Chapter 25
Vaginal Cytology
Examination of exfoliated cells from the vagina is a simple technique that is useful to monitor the progression of proestrus and estrus in dogs and cats.1–3 The vaginal epithelium undergoes a predictable hyperplastic response to increasing plasma estrogen concentrations during proestrus. Starting as only a few cell layers, the epithelium becomes 20 to 30 cell layers thick, eventually exfoliating large numbers of superficial epithelial cells during estrus. Vaginal cytology, often in tandem with hormone analysis, may provide valuable information about the stage of the ovarian cycle.4 In addition, vaginal cytology has proven useful to detect inflammatory and neoplastic conditions in the female reproductive tract.5
Vagina
Collecting Vaginal Samples
Cells are obtained by passing a cotton-tipped swab into the caudal vagina (Figure 25-1 and Figure 25-2). A narrow spreading speculum may be used to allow unimpeded swab passage. If no vaginal discharge is present, the swab may be moistened with sterile saline to avoid discomfort. The swab should be directed craniodorsad when entering the vaginal vault to avoid the clitoral fossa; keratinized epithelium normally present in the fossa could lead to an inappropriate cytologic interpretation (Figure 25-3).3 Once cranial to the urethral orifice, the vaginal wall is gently swabbed. The cells are then transferred to a glass slide by gently rolling the swab with minimal pressure to avoid rupturing cells. The smear is allowed to air-dry thoroughly before staining. Romanowsky-type stains typically used for blood films (Wright or modified Wright-Giemsa stains, including quick-type stains) provide good morphologic detail.

Figure 25-1 The labia are carefully parted to allow unimpeded passage of the swab. (Courtesy of Kal Kan Forum.)

Figure 25-2 The swab is directed craniodorsad to avoid entering the clitoral fossa. (Courtesy of Kal Kan Forum.)
Classifying Vaginal Cells
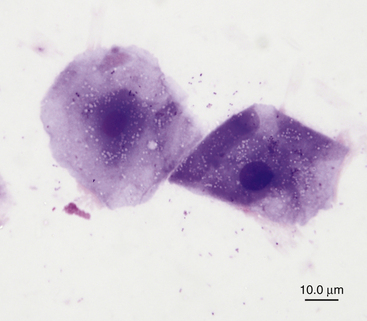
Vaginal epithelial cells are described beginning with the deepest, most immature layer near the basement membrane and progressing superficially to the most mature layer nearest the vaginal lumen (Figure 25-4).
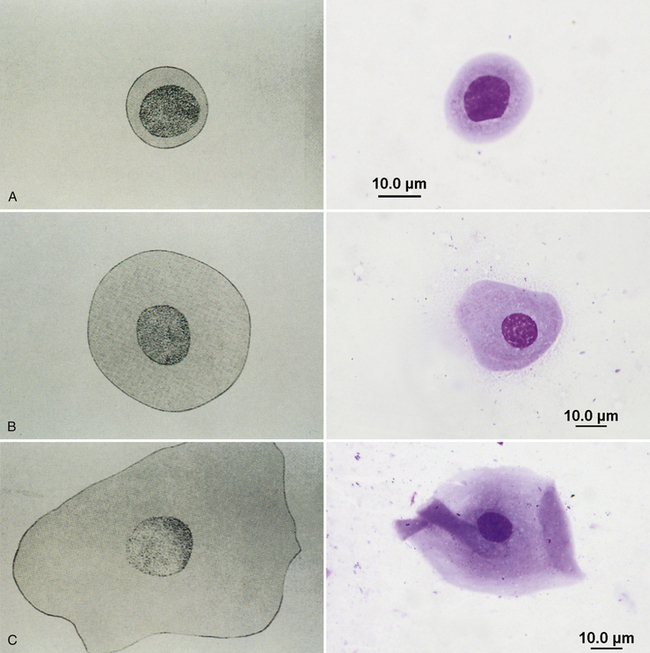
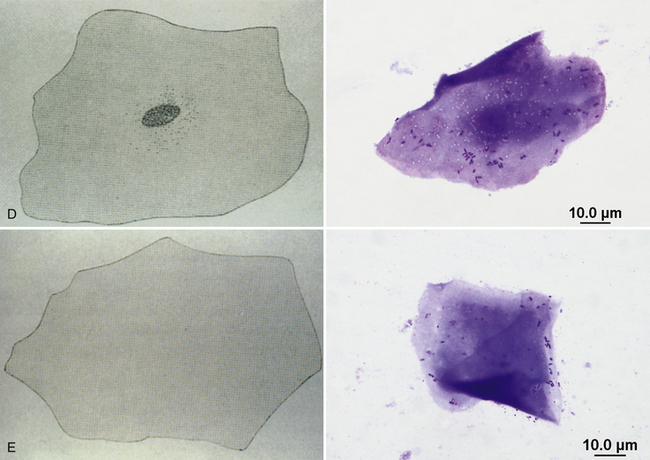
Figure 25-4 Diagrams and corresponding images of epithelial cell types from the canine vagina.
