Chapter 12 Urinary Tract Trauma and Uroperitoneum
Introduction
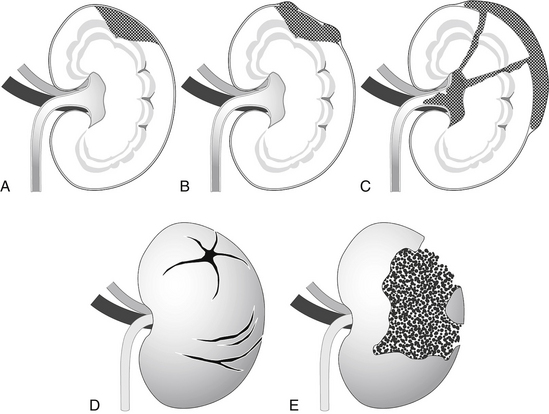
A. Types of trauma to the urinary tract (Figure 12-1)
1. Kidney: Renal trauma is not commonly recognized in dogs or cats, possibly because the kidneys are protected by a fibrous capsule and embedded in perirenal fat. Absorption of shock also is facilitated by the fact that both kidneys are relatively mobile in the dog and cat. Further protection of the kidneys is provided by the ribs, epaxial musculature, and spine.
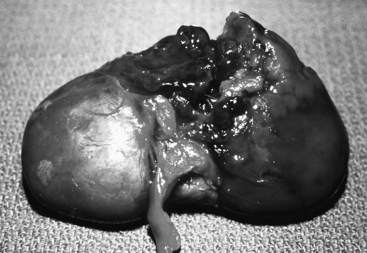
c. Fissure: Renal parenchymal tear that extends through the renal capsule resulting in a perinephric hematoma (Figure 12-2).
d. Rupture: Tear that is extensive enough to allow blood to accumulate in the retroperitoneal space or peritoneal cavity.
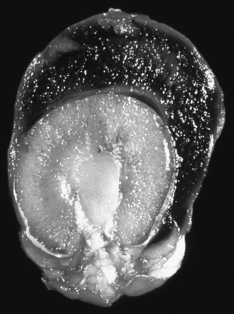
FIGURE 12-2 Perinephric hematoma. Note the degree of retroperitoneal hemorrhage surrounding this kidney.
Pathogenesis and Pathophysiology
Causes of Urinary Tract Trauma
Syndromes Caused by Urinary Tract Trauma or Rupture
3. Urine extravasation into body cavity.
a. Uroperitoneum is the accumulation of urine in the peritoneal or retroperitoneal spaces due to a rupture of the urinary tract anywhere along its course (i.e., kidney, renal pelvis, ureter, urinary bladder, urethra).
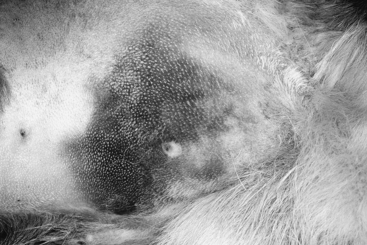
4. Urine extravasation into subcutaneous tissues from a tear in the urethra causes swelling, bruising, and sloughing of tissues.
5. Postrenal azotemia and failure. Azotemia develops as nitrogenous waste products accumulate in the peritoneal cavity and are absorbed across the semipermeable peritoneal membranes. Absorption of waste products also can occur from the subcutaneous tissues when urine accumulates there.
Clinical Signs
E. Increased thirst sometimes is noted as a consequence of fluid shifts that occur as urine accumulates in the peritoneal cavity.
G. As uroperitoneum persists, the signs of uremia including vomiting, lethargy, and dehydration become more apparent.
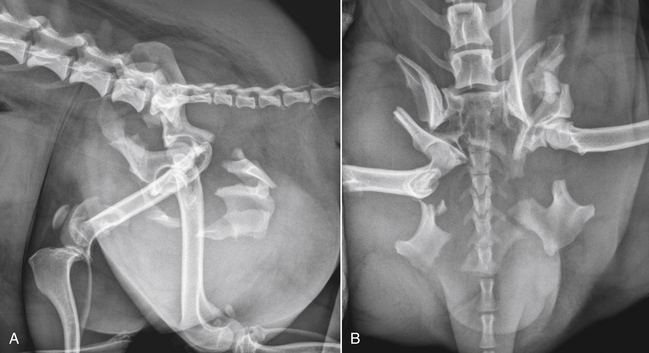
H. Because uroperitoneum frequently is associated with trauma, additional signs often will be present due to other systemic injuries (e.g., musculoskeletal injuries).
Physical Examination
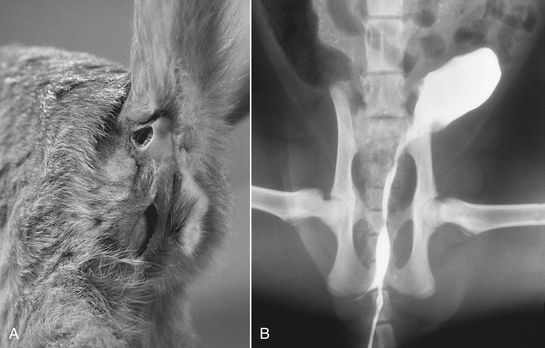
C. Evidence of extensive abdominal injury (e.g., bruising) or fractures (e.g., pelvis, femur) in small animals (Figures 12-4 and 12-5).
D. A small urinary bladder may be palpable in dogs and cats with ruptured bladder.
2. If the tear is in one kidney or ureter, the bladder still may fill adequately from urine formed by the intact kidney.
E. Distal urethral rupture can result in urine accumulation in the soft tissues of the perineum, caudal thighs, and inguinal region (Figure 12-6). Bruising, cellulitis, and sloughing of tissues may be detected after 12 to 36 hours.
Diagnosis of Uroperitoneum
Passage of Urethral Catheter
Abdominocentesis
1. The ratio of the abdominal fluid creatinine concentration to the serum creatinine concentration (both in mg/dL) provides evidence that the suspect abdominal fluid is urine.
2. The concentrations of creatinine and urea in urine entering the peritoneal cavity from a ruptured bladder are very high. Having a higher molecular weight than urea, creatinine does not move across the peritoneal membranes into blood as rapidly as urea, and thus accumulates to a greater degree in the abdominal fluid.
3. The concentration of creatinine in a sample of the abdominal fluid can be compared with the serum creatinine concentration. For example, the concentration of creatinine in the abdominal fluid may be 16.0 mg/dL and serum creatinine concentration may be 4.0 mg/dL. This ratio of 4:1 is definitive evidence that the fluid is urine (a ratio of >2:1 is expected in most cases of ruptured bladder).
4. Simultaneous determination of the abdominal fluid urea nitrogen concentration as compared to blood urea nitrogen (BUN) concentration also can be performed but is not as helpful. Urea has a lower molecular weight than creatinine and equilibrates across the peritoneal membranes more rapidly, resulting in a lower ratio of abdominal fluid urea concentration to BUN concentration. For example, the fluid urea nitrogen concentration may be 90 mg/dL as compared with a BUN concentration of 80 mg/dL (ratio of 1.1).
5. Also due to molecular size differences, phosphate will be retained in the abdominal fluid longer than potassium.
6. In a study of 13 dogs with ruptured bladder, abdominal fluid creatinine concentration was at least four times greater than the upper limit of normal serum creatinine concentration in all cases.
< div class='tao-gold-member'>
a. The median abdominal fluid creatinine concentration to serum creatinine concentration ratio was 4.0 (range, 1.4 to 19.2). A ratio of >2.1 identified 86% of dogs with uroperitoneum. The median abdominal fluid creatinine concentration was 16 mg/dL (range, 7.5 to 22.5 mg/dL) and median serum creatinine concentration was 4.4 mg/dL (range, 0.6 to 11.4 mg/dL).
b. As expected, the largest gradients were seen in animals that had minimal azotemia and the smallest gradients were seen in animals with overt azotemia.
c. The median abdominal fluid potassium concentration to serum potassium concentration ratio was 2.7 (range, 1.4 to 3.3). A ratio of >1.4 predicted uroperitoneum accurately in all of the dogs.
d. Dogs with ascites of other cause had a median abdominal fluid creatinine concentration to serum creatinine concentration ratio of 1.1 and an abdominal fluid potassium concentration to serum potassium concentration ratio of 1.0.
e. Specificity and sensitivity were 100% for the diagnosis of uroperitoneum in dogs when the abdominal fluid creatinine concentration was at least 4 times the upper limit of the laboratory reference range for normal serum creatinine concentration, the abdominal fluid potassium concentration to serum potassium concentration ratio was >1.4, and the abdominal fluid creatinine concentration to serum creatinine concentration ratio was >2.1.
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree