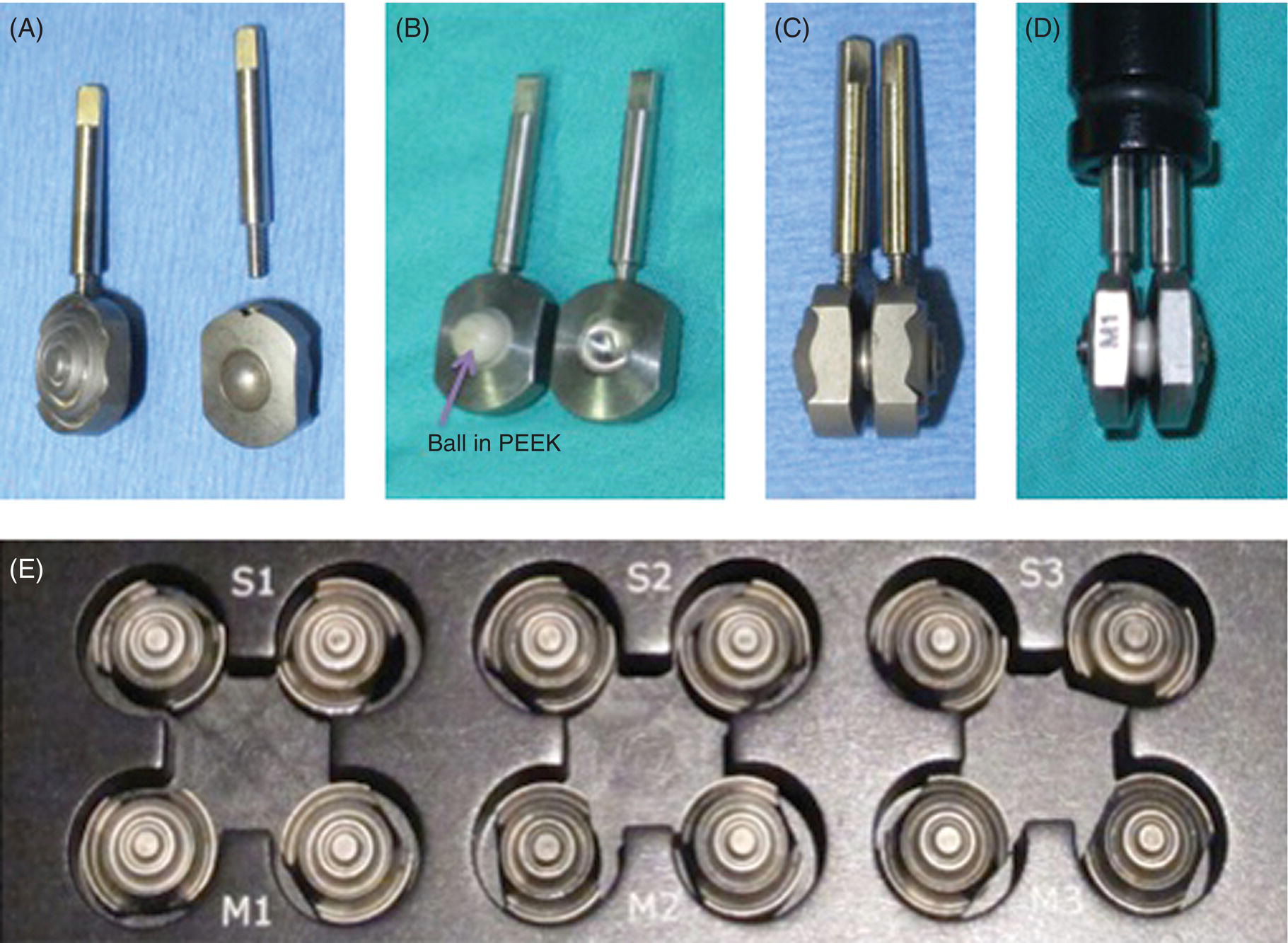
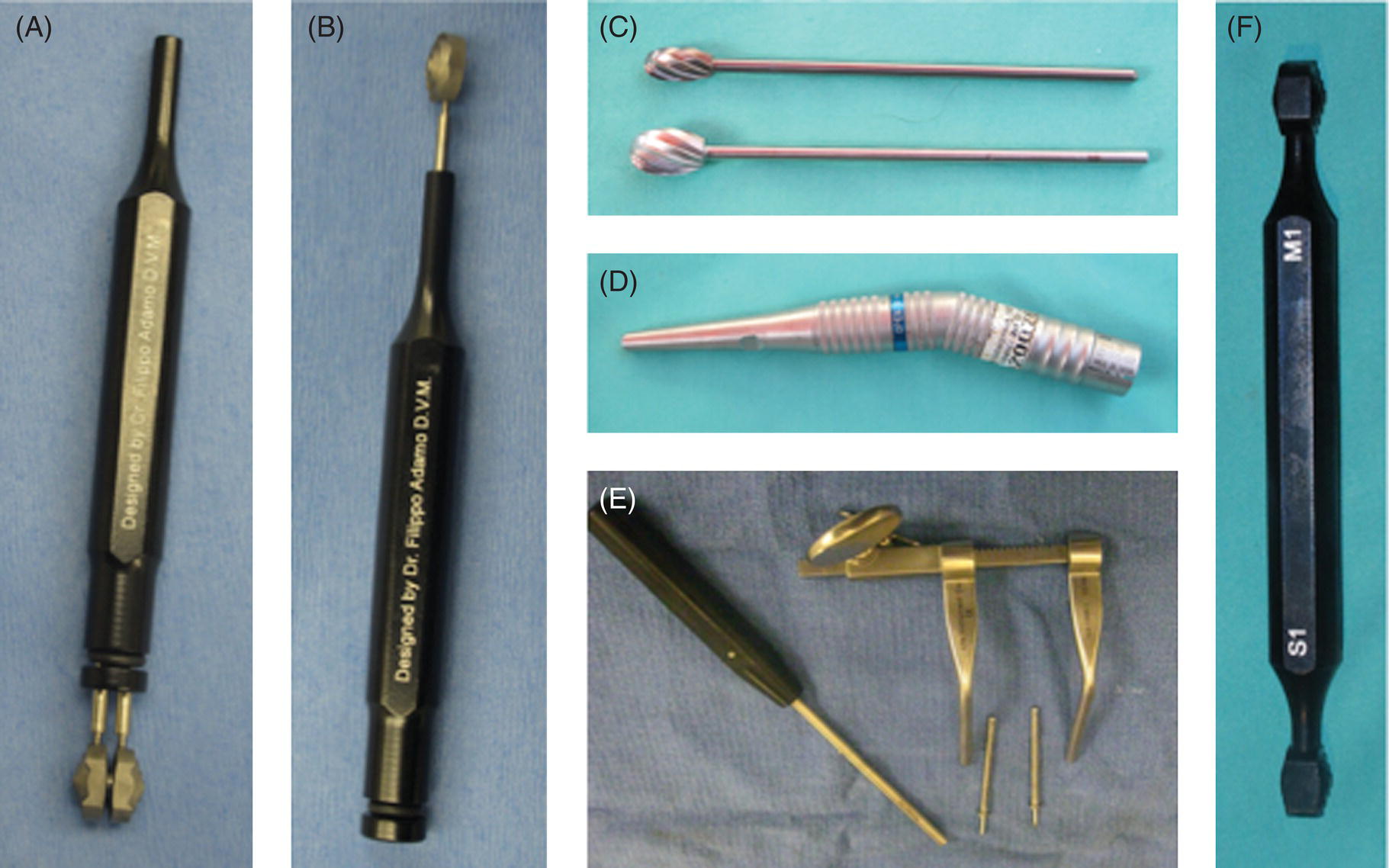
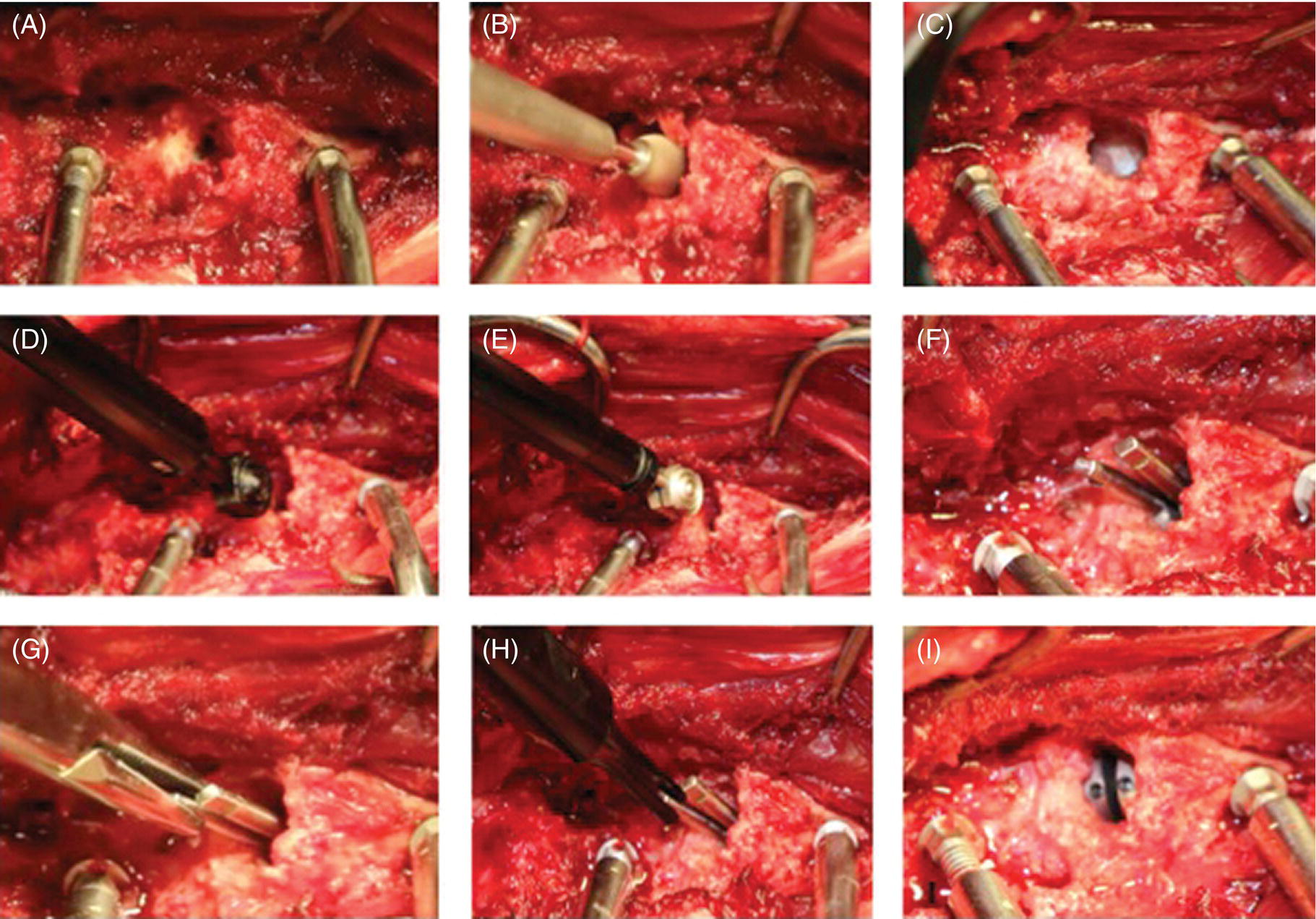
40 Filippo Adamo and Franck Forterre Spinal arthroplasty offers an exciting alternative to fusion for the treatment of degenerative disc disease. Currently, the main indication for disc prosthesis in small animals is the treatment of disc-associated cervical spondylomyelopathy in dogs, also known as disc-associated wobbler syndrome (DAWS) (see Chapter 7). Another potential indication is the treatment of disc-associated lumbosacral stenosis (see Chapter 32). DAWS in dogs shares many similarities with cervical spondylotic myelopathy in people, and the Doberman breed has been proposed as a natural model to study the disease in humans [1]. The knowledge gained over the last 15 years in people with disc arthroplasty can be applied in veterinary medicine for the treatment of DAWS. However, this information should be interpreted cautiously by veterinarians because of biomechanical differences in dogs such as greater axial forces and greater amount of coupled motions in dogs compared to people [2, 3]. The goal of cervical arthroplasty is to preserve intervertebral mobility while providing distraction, stability, and neural decompression [4–6]. Cervical disc arthroplasty involves discectomy, spinal cord decompression, milling of the vertebral end plates, and placement of a device to maintain distraction and preserve intervertebral mobility at the treated space [4–11]. Maintenance of motion at a decompressed interspace may result in improved load transfer and reduced stress on the adjacent intervertebral discs and dorsal elements, although this has not yet been demonstrated conclusively in the canine spine. In people with cervical myelopathy and radiculopathy secondary to degenerative disc disease, anterior cervical discectomy and fusion (ACDF) is a reliable surgical treatment with a satisfactory outcome in 90–95% of patients [12]. However, there is a significant incidence of disc disease at adjacent sites causing recurrence of neurologic symptoms, termed domino effect [12–14]. Within 5 years of surgery, 92% of patients have radiographic evidence of degenerative disc disease at adjacent segments, and by 10 years, about 25% of people require a second surgery for the same problem at an adjacent space [12, 14]. The cause of this subsequent disc degeneration remains unknown. One suggested factor is an increase in intradiscal pressure at adjacent discs after fusion [15–18]. This increased pressure blocks the diffusion of nutrients from the end plate and is the most significant cause of disc degeneration [19]. Clinical studies using dynamic radiography show increased motion at adjacent segments above and below the level of cervical fusion, and this is also a factor associated with deterioration [20, 21]. After arthroplasty, the range of motion is increased or maintained in the surgically treated segment and mildly decreased at adjacent levels. However, this reduction is compensated by the movement of the artificial disc itself [22]. An interesting dilemma regarding domino lesions is whether such lesions are the natural progress of an underlying similar process at the adjacent vertebral motion units or if they are an accelerated degenerative process influenced by the biomechanical effect of fusion [21–23]. Motion preservation at the surgery site may reduce the rate of adjacent-level cervical disc disease [24–28]. The use of a cervical disc prosthesis in human patients was first reported by Ferstron in 1966 [29]. Over the last decade, clinical experience with many different types of artificial discs has been reported, including Cummins artificial cervical joint [30] (which evolved into Prestige [31], ProDisc-C [32], Bryan Cervical Disc [33], Discover [34, 35]), and several clinical trials are currently underway [28]. Currently, artificial discs are classified into three types: non-, uni-, and biarticulating. The implant may consist of a metal-on-metal design, metal-on-polymer (ultrahigh-molecular-weight polyethylene), and less commonly ceramic-on-polymer or a ceramic-on-ceramic design [36]. The disc is either modular (having replaceable components) or nonmodular (without replaceable components) and some are used in conjunction with supplemental vertebral body screw fixation [36]. Certain designs promote biological bone ingrowth at the disc The distribution of force and subsidence is possibly the most important biomechanical consideration for an artificial disc. The idea is to distribute the forces involved as uniformly as possible over a large area [37]. Intradiscal replacement of the nucleus pulposus represents an alternative to total disc replacement and spinal fusion procedures. The aim is to reconstruct the nucleus pulposus primarily while preserving the biomechanics of the annulus fibrosus and cartilaginous end plate. Nucleus pulposus implants are designed to provide stable motion, increase disc space width, relieve or lessen transmission of shear forces on the remaining annulus, and stabilize ligaments [38]. Nucleus pulposus replacement devices can be categorized into two groups: the intradiscal implants and in situ curable polymers. Intradiscal implants are biomechanically more similar to the native nucleus pulposus, whereas in situ curable polymers consist of compounds that harden after implantation. These implants are currently at different stages of preclinical and clinical investigations in veterinary medicine [39; F. Forterre, personal communication]. The first cervical prosthesis specifically for the canine cervical spine1 was designed and biomechanically tested in vivo in 2007 [7]. This prosthesis is made of a titanium alloy (Ti-6AI-4 V-ELI) and consists of two end plates, with a range of movement of 30o between the plates (Figure 40.1). Titanium alloy was selected because it is resistant, is relatively inexpensive, has a good corrosion resistance compared to other materials, and is ideal for follow-up MRI studies in the event of postsurgical worsening and to evaluate domino lesions. This prosthesis is rotationally unconstrained, following the ball-and-socket principle, and does not require supplemental fixation. Unconstrained cervical prostheses designed for people usually allow about 11° of freedom [24]. The higher degree of freedom in this prosthesis was arbitrarily chosen considering that heterotopic ossification at the treated site observed in people significantly decreases the range of motion at the site of implantation over time. The outer surface of each end plate is convex to avoid prosthesis migration and has concentric grooves to allow bone ingrowth into the prosthesis. In the in vitro study, it was concluded that cervical spine specimens with the implanted prosthesis have biomechanical behaviors more similar to an intact spine compared to spinal specimens with ventral slot and PMMA fusion [7]. This was the prerequisite for the subsequent clinical investigation [8–10]. Figure 40.1 Adamo spinal disc®. US Patent # 8,496,707 B2. The prosthesis is made of a titanium alloy, and the concavity and convexity of the central aspects of the end-plate surfaces result in a ball-and-socket type of connection between the end plates. The external surface of each end plate is convex, resembling the concavity of the caudal end plate of the most caudal cervical vertebrae. The outer surface of each end plate has concentric grooves to allow bone ingrowth into the implant and is pretreated with a dual acid etch bath to promote bone ingrowth into the prosthesis (A). The convexity of the central aspect of the end-plate surface is made of polyether ether ketone (PEEK) (B). Two end-threaded stainless steel pins screwed into each piece of the implant and a barrel holder are used to hold together the two pieces of the implant during placement within the disc space (C and D). Six standard sizes of prosthesis are available, labeled S1, S2, and S3 and M1, M2, and M3. However, since each male piece of the prosthesis has to be assembled with a separate female piece, this makes a total of 12 different sizes when the disc is assembled in all possible combinations (E). A pilot long-term clinical study using this prosthesis in two dogs affected by DAWS showed that cervical arthroplasty was well tolerated with excellent outcome in both dogs. Mobility at the treated site was lost and distraction decreased over time in both dogs, without affecting the clinical outcome. Furthermore, the presence of the prosthesis did not affect the ability to reassess the area via MRI at a follow-up 18 months later, and domino lesions were not observed in either dog [9]. A multicenter study evaluating the short and intermediate clinical and radiological results (average 15 months) using the same prosthesis in 12 dogs with single- and multilevel lesions has been reported [10]. In this study, the external surface of the prosthesis was treated with dual acid bath etch [40, 41] to promote bone–implant incorporation at the implant–vertebral end-plate interface, and dedicated surgical tools were created to facilitate implantation (Figure 40.2). To improve visual assessment, a high-powered headlamp, magnification loupes, and a Caspar cervical distractor were used as in the previous study (Figure 40.3). All 12 dogs had immediate postoperative recovery with good degree of distraction in the immediate postoperative radiographs (Figure 40.4). All dogs in this study, except one in which the technique was improperly performed, showed improvement in the neurological status during the observation period. In the majority of dogs, the distraction was moderately lost, and mobility at the treated sites decreased or became undetectable over time (Figure 40.5). A subsequent study using a redesigned thinner disc (2nd-generation disc) with the internal convex surface replaced with polyether ether ketone (PEEK) and an additional tool (sizing probe) to probe/test the disc space during burring before final disc implantation showed similar results but with the advantages that the surgery was facilitated by less burring and less implant manipulation and the implant accommodated easier along the natural angle of the disc space [11]. A recent study evaluating 50 disc spaces in 33 dogs treated with CDA for DAWS showed that on the immediate postoperative radiographs, 15 sites were overdistracted, 34 sites were adequately distracted, and only 1 site was underdistracted. Overdistraction was mostly observed with the 1st-generation (thicker) implant, while the adequate distraction was mostly observed with the 2nd-generation (thinner) implant. On serial radiographic evaluation, the distraction was gradually decreased compared to the immediate postoperative radiographs and subsidence (defined as reduction of the width of the disc space equivalent to or less than the width of the preoperative radiographs) was seen in 7/19 sites (37%) at 6 months postsurgery and progressed to all the five sites evaluated at 2 years postsurgery. Subsidence, except for one dog, was seen only when the disc spaces were overdistracted, and it was more pronounced with the 1st-generation (thicker) and narrower implants and less pronounced with the 2nd-generation (thinner) and wider implants (Adamo, personal observation). Mobility was not detectable in 8/36 treated sites (22%) 2 weeks after surgery in 24 dogs examined and was lost or not detectable in 17/22 sites (77%) at 6 months after surgery in 14 dogs examined. No implant migration or implant infections were observed on serial radiographs or on MRI when available. In this study, the mean and median follow up time was 16 and 12 months, respectively (range, 2 weeks to 42 months), and the outcome was considered good to excellent in 30 out of 33 dogs (91%). The three dogs with poor or unsatisfactory outcome were presented with over 2 months of nonambulatory tetraparesis and severe extensor rigidity in both thoracic limbs. Among these, one dog (12.4-year-old sheltie mix weighing 9 kg [19.5 lb]) was euthanized 2 weeks postsurgery because of a compressive fracture of C6 with ventral displacement of the implant, and another dog (13.5-year-old chow mix) was euthanized 8 months after surgery because of lack of significant improvement. Two dogs had recurrence of the neurological signs 18 months after surgery secondary to suspected osteophytes (noted on MRI) causing ventral spinal cord compression at the treated sites. Ventral osteophytes were seen at six treated sites, in four dogs on postoperative radiographs, causing bridging spondylarthrosis and ankylosis at three disc spaces in two dogs. No neurologic domino lesion adjacent to treated sites was seen in any of the dogs during the observation period. Median postoperative hospitalization time was 1 day (range 0–5 days), and 5 dogs were discharged on the day of surgery. In this study, it was concluded that correct patient selection (dog’s weight not less than 20 kg [44 lb]), neurological status at presentation, size of the implant, end-plate preparation, and applied distraction during surgery were important factors that may influence the outcome (Adamo, personal observation). Figure 40.2 Dedicated surgical tools and other accessories. US Patent # 8,491,655 B2. Barrel holder. (A) After the two pieces of the implant are assembled, the two pins are inserted into the barrel holder. (B) The barrel holder has the double function of holding the prosthesis assembled with one extremity and to unscrew the end-threaded pins after the prosthesis is placed in the slot with the other extremity. Custom-made burrs. (C) Two dedicated custom-made burrs are used. The small burr head is used to enlarge the discectomy and to create enough space for the insertion of larger burr. The large head burr resembles the external convexity of the implant, and it is used for the final burring to create the specular concavity to accommodate the implant into the disc space. Twenty degree angle attachment. (D) A 20° angle attachment for the high-speed air drill is used to facilitate burring at an angle parallel to the disc space. Caspar cervical distractor. (E) This instrument is used to distract the two cervical vertebrae at the affected disc space. It allows better visualization of the dorsal aspect of the discectomy, facilitates the removal of the bulging disc, improves visualization of the dorsal longitudinal ligament, and facilitates the inspection of the vertebral canal for adequate spinal cord decompression. Sizing probe. (F) This instrument resembles at each extremity the shape of the S or M disc size, respectively. It is used to probe the discectomy between burring (in place of the implant), and to assess the congruity of the discectomy to the implant. This instrument shortens the total surgery time by avoiding multiple times of checking of the discectomy with the actual implant, and it also facilitates proper selection of the size of the implant after the discectomy is completed.
Will There be a Role for Disc Prostheses in Small Animals?
Introduction
Comparison of DAWS in people and in dogs
Cervical disc prosthesis in people
Classification of artificial discs
–end-plate interface. In terms of motion, artificial discs may be constrained, semiconstrained, or unconstrained [36]. Devices are considered constrained in certain planes if they restrict motion to less than that seen physiologically. Devices are considered semiconstrained in certain planes if they allow motion similar to that seen physiologically. Devices are considered nonconstrained in certain planes of motion if there is no mechanical stop to the motion and if they are reliant on the perispinal soft tissue and the inherent compression across the disc space to provide restraint to extremes of motion [37].
Cervical disc prosthesis in dogs

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