A, Parabasal epithelial cells. B, Small intermediate cells. C, Large intermediate cells. D, Superficial cells with pyknotic nuclei (note bacteria adhered to the cell on the right). E, Anuclear superficial cells. (All cytology images stained with Wright stain. Original magnification 1000×.) (All diagrams courtesy of Kal Kan Forum.)
Parabasal Cells
Parabasal cells are small round cells with round vesiculated nuclei and a small amount of cytoplasm and are usually quite uniform in size and shape (see Figure 25-4, A). Large numbers of parabasal cells may exfoliate when the vagina of a prepubertal animal is swabbed.
Intermediate Cells
Intermediate cells vary in size, depending on the amount of cytoplasm present. Although the nuclei of both small and large intermediate cells are similar in size to parabasal cell nuclei, intermediate cells are about twice the size of parabasal cells (see Figure 25-4, B and C). Intermediate cells still have vesiculated nuclei, but as they increase in size, their cytoplasm becomes irregular, folded, and angular, similar to the cytoplasm of superficial cells. Large intermediate cells are sometimes called superficial intermediate cells or transitional intermediate cells.
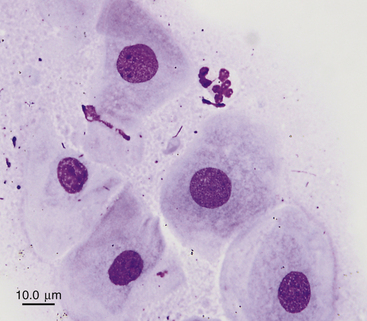
Superficial Cells
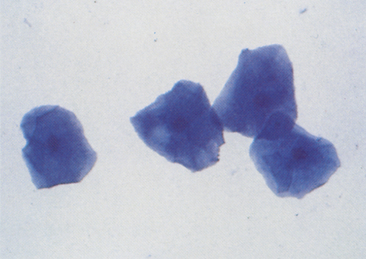
Superficial cells are the largest epithelial cells seen in vaginal smears (see Figure 25-4, D). These are dead cells, whose nuclei become pyknotic and then faded, often progressing to anucleate forms (see Figure 25-4, E). Their cytoplasm is abundant, angular, and folded. As cells degenerate, their cytoplasm may develop small vacuoles (Figure 25-5). The degeneration process of stratified squamous epithelial cells into large, flat, dead cells is called cornification; superficial epithelial cells are commonly called cornified cells. Superficial cells with small pyknotic nuclei and anuclear superficial epithelial cells have the same significance.
Other Normal Cytologic Findings
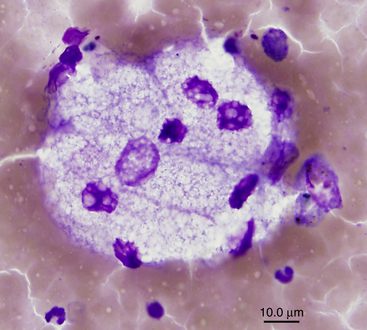
Metestrum cells have been described as vaginal epithelial cells containing neutrophils in their cytoplasm (Figure 25-6).3,6 They are not specific for any stage of the cycle and may be seen whenever neutrophils are present.
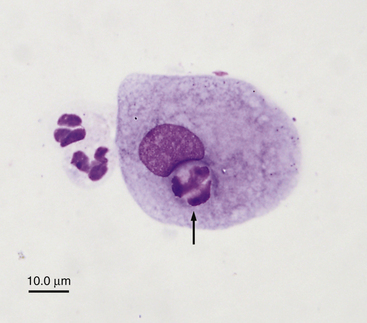
Figure 25-6 Neutrophil (arrow) within the cytoplasm of an epithelial cell.
These cells have been termed metestrum cells but may be seen at any time neutrophils are present. (Wright stain. Original magnification 1000×.)
The vagina of dogs and cats contains normal bacterial flora, and bacteria are frequently observed on vaginal cytology slides.7,8 Unless the bacteria are accompanied by large numbers of neutrophils, they are generally considered normal flora.
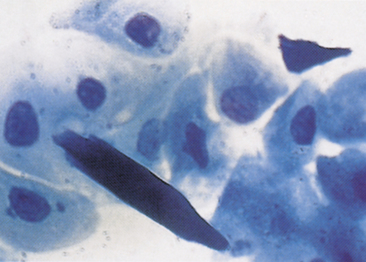
Spermatozoa are sometimes observed in vaginal cytologic preparations from mated bitches (Figure 25-7), but the period during which they are present varies. The presence of spermatozoa confirms a mating, but their absence does not ensure that a bitch was not bred. We have observed intact spermatozoa or sperm heads in about 65% of vaginal smears made 24 hours after a natural mating and in 50% of smears made 48 hours after mating.
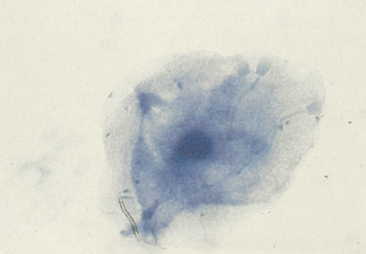
Figure 25-7 Spermatozoa and a superficial epithelial cell in a vaginal smear from a bitch several hours after mating. (Wright stain. Original magnification 400×.)
Cells that appear to be placental trophoblast-like syncytia may be occasionally observed in vaginal cytologic preparations, particularly several weeks after whelping in bitches with suspected subinvolution of placental sites (Figure 25-8).5
Staging the Canine Estrous Cycle
Figure 25-9 provides an overview of the changes in vaginal cytology related to plasma estrogen levels during the normal canine estrous cycle.
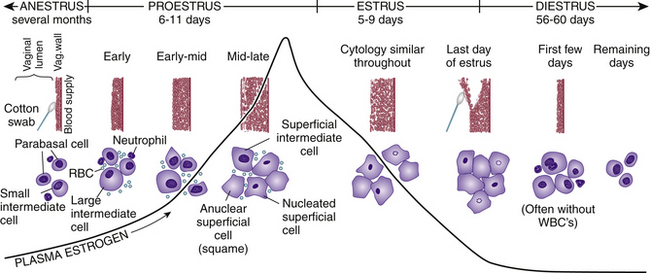
Figure 25-9 Illustration of the changes in vaginal cytology related to plasma estrogen levels: in the average canine estrous cycle. (From Feldman EC, Nelson RW: Ovarian Cycle and Vaginal Cytology. In: Feldman EC, Nelson RW, editors: Canine and feline endocrinology and reproduction, ed 3, Philadelphia, PA, 2004, Saunders, p. 755.)
Proestrus
As ovarian follicles mature and serum concentrations of estrogen (estradiol) increase, the vaginal epithelium proliferates and erythrocytes pass through uterine capillaries. These changes result in the typical appearance of vaginal cytologic preparations made during proestrus (Figure 25-10). Cytologic specimens obtained in early and mid-proestrus are characterized by a mixture of epithelial cells, including parabasal, small and large intermediates, and superficial cells (Figure 25-11), along with variable numbers of neutrophils and erythrocytes. Basophilic mucous material may be present in the background. As proestrus continues and the vaginal epithelium thickens, neutrophils are no longer able to traverse the vaginal wall, so their numbers decrease. Progressively higher percentages of large intermediate and superficial cells are present, with fewer parabasal and small intermediate cells. After serum estrogen levels peak in late proestrus, more than 80% of epithelial cells are superficial, and neutrophils are absent; this is identical to the vaginal cytology during estrus.9 Erythrocytes may be abundant or absent throughout proestrus. Bacteria, both free and on the surface of epithelial cells, are often present in large numbers (see Figure 25-14). The mean duration of proestrus in mature bitches is 9 days, although a range of 2 to 17 days is seen in normal dogs.2
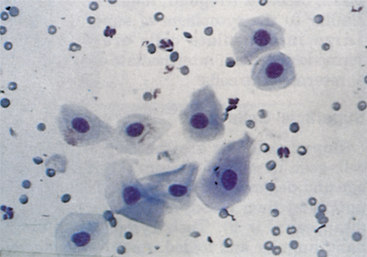
Figure 25-10 Vaginal smear from a dog in proestrus.
Intermediate epithelial cells predominate. Note the erythrocytes and a few neutrophils. (Wright stain. Original magnification 100×.)
Estrus
Most (80% to 90%) of the epithelial cells exfoliated during estrus are superficial cells. Typically, almost all these superficial cells contain small pyknotic nuclei (Figure 25-12). However, samples from some bitches contain nearly 100% anuclear cells; in other bitches, large intermediate cells are retained. Maximal cornification follows the serum estrogen peak in late proestrus and continues throughout estrus.1,9 Ovulation usually occurs about 2 days after the luteinizing hormone (LH) surge, following decreases in serum estrogen and increases in serum progesterone (Figure 25-13).2 Because maximal cornification may occur as much as 6 days before or 3 days after the LH surge, vaginal cytology is an imprecise predictor of ovulation. Cytologic preparations made during estrus usually have a clear background that is free of mucus, and may or may not contain erythrocytes. Large numbers of bacteria are commonly observed on and around superficial epithelial cells, but neutrophils are normally absent unless inflammation is present (Figure 25-14).3 The average duration of estrus is 9 days for mature bitches, but a range of 3 to 21 days has been reported.2
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree