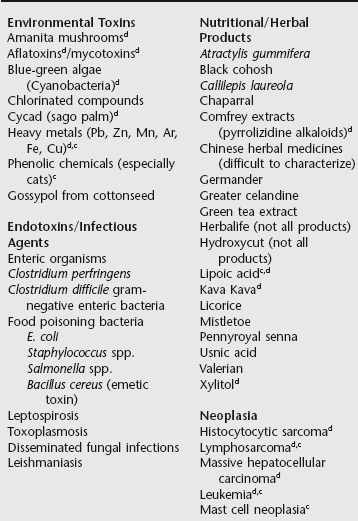
Chapter 141 Acute liver failure (ALF) is an uncommon, rapidly progressive, often lethal condition reflecting sudden, or perceptively sudden, severe hepatocellular necrosis or dysfunction associated with hyperbilirubinemia, coagulopathy, and evidence of hepatic encephalopathy (HE) (Nguyen and Vierling, 2011). As characterized in humans, HE manifests as a breadth of neurobehavioral or psychologic abnormalities ranging from overt to mild encephalopathy. No subjective or objective scoring system has been validated in companion animal patients, similar to criteria used in humans (Riordan and Williams, 1997). In humans with ALF, high-grade HE has a poor prognostic implication. Identifying the cause of ALF has prognostic and therapeutic implications but often remains enigmatic. However, a number of well-substantiated causes have been recognized (Boxes 141-1 and 141-2). Hepatotoxic and idiosyncratic drug reactions are most common, with environmental and plant toxins, infectious diseases, rare neoplastic disorders, and other conditions less common. The indiscriminant appetite of many dogs results in a greater risk of environmental toxin, hepatotoxic plant, or mycotoxin ingestion compared with cats. The liver has a high susceptibility to toxicity because of its location and central role in metabolic and detoxification pathways. Susceptibility and severity of hepatobiliary injury is influenced by age, species, patient nutritional status, concurrent drug administration, antecedent disease, the presence of excessive hepatocellular transition metal storage, antioxidant status, hereditary factors, and current or prior exposure to the same or similar compounds. Hepatic toxicity is the most commonly reported organ system toxicity associated with true adverse drug reactions that may be intrinsic or idiosyncratic (see Chapter 140). Metabolically generated toxins often derive from reactions catalyzed by the cytochrome P-450 system. Such toxins may be potentiated by microsomal enzyme inducers (e.g., phenobarbital, omeprazole), whereas toxicity of some is impaired by microsomal enzyme blockers (e.g., cimetidine, chloramphenicol, ranitidine). Although pathophysiologic mechanisms leading to ALF vary depending upon the causal agent, oxidative injury often plays a critical role. Many toxins are metabolized to a secondary injurious product generating toxic electrophilic adducts that interact with structural proteins, enzymes, or nucleoproteins (aflatoxin, cycad, sulfonamides) or that induce lymphocytotoxic responses or FAS-induced apoptosis (Box 141-3). The capacity of the hepatic microenvironment to terminate injury and regenerate perfused nonfibrosed hepatic parenchyma varies with the inciting cause, whether the toxin incapacitates protein transcription, the nutritional status of the patient (inappetence reduces glutathione [GSH] concentrations), presence of antecedent liver injury, and for dogs the status of transition metal accumulation (iron, copper). In humans, genetic polymorphisms in keratins 8 and 18 that confer antiapoptotic effects in liver injury increase susceptibility to ALF; these are known to segregate with ethnicity (Strnad et al, 2010). There is no information regarding this phenomenon in dogs or cats. Susceptibility to certain drugs and toxins having a narrow therapeutic or exposure window may reflect innate (individual or species related) or acquired low hepatic GSH. The increasing causal role of complementary alternative medications in ALF in humans is relatively uninvestigated in companion animals. All supplements or complementary alternative medications have risk for contamination with other undeclared botanicals or chemicals (Nguyen and Vierling, 2011).
Acute Liver Failure
Causal Factors
Pathophysiology
Acute Liver Failure