CHAPTER 15. Endocrine Disorders
Patricia A. Schenck
DISORDERS OF THYROID METABOLISM
I. Normal thyroid function
A. Hypothalamus secretes thyroid-releasing hormone (TRH), which stimulates the release of thyroid-stimulating hormone (TSH) from the pituitary gland. TSH stimulates the release of thyroid hormones from the thyroid glands. Released thyroid hormones exert negative feedback on the hypothalamus and pituitary glands to decrease the production of TSH
B. Hormones produced by the thyroid
1. Total T 4 (thyroxine, tetra-iodothyronine) includes free and protein-bound
2. Total T 3 (tri-iodothyronine) includes free and protein-bound
3. Free T 4(FT4)
4. Free T 3 (FT 3) (the active thyroid hormone)
II. Tests for thyroid function
A. Total T 4
1. Measurement readily available
2. May be falsely normal in hypothyroid dogs that have T 4 autoantibodies (T 4AA)
3. 5% to 10% of hyperthyroid cats have normal T 4 concentrations
B. Total T 3. False results occur in 20% of hypothyroid dogs because of the presence of T 3 autoantibodies (T 3AA).
C. Free T 4
1. Different methods available for measurement
2. Free T 4 by equilibrium dialysis (FT 4d) is the “gold standard” measurement
a. Less affected by illness or medication than are T 4 or other methods of FT 4 measurement
b. Free from T 4AA interference
c. More consistently increased in hyperthyroid cats with other concurrent illnesses
d. Delayed or inappropriate shipping can cause increased values
D. Free T 3. Not much diagnostic utility as a single test. False results occur in 20% of hypothyroid dogs because of the presence of T 3AA
E. TSH
1. Poor accuracy on its own but good accuracy in combination with thyroid hormone measurement
2. Elevated in most cases of hypothyroidism but may also be elevated during recovery from illness or with administration of sulfa-containing antibiotics
F. Thyroglobulin autoantibodies (TgAA) (dogs only)
1. Marker for lymphocytic thyroiditis
2. Can be detected before the development of hypothyroidism
3. Detects active inflammation
4. Provides no information concerning thyroid function
G. T 3AA, T 4AA (dogs only)
1. Present in some (but not all) dogs that have lymphocytic thyroiditis
2. T 3AA interfere with measurement of T 3 and FT 3
3. T 4AA interfere with measurement of T 4 and FT 4 (some methods) but do not interfere with FT 4d
H. T 3 suppression test
1. Used in the diagnosis of hyperthyroid cats
2. A “pre” sample is taken for measurement of T 4, T 3, FT 4, and FT 3. T 3 supplement is given (25 ug) every 8 hours for six or seven treatments. A “post” sample is collected 2 to 4 hours after the last treatment
3. In a normal animal, the administration of T 3 supplement should result in increases in T 3 and FT 3 concentrations in the “post” sample compared with the “pre” sample. This elevation of T 3 and FT 3 should cause suppression of T 4 and FT 4 production
4. In hyperthyroid cats, T 3 and FT 3 concentrations increase in the post sample, but there is either no or poor suppression of T 4 and FT 4, indicating a loss of negative feedback
III. Hypothyroidism in dogs
A. Hypothyroidism is the most common endocrine disease in dogs, with an estimated prevalence of approximately 0.5%. Most common in middle-aged purebred dogs. Can occur in any breed, but golden retrievers and Doberman pinschers have the highest incidence
B. Pathogenesis
1. Primary hypothyroidism (thyroid defect). In primary hypothyroidism, thyroid hormone synthesis is impaired, and concentrations of thyroid hormones decrease in serum. TSH increases in an attempt to stimulate thyroid hormone production
a. Acquired (most common)
(1) Lymphocytic thyroiditis (about 50% of cases)
(2) Idiopathic thyroid follicular atrophy
b. Congenital (dyshormonogenesis)
a. Acquired (pituitary masses)
b. Congenital (dwarfism, receptor defects, dyshormonogenesis)
C. Lymphocytic thyroiditis
1. Thyroglobulin autoantibody is a marker for lymphocytic thyroiditis. Some dogs also have autoantibodies to T 3 or T 4
2. Present in about 4% of healthy dogs
3. Hereditary
4. Breed predilection: English setter, dalmatian, basenji, Rhodesian ridgeback, Old English sheepdog, boxer, others
5. Stages of lymphocytic thyroiditis
a. Subclinical thyroiditis
(1) TgAA present
(2) Thyroid hormone and TSH concentrations normal
(3) Focal inflammatory infiltrates of lymphocytes
(4) No clinical signs relating to hypothyroidism
(5) Treatment with T 4 not warranted
b. Subclinical hypothyroidism (partial thyroid failure)
(1) TgAA present
(2) Elevated TSH concentration
(3) Thyroid hormone concentrations normal or borderline low
(4) Extensive lymphocytic inflammatory infiltrates with follicular cell hypertrophy
c. Clinical hypothyroidism
(1) TgAA present
(2) Low thyroid hormone concentrations, elevated TSH concentration
(3) Extensive diffuse lymphocytic inflammatory infiltrates
(4) Functional thyroid follicles rare
D. Clinical signs
1. Weight gain or obesity
2. Lethargy, weakness
3. Cold intolerance, heat seeking
4. Skin disorders occur in 85% of patients with hypothyroidism. Skin disorders include poor coat quality, alopecia, hypopigmentation, secondary pyoderma and pruritus, otitis
5. “Tragic” facial expression
6. Myxedema
7. Cardiac abnormalities including bradycardia, decreased contractility, and increased risk for atherosclerosis resulting from lipid metabolism abnormalities
8. Neurologic signs including generalized weakness, forelimb lameness, laryngeal paralysis, megaesophagus, vestibular disease (circling, head tilt, incoordination)
9. Ocular abnormalities including eyelid edema, corneal lipid deposits, keratoconjunctivitis sicca
E. Diagnosis
1. Clinical pathology findings include chronic fasting hyperlipidemia, hypercholesterolemia, hypertriglyceridemia, nonregenerative anemia in about 35%, nonspecific findings
2. Diagnosis should not be based on clinical signs alone
3. Primary hypothyroidism is diagnosed based on finding low concentrations of thyroid hormones with an elevation of TSH
4. Hypothyroidism should not be diagnosed based on a single low T 4 concentration
F. Other causes of low thyroid hormone concentrations
1. Metabolic response to nonthyroidal illness
a. Often termed “sick euthyroid”
b. FT 4 by equilibrium dialysis is often normal but may be low
2. Medications such as phenobarbital, glucocorticoids, sulfonamides
3. Sighthound breeds (such as greyhounds, salukis, others) may normally have lower concentrations of thyroid hormones than other breeds
G. Treatment
1. Supplemental T 4: 0.01 mg/lb once to twice daily
2. Fatty foods improve absorption of T 4
3. Peak absorption of supplement typically occurs about 3 to 4 hours after ingestion of supplement
4. Monitor thyroid hormone levels 3 to 4 weeks after starting supplement
5. Signs of hyperthyroidism such as anxiousness, panting, and hyperactivity may occur if the T 4 supplement dose is excessive
6. If thyroid supplement has been started before a definitive diagnosis of hypothyroidism, all supplements must be stopped for 4 to 6 weeks before testing thyroid function to determine whether hypothyroidism is actually present
IV. Hypothyroidism in cats
A. Naturally occurring is rare
B. Clinical signs include dwarfism, stunted growth, apathy, lethargy, constipation, thickened skin, seborrhea
C. Thyroid hormone concentrations are low, and TSH is elevated
D. Treatment with T 4: 0.01 to 0.02 mg/kg/day
V. Hyperthyroidism in cats
A. The average age for hyperthyroid cats is 12 to 13 years. Less than 5% of cases are in cats younger than 10 years
B. Hyperthyroidism is usually due to benign adenomatous hyperplasia. Thyroid carcinoma is rare
C. Clinical signs include weight loss, palpable goiter, polyphagia, polyuria, polydipsia, tachycardia, hyperactivity, diarrhea, cardiac abnormalities
D. Clinical pathology findings
1. Increased alanine aminotransferase (ALT), aspartate aminotransferase (AST), alkaline phosphatase (ALP), phosphorus
2. Azotemia in 25%
3. Mild hyperglycemia
4. Stress leukogram, mature neutrophilia
E. Diagnosis
1. Significantly elevated thyroid hormones in many cases of hyperthyroidism
a. Thyroid hormones may be normal or only slightly increased
b. May need to perform a T 3 suppression test to demonstrate loss of negative feedback
c. Day-to-day fluctuation in thyroid hormone production may result in normal thyroid hormone concentrations
d. Concurrent nonthyroidal illness with hyperthyroidism may suppress hormone concentrations into normal range
F. Treatment
1. Surgical thyroidectomy
2. Radioactive iodine therapy
3. Chronic methimazole therapy 5 mg twice or three times daily
G. Complications of therapy
1. Transient or permanent hypoparathyroidism post surgery
2. Hyperthyroidism may recur
3. Reduced glomerular filtration rate (GFR)
4. Renal failure in subclinical or compensated renal failure cases
VI. Hyperthyroidism in dogs
A. Most thyroid tumors are carcinomas and are invasive
B. Hyperthyroidism occurs in about 10% to 20% of thyroid carcinomas. Most thyroid tumors are nonfunctional and do not cause hyperthyroidism
C. Clinical signs include visible neck mass, coughing, dyspnea, dysphagia, dysphonia, weight loss, hyperactivity
D. Treatment
1. Surgery and chemotherapy
2. Treatment with oral thyroxine is recommended post surgery to suppress TSH and to prevent stimulation of potentially precancerous cells
DISORDERS OF ADRENAL FUNCTION
I. Normal adrenal function
A. Adrenal cortex has three zones
1. Zona glomerulosa secretes primarily mineralocorticoids
2. Zona fasciculata secretes primarily glucocorticosteroids
3. Zona reticularis secretes primarily sex hormones
B. Pituitary gland normally secretes endogenous adrenocorticotrophic hormone (eACTH), which acts on the adrenal cortex to cause release of primarily cortisol. As cortisol increases, negative feedback mechanisms cause a decrease in production of eACTH
II. Tests for adrenal function
A. Tests to help support a diagnosis of hyperadrenocorticism (HAC)
1. Low-dose dexamethasone suppression test (LDDST)
a. Blood sample collected before administration of dexamethasone
b. Dexamethasone given intramuscularly at 0.01 mg/kg
c. Post-samples taken 3 to 6 hours post and 8 hours post dexamethasone
d. Measure cortisol concentration in samples
e. Post dexamethasone cortisol concentration greater than 30 to 40 nmol/L suggests HAC
f. Suppression of cortisol concentration greater than 50% of baseline (but still greater than 30 to 40 nmol/L) at 3 to 6 hours post or 8 hours post dexamethasone suggests pituitary-dependent hyperadrenocorticism (PDH)
g. Suppression of cortisol concentration less than 50% of baseline (but still greater than 30-40 nmol/L) could indicate either PDH or an adrenal tumor (not diagnostic for adrenal tumor)
h. If the LDDST is normal, HAC is unlikely
i. False-positive results are seen especially when other illnesses such as diabetes mellitus (DM) are present
j. Test not appropriate if there is a history of exogenous steroid use
2. ACTH response test
a. Test of choice if suspect iatrogenic HAC or hypoadrenocorticism, or when monitoring HAC therapy
b. Measures adrenocortical reserve
c. Baseline blood sample taken before administration of ACTH
d. Depending on the type of ACTH used, the post sample is taken 1 or 2 hours after ACTH
e. Cortisol is measured in both samples
f. Post ACTH cortisol concentration greater than 550 to 600 nmol/L suggests HAC
g. False-positive and false-negative results occur
h. Disadvantage is that this test offers no insight as to the origin of HAC
3. Urinary cortisol-to-creatinine ratio (UCCR)
a. Have owners collect morning urine at home (nonstressed environment)
b. If UCCR results are normal, HAC is very unlikely
c. Convenient, inexpensive test with little stress on patient
d. May be elevated in response to stress or other illness
e. Elevation of UCCR is not diagnostic for HAC
4. Corticosteroid-induced ALP (ciALP)
a. If not elevated, HAC is very unlikely
b. May be elevated in response to stress, glucocorticoid administration, or other illness
c. Elevation of ciALP is not diagnostic for HAC
B. Tests for differentiating the origin of HAC
1. Dexamethasone suppression
a. Low- or high-dose (0.1 mg/kg) dexamethasone suppression
b. Greater than 50% suppression of cortisol from baseline sample suggests PDH
d. High-dose dexamethasone suppression test should not be used for the diagnosis of HAC as some pituitary tumors will remain responsive to a high dose of dexamethasone and show normal suppression
2. Endogenous ACTH measurement
a. Concentration is very low with adrenal tumors because of negative feedback of excess cortisol on pituitary production of endogenous ACTH
b. Concentration of endogenous ACTH may be slightly subnormal, normal, or elevated in cases of PDH
c. Sample handling is critical since endogenous ACTH is very labile
3. Abdominal ultrasound
a. With an adrenal tumor, one adrenal gland may be enlarged and irregular in contour
b. With PDH, both adrenals are enlarged to a similar degree
III. HAC: Canine
A. Pathogenesis
1. PDH is caused by a pituitary microadenoma, macroadenoma, or adenocarcinoma
2. Adrenal-dependent HAC is caused by an adrenal adenoma or adenocarcinoma
3. Iatrogenic HAC is due to chronic exogenous steroid administration
a. Chronic steroid use causes clinical signs of HAC with suppression of cortisol production by the adrenal glands
b. Ear and eye medications containing steroids are readily absorbed and can cause iatrogenic HAC
c. The ACTH response test is the test of choice if iatrogenic HAC is suspected. Resting cortisol concentration is typically low with subnormal stimulation of cortisol with the administration of ACTH
d. Treatment is to remove the source of the exogenous steroids
e. Suppression of adrenal cortisol production from exogenous steroid administration may last 4 weeks or longer, depending on type of steroid used, the route of administration, and the duration of therapy
B. Signalment
1. Middle-aged to older dogs
a. PDH, approximately 7 to 9 years old (range, 2 to 16 years)
b. Adrenal tumor, approximately 11 to 12 years old (range, 6 to 16 years)
2. Sex predilection
a. No difference in PDH
b. More females than males are affected with adrenal tumors
3. Breed predilection
a. Any breed may be affected
b. PDH: Poodles, dachshunds, and small terriers (Yorkshire terrier, Parson Russell terrier, Staffordshire bull terrier) at increased risk
c. Adrenal tumor is more frequent in large breeds (weighing more than 20 kg)
C. Clinical signs
1. Polyuria or polydipsia
2. Polyphagia
3. Abdominal distension (pot-bellied appearance)
4. Muscle wasting and weakness
5. Lethargy, poor exercise tolerance
6. Skin thinning, decreased elasticity of skin, calcinosis cutis, hyperpigmentation
7. Symmetrical alopecia
8. Persistent anestrus or testicular atrophy
D. Clinical pathology findings
1. Findings are nonspecific
2. Stress leukogram: Mature neutrophilia, lymphopenia, eosinopenia, monocytosis
3. Hyperglycemia with or without glucosuria
4. Hypercholesterolemia, hypertriglyceridemia
5. Increased corticosteroid-induced ALP (ciALP), increased ALT, increased bile acid concentrations
6. Decreased thyroid hormone concentrations (with no elevation of TSH)
7. Decreased urine specific gravity (USG), increased incidence of urinary tract infections
E. Radiography findings
1. Nonspecific findings
2. Hepatomegaly, increased abdominal fat
3. Distended urinary bladder, cystic calculi
4. Soft tissue calcification
F. Diagnosis
1. Diagnosis is based on a combination of clinical signs and appropriate adrenal function test findings. The test of choice for diagnosis of naturally occurring HAC is the low-dose dexamethasone suppression test
2. False-positive and false-negative results occur with any adrenal function test
3. Stress of other concurrent illness often causes false-positive results (especially DM)
4. Borderline or positive test results in the absence of clinical signs is probably not HAC
5. An elevated resting cortisol concentration or elevated ALP concentration is not specific for HAC
6. Once a diagnosis of HAC has been made, further testing should be performed to determine the cause of the HAC
G. Treatment
1. Iatrogenic HAC: remove source of exogenous steroids
2. Adrenal tumor
a. Surgery is the treatment of choice, but it may be difficult because adrenal tumors are very vascular
(1) Mitotane is used at higher doses than in PDH, with longer periods of induction
(2) Frequent monitoring (with ACTH response test) necessary
(3) Median survival time is 11 months
3. PDH
a. Surgery to remove the pituitary mass has very limited availability
b. Medical therapy
(1) Mitotane
(a) Causes destruction of the adrenal cortex
(b) Induction phase (25 to 50 mg/kg daily) followed by the maintenance phase (25 to 50 mg/kg once to twice weekly)
(c) Monitor with ACTH response test
(d) Oversuppression of cortisol production can occur, resulting in hypoadrenocorticism
(2) Trilostane
(a) Inhibits glucocorticoid, mineralocorticoid, and adrenal androgen production
(b) Daily medication
(c) Monitor with ACTH response test
(3) l-Deprenyl (selegiline hydrochloride)
(a) Long-term results are disappointing
(b) No severe adverse side effects
(c) Use clinical signs to monitor effectiveness
(4) Ketoconazole
(a) Suppresses steroidogenesis
(b) Monitor using ACTH response test
H. Atypical HAC (dogs)
1. Clinical signs of HAC are present, but dogs have normal cortisol values after adrenal function testing
2. Perform an ACTH response test, and measure intermediates in the cortisol pathway and sex steroids (progesterone, 11-deoxycorticosterone, 17-hydroxyprogesterone, androstenedione, dehydroepiandrosterone, testosterone, estradiol)
3. Abnormal elevations of intermediates or sex steroids in response to ACTH administration may suggest an adrenal tumor
a. Elevated 17-hydroxyprogesterone can occur with either pituitary or adrenal tumors
b. Elevated 17-hydroxyprogesterone can also occur with nonadrenal illness
4. If an adrenal tumor is present, adrenalectomy is the treatment of choice. Patients may also be treated with mitotane or trilostane
IV. HAC: Feline
A. Signalment
1. Uncommon in the cat; disease of middle-aged to older cats
2. Most cases are PDH
3. Most cats have concurrent DM
B. Clinical signs
1. Polyuria or polydipsia (usually secondary to DM)
2. Pot-bellied appearance
3. Polyphagia
4. Muscle wasting
5. Hair loss, thin skin, fragile skin
6. Lethargy, obesity, weight gain
C. Diagnosis
1. Clinical pathology
a. Hyperglycemia, glycosuria
b. Lymphopenia, eosinopenia, monocytosis
c. Hypercholesterolemia, increased ALT, increased ALP
2. Adrenal function tests
a. ACTH response test
b. Dexamethasone suppression test
D. Treatment
1. Adrenalectomy is the most successful method of treatment
a. Unilateral if adrenal tumor
b. Bilateral if PDH. Will require mineralocorticoid and glucocorticoid supplementation
c. May have increased risk of infection and delayed wound healing
2. Hypophysectomy for PDH (not readily available)
3. Medical therapy has been disappointing
V. Hypoadrenocorticism
A. Pathogenesis
1. Primary hypoadrenocorticism with deficiency of both glucocorticoid and mineralocorticoid production
a. Deficiency of glucocorticoid and mineralocorticoid
b. Idiopathic adrenocortical atrophy is most common due to immune-mediated destruction
c. Mitotane-induced adrenocortical necrosis
d. Bilateral adrenalectomy
e. Other causes such as hemorrhage, infarction, neoplasia, granulomas of adrenal glands
2. Secondary hypoadrenocorticism
a. Deficiency of eACTH production or release
b. Mineralocorticoid production is normal
c. Caused by tumors of pituitary or hypothalamus or prolonged suppression of ACTH by drug therapy
B. Signalment
1. Very rare in cats
2. Age: Young to middle-aged dogs (median, 4 years old; range, 3 months to 14 years)
3. Gender: Approximately 70% of cases are female
4. Breed: Any breed can be affected; however, incidence is greater in the Great Dane, Portuguese water dog, rottweiler, standard poodle, West Highland white terrier, soft-coated wheaten terrier, Great Pyrenees, bearded collie, Chinese crested
C. Clinical signs
1. Acute (life-threatening)
a. Hypovolemic shock
b. Collapse
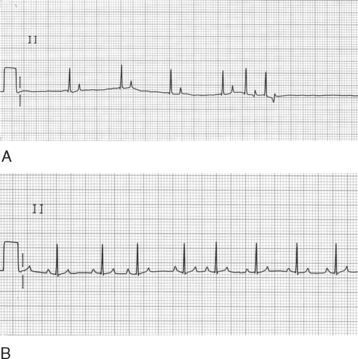 |
| Figure 15-1 Electrocardiograms from a 4-year-old bearded collie dog with primary hypoadrenocorticism taken (A) before and (B) after supplementation with glucocorticoids and mineralocorticoids. Paper speed is 25 mm/sec and sensitivity is 1 cm = 1 mV. A, The P waves are absent, the T waves are peaked, and there is profound bradycardia. The serum sodium concentration was 138 mEq/L and the serum potassium 9.5 mEq/L. B, Electrocardiogram after treatment showing sinus arrhythmia. The serum sodium concentration was 142 mEq/L and the serum potassium 5.4 mEq/L. (From Ettinger SJ, Feldman EC. Textbook of Veterinary Internal Medicine, 6th ed. St. Louis, 2005, WB Saunders.) |
d. Hypothermia
e. Abdominal pain, vomiting, diarrhea
2. Chronic
a. Vague, nonspecific signs exacerbated by stress
b. Waxing and waning course
c. Episodic weakness and collapse
d. Anorexia, weight loss, failure to gain weight
e. Lethargy, depression
f. Vomiting, diarrhea, melena, abdominal pain
g. Polyuria, polydipsia
D. Diagnosis
1. Clinical pathology
a. Lymphocytosis, eosinophilia, neutropenia
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


