Tim G. Eastman
Wounds of the Foot
Horses are “fight-or-flight” animals and as such frequently are prone to traumatic incidents. Wounds involving the digit are a common challenge facing equine veterinarians and, depending on the structures involved, may be life threatening. A thorough understanding of the regional anatomy is imperative to accurately diagnose and treat the myriad conditions that affect the digit of horses. This chapter reviews common conditions involving the horse’s foot and discusses their treatment.
Diagnosis
The first step in assessing the severity of a wound involving the equine digit is to determine whether bone, tendons or ligaments, or a synovial structure is involved. The distal interphalangeal joint, podotrochlear bursa, and digital flexor tendon sheath are the synovial structures most frequently involved. To assess communication of one of these structures with a wound, an area remote from the wound should be aseptically prepared and a sterile needle inserted into the synovial structure in question. It is ideal to delay antimicrobial therapy briefly until a sample of synovial fluid has been obtained. Once fluid has been obtained and submitted for aerobic and anaerobic culture and sensitivity as well as cytologic evaluation, local and systemic antimicrobials may be instituted. Total protein concentration greater than 4.0 mg/dL or total nucleated cell counts greater than 30,000 cells/µL are considered highly suggestive of sepsis. At this point, the synovial structure can be distended with a sterile isotonic solution to determine whether the synovial structure communicates with the wound. Given the high incidence of false-negative culture results in synovial structures, cytology can be useful in the short-term for advising horse owners on the likelihood of sepsis. The likelihood of obtaining meaningful culture results can be greatly enhanced by allowing the sample to incubate in blood culture media for 24 hours rather than directly swabbing culture plates. Because cells deteriorate with time and inflammatory synovial fluid tends to clot, collected synovial fluid samples should be processed promptly to enhance the likelihood of obtaining diagnostic cytology information. Cytology frequently reveals a preponderance of polymorphonuclear cells and high protein levels in fluid from septic synovial structures and may reveal phagocytized or free bacteria. Given the severity of the consequences that arise when septic synovial structures are not aggressively treated, wounds in which determination of synovial space penetration is not straightforward should be considered septic until proved otherwise. The collateral cartilages of the third phalanx serve as a useful landmark for assessing involvement of the distal interphalangeal joint, with lacerations axial to this structure frequently having synovial involvement. If sterile fluid injected into the synovial structure at a site remote from the wound fails to egress through the wound, it is unlikely that the synovial structure is involved at that time. Practitioners should remember, however, that delayed extension of infection into the synovial structure secondary to necrosis of the surrounding tissues is possible.
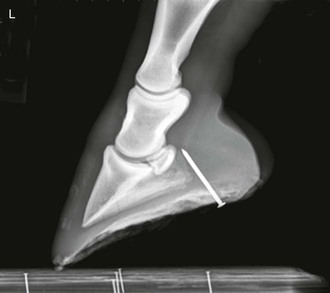
Puncture wounds of the foot frequently represent a diagnostic challenge. It is ideal to radiograph the foot with the penetrating foreign body still in situ (Figure 196-1), but frequently the offending object (most often a nail) has been removed before the time of first evaluation by the veterinarian. The remaining tract can be very difficult to localize after the foreign body has been removed. To determine the foreign body’s trajectory into the foot and estimate what structures were involved, a sterile probe can be inserted into the resultant tract if it is identifiable (Figure 196-2).
Contrast fistulography can also be useful in identifying involvement of adjacent structures. If the tract is not readily recognizable, an attempt should be made to obtain a fluid sample from all synovial structures in the vicinity. Sometimes communication with the bottom of the foot can be confirmed by pressurizing the adjacent synovial structure (e.g., the podotrochlear bursa) and observing for egress of synovial fluid through the draining tract.
Treatment
Regardless of the site of entry into a synovial structure, the hallmark of treatment of septic synovitis is aggressive lavage combined with local and regional antimicrobial therapy. Arthroscopic lavage allows for simultaneous debridement of inflamed synovium, removal of inflammatory debris, and high-volume lavage of the structures in question. Multiple portals should be used to prevent a one-way stream effect of fluid through the synovial structure. If the wound is sufficiently large, the wound itself can serve as the egress portal; otherwise, appropriately sized needles (18-gauge and larger) can be inserted to provide outflow of the lavage fluid. Some surgeons prefer to perform regional limb perfusion (RLP) with antimicrobials at the time of the lavage, and others prefer to wait until the lavage is complete so that the antimicrobials are not washed out with the irrigating fluid.
If arthroscopic evaluation and lavage are not possible, a through-and-through lavage performed with needles is the next-best option. The decision to perform this in the standing horse or with the horse under general anesthesia depends on surgeon preference, economics, structures involved, and horse temperament. The author often prefers general anesthesia to enable adequate assessment of the degree to which synovial structures are involved and to facilitate the initiation of treatment.
In the past decade, RLP has become commonplace in the treatment of septic conditions involving the foot in horses. The once popular “streetnail” procedure has waned in popularity given the success realized with serial RLP and the associated decreased convalescence time.