax. Rationale: To ensure equal distribution in the body. 11. Action: Remove the drapes and dry the area. Allow the patient to resume sternal recumbency and place back in the kennel. Rationale: Ensure patient is comfortable in kennel. 12. Action: Dispose of equipment safely and appropriately. Rationale: It is essential to dispose of equipment correctly to avoid contamination and accidents. Any isotonic crystalloid fluid such as 0.9% NaCl; 0.18% NaCl + 4% dextrose; Hartmann’s solution. 1. Action: Select and prepare equipment – prewarmed fluid, measured volume in sterile syringe with sterile new needle attached, clippers, surgical skin scrub solution, swabs, gloves. 2. Action: Assistant to restrain patient in dorsal recumbency and reassure patient throughout procedure. 3. Action: Clip area surrounding umbilicus. Rationale: Reduce risk of infection by clipping hair, allowing a wide margin around umbilicus. 4. Action: Prepare skin aseptically and drape area. Rationale: To reduce risk of infection. 5. Action: Infiltrate local anaesthetic into prepared site – region of umbilicus – as per veterinary surgeon instructions. Rationale: To desensitize area prior to administration of fluid. 6. Action: Introduce sterile needle attached to fluid syringe through the skin and central line (linea alba) into the peritoneal cavity. Rationale: Ensure asepsis maintained and introduction efficient and smooth. 7. Action: Withdraw plunger of syringe. 8. Action: Introduce prewarmed fluid into the peritoneal cavity. Rationale: If any resistance is felt, stop and restart procedure from point 6. 9. Action: Withdraw needle and syringe, putting gentle pressure over injection site. 10. Action: Remove drapes and dry area. Allow patient to regain sternal recumbency, reassure and replace in kennel. 11. Action: Record fluid administration details. Rationale: To ensure accurate monitoring. 12. Action: Dispose of equipment safely and appropriately. Rationale: It is essential to dispose of equipment correctly to avoid contamination and accidents.
Administration of fluid therapy
INTRODUCTION
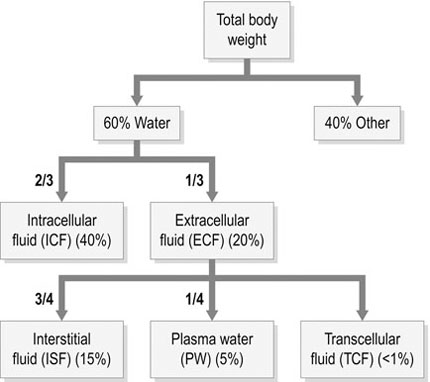
Procedure: Appreciation of water content in the body (Fig. 4.1)
Procedure: Appreciation of water balance in the body
Procedure: Assessing level of dehydration of the patient
Procedure: Selection of fluids in relation to their action in the body
Procedure: Selection of fluid for specific needs
Procedure: Oral fluid therapy
Fluid choice
Procedure: Subcutaneous fluid therapy
Fluid choice

Procedure: Intraperitoneal fluid therapy
Fluid choice
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


