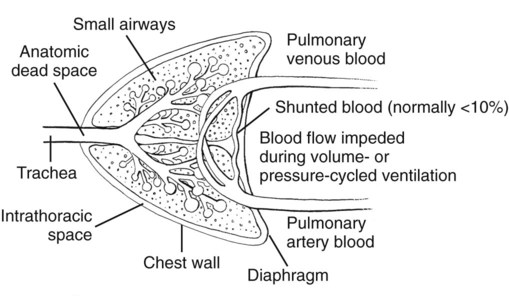
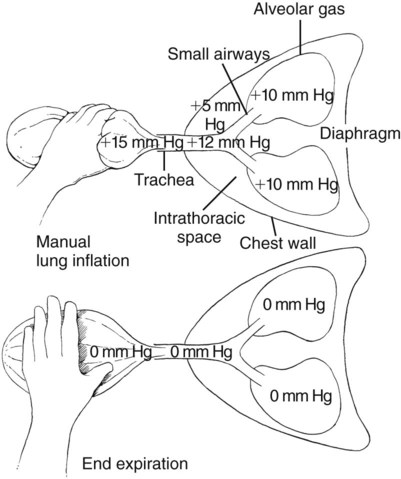
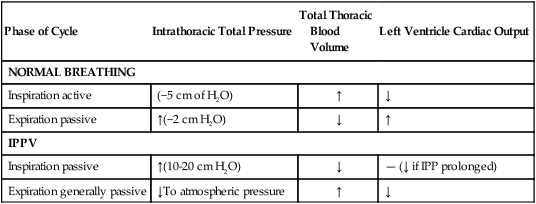
I Manual or mechanical intermittent positive pressure ventilation (IPPV) when properly applied can be used to maintain stable inhalant anesthesia (the drug delivery system is the lung) and blood gases (PO2, PCO2) for prolonged durations with minimal untoward effects II Positive pressure ventilation requires a thorough familiarity with cardiopulmonary physiology, ventilatory equipment and techniques, and blood gas interpretation III Mechanical ventilators inflate the lungs to a predetermined volume (volume cycled) or pressure (pressure cycled) or for a preset time at a predetermined gas flow rate (time cycled). Most anesthesia ventilators consist of a compliant pleated compressible bellows connected to an anesthetic breathing circuit. The bellows is contained within an airtight rigid plastic cylinder that can be pressurized to compress the bellows. Driving gas is cyclically introduced into the cylinder (outside the bellows) causing pressure within the cylinder to increase (inspiratory phase). The bellows is compressed and gas contained therein is delivered to the airway. When pressure within the cylinder is released, the process reverses and the elastic recoil of the lung causes the bellows to expand (expiratory phase). A The breathing circuit must be airtight (no leaks; “closed circuit”) during the inspiratory phase of the ventilation cycle for gas to be directed into the airway and lungs IV Controlled ventilation may be required in animals that are not breathing adequately or that are difficult to keep anesthetized V PaCO2 values and capnometry (ETCO2) provide continuous assessment of ventilatory adequacy (see Chapter 14) I Depression of respiratory centers II Inability to adequately expand the thorax H Bony deformities of the chest wall 1. Weight of abdominal viscera on the diaphragm may impede lung expansion 3. Surgical tie downs and abnormal thoracic limb positioning III Airway obstruction including laryngeal paralysis A Foreign and bodily materials (e.g., stones, sticks, water, mucus, blood) B Trauma (nasal, laryngeal, trachea) E Congenital anomalies (e.g., collapsed trachea or bronchi) IV Inability to adequately expand the lungs I Anesthetics are respiratory depressants; positive pressure ventilation may be required to assist or control breathing A Controlled ventilation helps to ensure adequate alveolar ventilation, aiding in the uptake (inhalants) and elimination of drugs and gases II Special indications for controlled ventilation during anesthesia 1. Controlled respirations minimize spontaneous chest wall movements 2. The lungs cannot be inflated when the chest is open (intrathoracic pressure equals atmospheric) B Neuromuscular blockers (see Chapter 10): neuromuscular blocking drugs paralyze the diaphragm and intercostal muscles producing apnea C Prolonged surgical anesthesia (more than 60 minutes) reduces respiratory effort, especially in horses, resulting in hypoventilation D Chest wall or diaphragmatic trauma a. “Flail chest”: series of adjacent broken ribs resulting in the segment moving independently (chest wall moves in during inspiration instead of out: paradoxical breathing). Usually associated with lung contusion and pneumothorax. E Maintain a more stable plane of anesthesia F Obesity and special positioning G Control of intracranial pressure H Convenience: eliminate concerns about hypoventilation and poor gas exchange (low oxygen [O2]; high carbon dioxide [CO2]) A Normal lungs are well ventilated during spontaneous breathing (Fig. 13-1) 1. Inspiration is active and dependent upon the integrated function of the nervous and musculoskeletal systems 2. Expansion of the rib cage and flattening of the diaphragm increase the volume of the thoracic cavity and the negative pressure in the thoracic cavity, drawing air into the lung 3. Expiration is passive returning lung volume to its original state B The portions of the lung in closest contact with moving surfaces (i.e., the peripheral lung field, diaphragm) undergo the greatest volume changes during spontaneous ventilation C Decreased breathing of hypoventilation causes increases in CO2 (PaCO2 > 45 to 50 mm Hg) 1. Results in respiratory acidosis 2. Activates the sympathetic nervous system 3. Predisposes to cardiac arrhythmias 4. Initially causes peripheral vasoconstriction (sympathetic effect) followed by peripheral vasodilation as a direct effect of CO2 on smooth muscle tone 5. Increased PaCO2 can produce narcosis D Positive pressure ventilation inflates the peribronchial and mediastinal areas of the lung; the peripheral segments are relatively less ventilated compared with normal spontaneous breathing 1. Pressure or volume ventilation increases airway diameter and thus anatomic dead space, reducing alveolar ventilation E Positive pressure ventilation results in a significant reduction in lung compliance; the lung becomes stiffer and predisposes to atelectasis and hypoxemia II Cardiovascular system (Table 13-1) TABLE 13-1 Cardiovascular System: Effects of Breathing and Intermittent Positive Pressure Ventilation IPP, Intermittent positive pressure; IPPV, intermittent positive pressure ventilation. A The subatmospheric pressure within the thorax augments venous return during inspiration; this subatmospheric pressure is made more negative during inspiration by contraction of the diaphragm B The pressure in the airway and lungs is transmitted to the thoracic cavity during controlled ventilation, impeding venous return and potentially decreasing cardiac output (see Fig. 13-1; Fig. 13-2) C Controlled ventilation decreases arterial blood pressure and cardiac output when: 1. Average airway pressure is consistently more than 10 mm Hg 2. Circulating blood volume is low, caused by dehydration and blood loss 3. Sympathetic nervous system activity is impaired, caused by anesthesia, local anesthetics, and shock
Ventilation and Mechanical Assist Devices
Overview
General Considerations
Reasons for Respiratory Inadequacy
Managing Ventilation during Anesthesia
Considerations for and Consequences of Ventilation
Phase of Cycle
Intrathoracic Total Pressure
Total Thoracic
Blood
Volume
Left Ventricle Cardiac Output
NORMAL BREATHING
Inspiration active
(−5 cm of H2O)
↑
↓
Expiration passive
↑(−2 cm H2O)
↓
↑
IPPV
Inspiration passive
↑(10-20 cm H2O)
↓
— (↓ if IPP prolonged)
Expiration generally passive
↓To atmospheric pressure
↑
↓
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree