Oral Calcium Supplementation in Peripartum Dairy Cows
Garrett R. Oetzel, DVM, MS, Food Animal Production Medicine, Department of Medical Sciences, School of Veterinary Medicine, University of Wisconsin–Madison, 2015 Linden Drive, Madison, WI 53706, USA. E-mail address: groetzel@wisc.edu
Keywords
Milk fever
Subclinical hypocalcemia
Hypocalcemia treatments
Sources of calcium for oral supplementation
Oral calcium supplementation strategies
Introduction
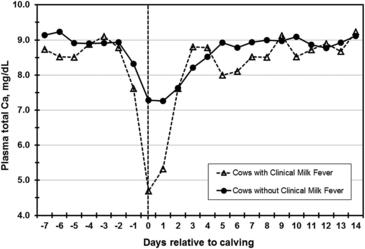
The initiation of lactation challenges a dairy cow’s ability to maintain normal blood calcium concentrations. Milk (including colostrum) is rich in calcium, and cows must quickly shift their priorities to adjust for this sudden calcium outflow. Average blood calcium concentrations noticeably decline in second or greater lactation cows around calving, with the lowest concentrations occurring approximately 12 to 24 hours after calving (Fig. 1).1,2 The extent to which hypocalcemia occurs around calving is an important determinant of fresh cow health and milk production.
Clinical milk fever versus subclinical hypocalcemia
Clinical milk fever is one of the most recognized diseases of dairy cattle. The clinical signs of milk fever may, for convenience, be divided into 3 stages. Stage I clinical milk fever is early signs without recumbency. It may go unnoticed because its signs are subtle and transient. Affected cattle may appear excitable, nervous, or weak. Some may shift their weight frequently and shuffle their hind feet.3 Cows in stage II milk fever are in sternal recumbency. They exhibit moderate to severe depression and partial paralysis and typically lie with their head turned into their flank.3 Cows in stage III clinical milk fever are in lateral recumbency, completely paralyzed, typically bloated, and severely depressed (to the point of coma). They die within a few hours without treatment.3
Subclinical hypocalcemia is defined as low blood calcium concentrations without clinical signs of milk fever. Subclinical hypocalcemia affects approximately 50% of second and greater lactation dairy cattle fed typical prefresh diets. If anions are supplemented to reduce the risk for milk fever, the percentage of hypocalcemic cows is reduced to approximately 15% to 25%.4
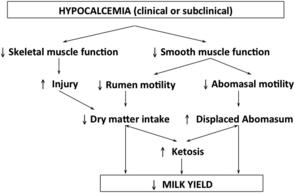
A cow does not necessarily have to become recumbent (down) to be negatively affected by hypocalcemia. With or without obvious clinical signs, hypocalcemia has been linked to a variety of secondary problems in postfresh cows.1,3 This happens because blood calcium is essential for muscle and nerve function—in particular, functions that support skeletal muscle strength and gastrointestinal motility. Problems in either of these areas can trigger a cascade of negative events that ultimately reduce dry matter intake, increase metabolic diseases, and decrease milk yield.1 The pathways by which hypocalcemia may negatively affect cow health and milk production are illustrated in Fig. 2.
Subclinical hypocalcemia is more costly than clinical milk fever because it affects a much higher percentage of cows in the herd.3 For example, if a 2000-cow herd has a 2% annual incidence of clinical milk fever and each case of clinical milk fever costs $300,5 the loss to the dairy from clinical cases is approximately $12,000 per year. If the same herd has a 30% annual incidence of subclinical hypocalcemia in second and greater lactation cows (assume 65% of cows in the herd) and each case costs $125 (an estimate that accounts for milk yield reduction and direct costs due to increased ketosis and displaced abomasum), then the total herd loss from subclinical hypocalcemia is approximately $48,750 per year. This is approximately 4 times greater than the cost of the clinical cases.
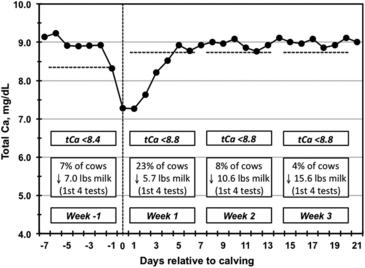
A recently published, large multisite study shows that hypocalcemia around calving was associated with reduced milk yield6 and increased risk for displaced abomasum.7 These studies also demonstrated that the cutpoint for serum total calcium is approximately 8.5 mg/dL, which is a higher concentration than had been previously assumed (Figs. 3 and 4).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree