CHAPTER 11 Cerebrospinal Fluid
Diagnosis and clinical management of nervous system disease involve a careful assessment of the history and environment, a complete physical examination, and a neurologic examination. Ancillary diagnostic procedures may include hematologic measurements, serum chemistry assays, serologic tests, toxicologic assays, radiographic procedures, and cerebrospinal fluid (CSF) analysis. These test results, in combination with the clinical findings, are used to formulate a differential diagnosis, make a definitive diagnosis, decide treatment, and determine a prognosis.
CSF is produced by ultrafiltration and active transport in the choroid plexus of the brain. The fluid circulates in the subarachnoid space and is absorbed by arachnoid villi associated with venous sinuses in the central nervous system (CNS).1,2 CSF is in direct contact with the brain and spinal cord and functions to cushion, protect, and nourish these delicate tissues.
The usual laboratory analysis of CSF consists of gross inspection, cell counts, measurement of protein content, and cytologic examination. On the basis of these preliminary results and the differential diagnosis, additional tests may be indicated, such as cultures for bacteria and fungi. Other measurements include enzyme activities, electrolyte concentrations, glucose content, antibody titers, and polymerase chain reactions for detection of specific antigens.3 The clinician can use alterations detected in the CSF to make a definitive diagnosis. CSF with abundant neutrophils, increased protein content, and numerous bacteria confirms a diagnosis of septic meningoencephalitis. In other cases, CSF results may be less conclusive but can help categorize the disease as infectious, inflammatory, metabolic, toxic, traumatic, degenerative, or neoplastic.
Sample Collection
CSF can be collected from either the atlanto-occipital or the lumbosacral region of the spine.1,4 The neurologic examination and clinical condition of the horse determine the collection site.5 Lesions localized to the brain and cervical spine are most likely to produce abnormalities in CSF collected from the atlanto-occipital site. Lumbosacral collection is most appropriate for lesions in the caudal segments of the spinal cord. For some horses, comparison of the results for CSF collected from both sites can be helpful in lesion localization. Collection of CSF from either site requires correct positioning, adequate restraint, appropriate needles, surgical preparation of the skin, and availability of specimen tubes. Atlanto-occipital collection is limited to comatose horses or those under general anesthesia because immobilization and lateral recumbency are necessary for collection. Collection of CSF from the lumbosacral site can be achieved in the standing adult horse. In foals, CSF can be collected from either site with the animal in lateral recumbency.6 People involved in the collection and laboratory analysis should exercise extreme caution if rabies is being considered in the differential diagnosis.
CSF should be collected into sterile, clear-glass or plastic-capped vials. An aliquot can be removed aseptically from the tube and used for cell counts, total protein concentration, and cell identification. The remainder of the specimen can be used for microbial culture or chemistry assays if indicated. Although most CSF specimens do not clot, a tube containing EDTA should be readily available in case the fluid is bloody or purulent. If the fluid is bloody on initial penetration, several tubes should be available so that multiple aliquots can be collected to see if the fluid clears. A recent study in horses revealed that blood contamination diminished significantly as three or four 2-ml aliquots of CSF were removed sequentially from the lumbosacral site.7
Atlanto-Occipital Technique
For atlanto-occipital collection the horse is placed in lateral recumbency with the neck flexed such that the longitudinal axis of the head and cervical spine are at a right angle.4,8 The nose is elevated to a horizontal plane. The subarachnoid space is located at a depth of 5 to 8 cm in adults and 2 to 4 cm in foals. A 9-cm, 18- to 20-gauge styletted spinal needle is used for adult horses. A 4-cm, 20-gauge disposable needle is appropriate for foals. The needle is inserted through the skin at the intersection of a line drawn between the cranial border of the wings of the atlas and the dorsal midline, which is identified by palpating the external occipital protuberance (Fig. 11-1). The needle is directed perpendicular to the cervical spine toward the rostral end of the mandible. Some resistance is encountered as the needle passes through the funicular part of the ligamentum nuchae. The needle is advanced until the atlanto-occipital membrane and dura mater are penetrated, which is perceived as a “popping” sensation or as a sudden absence of resistance. When either sensation is detected, the stylet is removed to allow CSF to flow. Position of the needle should not be adjusted without the stylet in place. The neck or head should not be moved while the needle is close to the subarachnoid space.
Lumbosacral Technique
The lumbosacral site can be accessed in most standing adult horses with a 15- to 20-cm, 18-gauge styletted spinal needle after infiltration of the skin and subcutis with local anesthetic. For large horses (12 to 17 hands tall) a 20-cm styletted spinal needle is suggested. A 20- to 23-cm needle may be required for draft horses over 17 hands tall.4,8 Anatomic landmarks are the tuber sacrale of the ilium and the dorsal midline. The needle is inserted through a stab wound located at the intersection of a line drawn between the cranial edges of each tuber sacrale and the midline, which is localized by palpating the spinous processes of the sixth lumbar vertebra and the second sacral vertebra (Fig. 11-2). A depression in the skin is often located in this area. The needle is directed perpendicular to the long axis of the vertebral column and advanced with stylet in place until the interarcuate ligament, dura mater, and arachnoid membrane are penetrated, as identified by a popping sensation or decreased resistance. Average depth of the subarachnoid space is 13 cm in adults. Entry of the needle into the subarachnoid space may be accompanied by excitement, tail movement, flexion of the pelvic limbs, or contraction of the axial muscles.1
Laboratory Assessment
As with other body fluids, the laboratory analysis of CSF consists of inspection of gross appearance, cell counts, measurement of protein content, cell identification, and special chemistry assays.9 Cells, especially neutrophils, degenerate and lyse rapidly in CSF because of its low protein content and its electrolyte concentrations, which are different from corresponding plasma values. Therefore, procedures for cell counts and preparation of smears on glass slides for cell identification should be done within 30 minutes of collection. Cells can be preserved for preparation of glass slides by mixing 8 to 10 drops (0.25 ml) of fresh CSF with 1 ml of 40% ethanol or by adding autologous serum to the sample. The addition of 1 drop of autologous serum to 0.25 ml of CSF will preserve cell morphology and differential counts for 48 hours when stored at 4° C.10 Measurement of protein content and special assays can be done on CSF that is refrigerated or frozen without additives.
Macroscopic appearance
Visual inspection of the color and turbidity of CSF is best done by viewing the specimen through natural sunlight or against a white background.8 A white index card with lines provides a background for accurate color assessment and fine lines to detect turbidity.
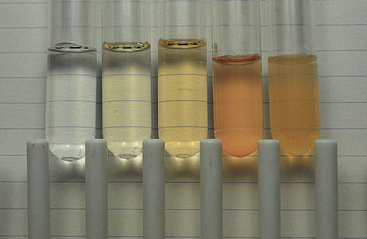
Normal CSF is clear, colorless, and watery and does not form a clot.3,8 Any deviation in color or turbidity is considered abnormal, and the cause should be determined. Causes of CSF turbidity include elevated cell count, presence of microorganisms, or a marked increase in protein content.1,8 Cell counts greater than 400 to 500 μl are necessary before CSF becomes turbid. The presence of myelographic contrast media or fat aspirated during collection may cause turbidity.5 Abnormal colors encountered in the macroscopic assessment of CSF are red tinged, bright red, xanthochromic, and opaque white (Fig. 11-3). Cloudy CSF with a white tinge indicates a marked increase in nucleated cells. Red-tinged or bright-red fluid indicates pathologic or iatrogenic hemorrhage.1,4,8
Subarachnoid hemorrhage resulting from disease is recognized by a red-tinged or bloody CSF that has a xanthochromic supernatant. Xanthochromia is a yellow-orange coloration of the CSF caused by erythrocyte breakdown products, oxyhemoglobin, and bilirubin.8 Other causes include a marked increase in CSF protein (>400 mg/dl) and severe icterus, which allows plasma bilirubin to cross the blood-CSF barrier. Subarachnoid hemorrhage may cause release of oxyhemoglobin from lysed erythrocytes. Xanthochromia forms in 2 to 4 hours, peaks at 24 to 36 hours, and may persist for 4 to 8 days.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree