Abscesses
The definition of an abscess is ‘a localized collection of pus in a cavity formed by the disintegration of tissue’ (Blood and Studdert, 1999). Pus is the product of suppuration, which is the inflammatory process that occurs in the presence of pyogenic organisms that resist phagocytosis. Pus consists of dead phagocytes, predominantly neutrophils, inflammatory exudate, bacteria and cellular debris. Neutrophils contain lysosomal granules that contain degradative enzymes, which play a major role in the destruction of bacteria. The life span of the neutrophil is short (3–4 days). Dead or dying neutrophils release lysosomal enzymes that not only autolyse the neutrophil but also digest dead tissue cells around them. Rabbit neutrophils contain lower levels of myeloperoxidases compared to that in other mammals; thus the digestion of dead cells is less than in other species, meaning that pus remains thick and sticky, rather than becoming liquid (Baggiolini et al., 1969). As the suppurative process continues, a cavity forms that becomes walled off from the surrounding tissue. The wall is composed of young connective tissue containing collagen fibres and blood vessels. It is lined by the ‘pyogenic membrane’ composed of a layer of pus cells that have not yet autolysed. The two layers can often be visualized as separate entities. Neutrophils and other leucocytes continue to migrate into the abscess from blood vessels in the wall. Antibodies that can neutralize toxins and kill bacteria arrive at the site. Eventually the abscess becomes enclosed in a fibrous capsule composed of fibroblasts and inflammatory cells, with an inner layer of degenerating neutrophils (Chaffee et al., 1975). The abscess expands along the line of least resistance and can rupture through the skin or into a body cavity, discharging pus, bacteria and toxins. Surgical intervention to provide drainage can resolve the suppurative process or it may persist to become chronic.
Chronic abscesses are refractory to treatment. Resorption of water from pus results in thick, caseous material within the abscess cavity. The presence of any type of foreign material within the abscess harbours bacteria that have an inhibitory or toxic effect on neutrophils. Antibiotics cannot penetrate abscess cavities because of the poor vascularity. Binding with purulent material inactivates some antibiotics. Failure of an abscess cavity to heal after rupture or surgical drainage may occur because the fibrous wall of the capsule has become so rigid that it cannot collapse. Residual micro-organisms can then lead to renewal of inflammation.
Chronic suppuration is common in rabbits and slow-growing, well-encapsulated, relatively painless abscesses develop readily. Pasteurella multocida is frequently isolated. This bacterium has capsular polysaccharides that resist phagocytosis (Deeb, 1993). Pasteurella multocida can reside in the nasal flora of asymptomatic rabbits and spread to other sites during grooming. Other pyogenic bacteria such as staphylococci, Pseudomonas spp. and Fusiformis spp. can also be isolated from rabbit abscesses (Chaffee et al., 1975; Dominguez et al., 1975; Ward et al., 1981). Secondary infections in tissues damaged by other causes such as surgical incisions, bite injuries, trauma, penetrating wounds or foreign bodies often result in abscess formation. Once a primary abscess has become established, haematogenous spread to other sites or local spread along the lymphatics can result in the formation of secondary abscesses. Venereal transmission and injuries to the genital tract can result in abscesses developing in the reproductive system of breeding does.
Chronic abscesses in rabbits are notoriously difficult to cure. In other species, acute inflammation due to pyogenic bacteria is associated with leucocytosis, due to an increase rate of production of neutrophils from the bone marrow. This response is not marked in rabbits (Toth and Krueger, 1989). Lymphopenia is associated with any chronic disease in rabbits, including abscesses (Harcourt-Brown and Baker, 2001; Hinton et al., 1982). In other species, abscesses often burst and providing drainage alone can be sufficient to effect a cure (Knight et al., 1980). Abscesses in rabbits seldom come to a ‘head’ and rupture spontaneously, although large areas of skin can become necrotic and slough if the abscess is particularly large. In rabbits, lancing and flushing is seldom curative, even in combination with aggressive antibacterial therapy, and relapse is common.
The immune response of rabbits affected by abscesses has been investigated. Rabbits that have an existing chronic abscess show reduced neutrophil influx into a new acute abscess in comparison to rabbits without an existing abscess (Bamberger et al., 1989). In vitro studies have demonstrated that blood neutrophils from rabbits with long-standing abscesses show a decreased chemotaxis to Staphylococcus aureus in comparison with neutrophils from rabbits with acute abscesses. Bamberger and Herndon (1990) also found that neutrophils from rabbits with chronic abscesses (2 weeks old) have diminished bactericidal capacity and superoxide function. Superoxide is a free radical that is involved in the destruction of bacteria within the neutrophil. The rabbits with chronic abscesses did not produce serum opsonic factors. Opsonins are substances such as antibody or complement that render bacteria more susceptible to phagocytosis. The abscess fluid from the rabbits with chronic abscesses was inhibitory to neutrophil function.
In pet rabbits, abscesses are often related to underlying dental disease. Periapical abscesses are common and result in extensive osteomyelitis. Microabscesses form within the bone. Malnourishment is associated with dental problems and can delay wound healing and exacerbate abscessation. Commercial rabbits kept under intensive conditions for meat or fur commonly develop abscesses in association with poor ventilation and sanitation (Cheeke et al., 1982) where particularly pathogenic strains of S. aureus or P. multocida can exist.
6.1 Causes of abscesses in pet rabbits
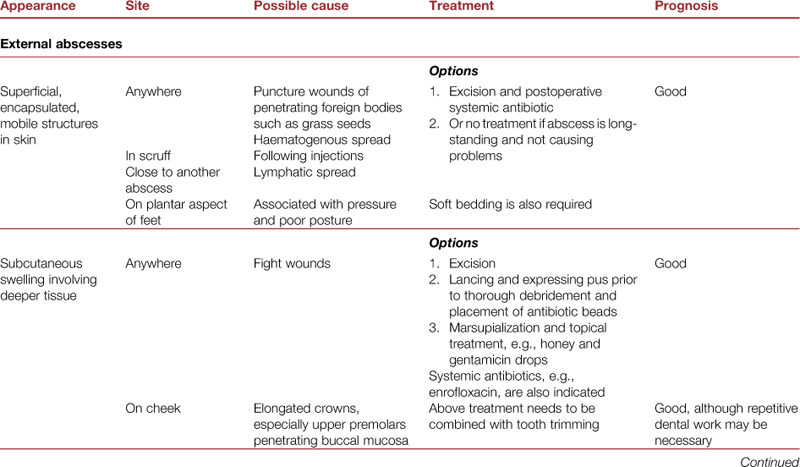
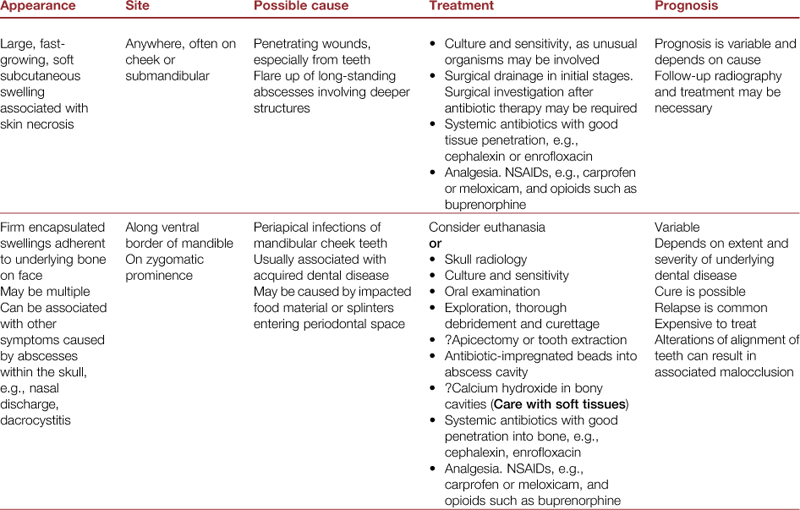
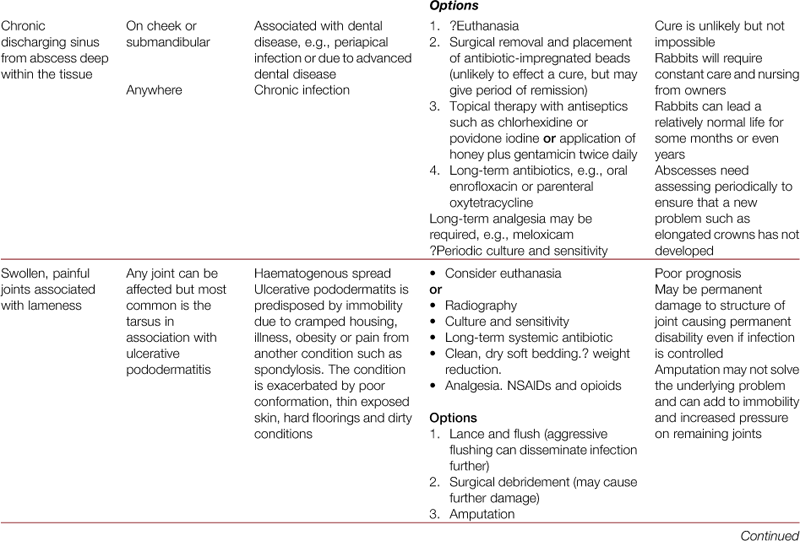
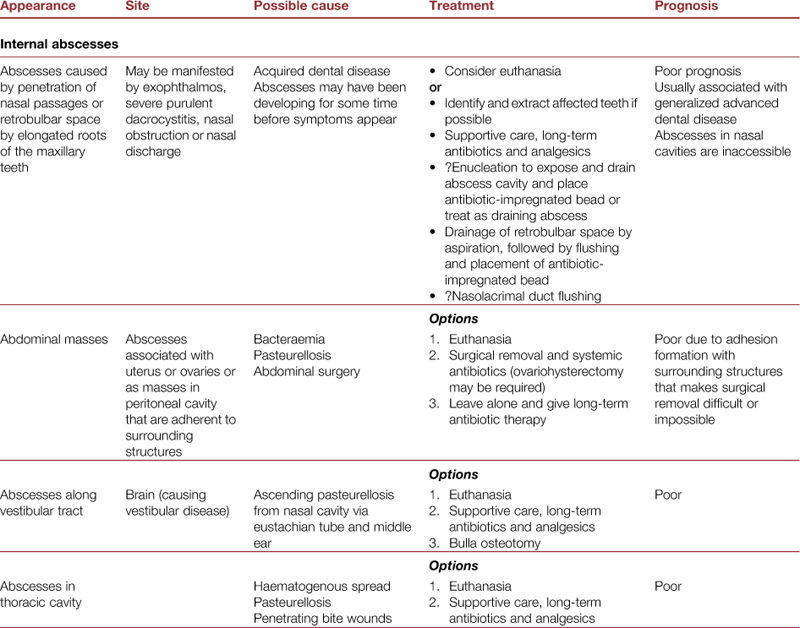
The causes of abscesses in pet rabbits are summarized in Table 6.1. It is important to ascertain the cause of abscess formation in order to institute appropriate therapy and remove the underlying cause. In dogs and cats, abscesses are usually due to penetrating injuries, especially bite wounds. Fights between rabbits can result in abscess formation or bite wounds can be inflicted on rabbits by dogs, cats, foxes or other predators. Penetrating wounds can also be caused by foreign bodies, such as seeds or pieces of hay that penetrate the skin or mucosal surfaces of the mouth. Haematogenous spread to distant sites can occur from any primary abscess and internal abscesses may develop in the thoracic cavity or abdomen. Abscesses can also occur after any surgical intervention in rabbits, particularly where suture materials are necessarily left internally or where surgical wounds are interfered with. Careful, sterile surgical technique can reduce this risk; however, those rabbits with compromised immunity may still develop abscesses.
In pet rabbits, most abscesses occur around the head and face and are associated with dental disease. They can be caused by overgrown crowns of maloccluded teeth that have penetrated the buccal mucosa or the skin on the lips. Alternatively, facial abscesses may be associated with infection at the apex of the teeth (see Figures 6.1–6.3). Acquired dental disease in pet rabbits is characterized by demineralization of the alveolar bone supporting the teeth. The periodontal space widens and the teeth become loose. Extraneous plant material can become impacted in the periodontal space. Periodontal disease can progress to allow periapical abscesses to develop. Once infection has reached the apex of the tooth, the structure of the root is destroyed and the surrounding alveolar bone becomes infected. Microabscesses can form throughout the surrounding bone (see Figure 6.1). Once osteomyelitis has become established, the prognosis is poor (Bohmer and Kostlin, 1988; Harcourt-Brown, 1995; Jenkins, 1997; Westerhof and Lumeij, 1987).

Figure 6.1 Lateral view of the skull of a rabbit with advanced osteomyelitis of the mandible.
In this lateral view of the skull of a 3-year-old, female Netherland dwarf, there is extensive osteomyelitis involving the roots of the mandibular cheek teeth and surrounding bone of one hemi-mandible. A large abscess is evident in which proliferative bone can be seen radiographically. This type of abscess carries a poor prognosis.

Figure 6.2 Lateral view of the skull of a rabbit with multiple abscesses associated with tooth roots that have penetrated the bone and continued to grow.
In this lateral view of the skull of a rabbit suffering from advanced dental disease, several tooth roots are growing into abscess cavities. The abscess under the chin contains a tooth root that is several centimetres long and is curling round in the cavity. The root of an upper second premolar is also elongated and curling round in an abscess involving the nasal cavity. Multiple abscesses in association with advanced dental disease carry a poor prognosis. (Image reproduced with kind permission from Waltham Focus.)

Figure 6.3 Lateral view of the skull of a rabbit with an abscess to show radiolucency.
The area of radiolucency in the mandible is associated with periapical infection of the second mandibular molar (fourth cheek tooth). This 1-year-old female mixed breed rabbit developed a palpable abscess over the lateral ramus 6 months prior to the radiograph. A large splinter of wood was wedged in the alveolar socket. The tooth was removed and the abscess successfully treated with antibiotic-impregnated beads. The rabbit subsequently developed an abscess in exactly the same place on the contralateral jaw. She spent her life in the garden where she would dig holes and chew through twigs and tree roots. The area of lytic bone shows clearly because there is no superimposition of the contralateral tooth.
6.2 Diagnosis of abscesses in rabbits
Abscesses in rabbits can be classified according to their clinical appearance and characteristics (Harvey, 1997). The prognosis varies with the type of abscess and each type requires a different approach (see Table 6.1). In most species, the development of an abscess is characterized by pain and accompanied by malaise and pyrexia. In rabbits, abscesses often do not appear to be painful and the animal may be eating well and not depressed. Pyrexia is not a feature of abscesses in rabbits.
Dental abscesses are very common in rabbits. Periapical abscesses are the commonest type and occur at typical sites in association with elongated tooth roots (Harcourt-Brown, 1995) (see Figure 5.1). Abscesses affecting the apex of the mandibular teeth can be palpated along the mandible and present as slow-growing subcutaneous swellings that may be mobile or may be adherent to deeper tissue. Neoplasia is a differential diagnosis. Osteogenic sarcoma has been recorded in the jaw in rabbits (Walberg, 1981) but is rare. Periapical abscesses of the maxillary teeth invade the nasal passages or periorbital space and cannot be palpated unless they have distorted the surrounding bone. Retrobulbar abscesses cause exophthalmos and can require enucleation of the eye to make a definitive diagnosis, although it is sometimes possible to aspirate the abscess by inserting a needle into the periorbital space. Ultrasonographic examination can determine the extent of the retrobulbar lesions, but may not be able to discriminate between abscess and fluid-filled cysts. CT or MRI may provide more definitive information. Tumours and cysts can also occur at this site. Abscesses within the nasal cavity require endoscopic confirmation, although a presumptive diagnosis can be made radiologically (see Fig. 5.12) or using CT. Affected rabbits may or may not show signs of respiratory tract obstruction such as a purulent nasal discharge, laboured breathing or upper respiratory noise. Nasal foreign bodies cause similar symptoms, which are usually unilateral (see Section 11.3). Chronic pasteurellosis also causes chronic purulent nasal discharge and upper respiratory tract disease (see Section 11.2.3). Abscesses around the apex of the maxillary incisors or premolars can obstruct the nasolacrimal duct and cause chronic dacrocystitis. Bony swellings of the zygomatic prominence can be palpated in association with abscesses at this site (see Fig. 5.11). Occasionally they will burst and discharge pus. The cheek is also the site of an abscess caused by penetration of the buccal mucosa by elongated crowns of the upper cheek teeth. Elongated crowns can be detected on careful examination of the oral cavity.
Superficial abscesses around the body can be palpated easily. Abscesses caused by bite wounds or penetrating injuries are usually associated with a history of a fight and may have a visible skin wound at the site of penetration. Abscessed joints are swollen and painful and the rabbit is lame. Internal abscesses can be difficult to diagnose. Large abscesses can develop within the abdomen without obvious clinical signs. They may involve the reproductive tract, occur after surgical intervention or be associated with adhesions. Symptoms only develop if adhesions interfere with digestive function. Lung abscesses impair respiratory function and cause dyspnoea, although symptoms may not be evident in the early stages of the disease when the rabbit is at rest.
Haematology is seldom diagnostic. Rabbits with abscesses do not seem to show a leucocytosis and neutrophilia, although a left shift is occasionally seen. Instead, non-specific signs of ill health such as mild anaemia and lymphopenia are encountered (see Figure 2.2). An increased monocyte count may be found in rabbits affected by abscesses, although monocyte counts within the laboratory reference do signify the absence of an abscess (see Section 2.2). Ultrasound scanning is a useful diagnostic aid to differentiate between internal abscesses and neoplasms. Radiology can also be useful. Some abscesses contain gritty, calcified material that shows up radiologically or ultrasonographically.
6.2.1 Radiology
Radiology can be used to determine the underlying cause of abscesses in rabbits and to ascertain the extent of bone destruction in cases of osteomyelitis. Radiography is indicated for any abscess involving underlying bone: i.e., facial abscesses or those affecting limbs or joints. Radiology of the skull is described in Section 5.8. Periapical abscesses may be a localized entity or part of a more serious disease process affecting the whole skull (see Figure 6.1). Abscessation is often the end point of acquired dental disease in rabbits (see Box 5.1). Lateral and dorsoventral skull radiographs are necessary for assessing the general state of the teeth and surrounding bone and for offering a prognosis. If the abscess is localized, it may be possible to identify the infected tooth from skull radiographs. Affected roots are often long and distorted (see Figure 6.2) or an area of radiolucency around the root may be seen (see Figures 6.3–6.5). Intra-oral views on dental film are useful for assessing changes that have taken place in association with infection of a specific tooth root. Flushing the cavity and instilling contrast medium can yield additional information about the extent of an abscess cavity.

Figure 6.4 Lateral view of a rabbit skull with moderate/advanced acquired dental disease (ADD) showing abscesses at the apices of the mandibular incisors, mandibular cheek teeth 1 and 2 and maxillary cheek teeth 1 and 2.
Areas of calcification are visible in the abscess ventral to the mandible.

Figure 6.5 Lateral view of a rabbit with moderate acquired dental disease.
A massive abscess originating from the apices of the mandibular incisors is visible as a soft tissue mass under the chin.
Radiography is necessary for the assessment of abscesses involving joints or long bones. If there is extensive bone destruction or multiple limbs are involved, the prognosis is poor, and euthanasia should be considered on welfare grounds. Although amputation can be an option if a single joint is involved, it increases the pressure on the remaining limbs and can result in ulcerative pododermatitis (see Section 7.10).
6.2.2 Bacteriology
Wherever possible, swabs should be taken for bacteriology and sensitivity. Although P. multocida is often believed to be the pathogen in rabbit abscesses, this is not always the case. Staphylococcus aureus is often found and other bacteria such as Bacteroides, Pseudomonas or Proteus can also be isolated (Hillyer, 1997). Swabbing the interior wall of the capsule of an abscess cavity, or preferably submitting a solid portion of this intraoperatively, is less likely to give a sterile culture than swabbing purulent contents.
6.3 Treatment of abscesses
The factors that improve success in treating rabbit abscesses are summarized in Box 6.1. While each case should be assessed on its own merits, successful treatment of rabbit abscesses will often depend on employing a range of treatments rather than a single method or agent. Many abscesses will require long-term treatment (months to years). Treatment is directed at removing as much exudate, necrotic debris and infected tissue as possible (while retaining structural integrity) and mopping up residual infection with antibiotics. Removal of the underlying cause and improving the health status of the rabbit are required to prevent recurrence (Figure 6.6). Treatment can prove expensive because of the need for repeated anaesthetics and the cost of diagnostic work-up, surgical exploration and long-term antibacterial therapy. Many different treatments for abscesses in rabbits have been described. Placing gentamicin-soaked collagen material into the abscess cavity was described by Bohmer and Kostlin (1988). Implantation of punctured clindamycin capsules into the cavity was described by Chappell (1994). Remeeus and Verbeek (1995) recommended packing abscess cavities with calcium hydroxide. Brown (personal communication) has had some success with injecting the abscess capsule in multiple sites with gentamicin. Some authors recommend long-term or permanent systemic antibiotic therapy (Hillyer, 1997), while others suggest the placement of drains in the abscess cavity (Malley, 1995). Setons were used by Hinton (1979). The use of creams and sprays containing digestive enzymes (trypsin) is described by Jenkins (1997). Blackwell (1999) describes the use of intramammary suspensions to pack abscess cavities after flushing the cavity with saline. As there are such a wide range of treatment options, it is obvious that there is no universal cure for abscesses in rabbits and each case must be judged on its own merit. The prognosis depends on the underlying cause (see Table 6.1).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree