Chapter 57 Tremor Syndromes
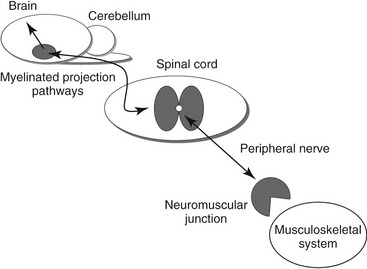
Tremor is a movement disorder characterized as involuntary hyperkinesias of regular repetitive movement oscillations around a joint.1 Tremors can occur at rest or during voluntary movement and typically cease with sleep. Most tremors in animals occur during movement and are associated with diseases of cerebellum and basal nuclei and related pathways, or with a diffuse disease process affecting myelin.2–4 However, lesions that cause tremor can be located in any region within the nervous and musculoskeletal systems (Figure 57-1). Often the cause of tremor in animals is related to an underlying systemic or neurological disease process and can be a hallmark clinical sign to a specific disease process.5 Rarely in cats are tremors a stand-alone clinical entity, which brings forth the importance of performing complete physical and neurological examinations of cats. Tremor disorders in dogs are not uncommon and have been described in past reviews.2,3,6 Tremors in cats have been characterized sporadically with specific disease processes in the veterinary literature. This chapter reviews tremor in cats with respect to classification, pathophysiology, and specific diseases and disorders. Clinical disease presentations for tremor are emphasized, as well as employing a systematic approach when determining an underlying cause of tremor.
CLASSIFICATION OF TREMOR
Tremors are characterized as repetitive, rhythmic, oscillatory, involuntary movements of the entire body or part of the body with regular amplitude and frequency.7,8 Tremors occur as synchronous contractions of agonist and antagonist muscle groups. An important clinical feature of tremor is that the movement ceases during sleep.1 As long as the dominant feature of the movement disorder is rhythmicity, it should be labeled as tremor.7 Electromyography defines tremor as exhibiting biphasic, rhythmic bursts of electrical activity. There are many different classification schemes for tremor. Variables used when classifying tremor include rhythm, amplitude, frequency, anatomical localization, and relation to movement activity. In human beings the gold standard for tremor research still remains through clinical presentations and phenomenology.7,8 Clinical disease entities associated with tremor are further separated based on the condition from which the tremor is elicited, additional findings on neurological examination, medical and family history, and tremor frequency.9 However, tremor classification in animals still remains enigmatic. Tremor in animals is classified according to its anatomical distribution as well as frequency and amplitude during rest, posture maintenance, movement, and performance of specific tasks.2,3,10 A recent article on classification of involuntary contractions in domestic animals categorized tremor as repetitive myoclonus.11
ANATOMICAL
Anatomically, tremors in domestic animals are localized (focal) or generalized.6 A localized tremor in animals can involve the head or one limb or region. Head bob originates from the neck muscles and consists of rapid tremors of the head and neck that are motioned in a horizontal or vertical direction and often are idiopathic in nature in dogs.2 This tremor syndrome may have some similarity to a benign postural tremor in human beings referred to as essential tremor.11 Limb tremors in animals more often are associated with neuromuscular disease weakness. Generalized tremors are caused by systemic disease processes related to degenerative diseases, myelin abnormalities, toxins, encephalitides, electrolyte disturbances, and idiopathic causes.
PHYSIOLOGICAL VERSUS PATHOLOGICAL
Founded on etiology, tremor types in human beings also are categorized as normal (physiological) or abnormal (pathological).8 Physiological tremors occur in all contracting muscle groups and persist throughout the waking and sometimes sleep states. The movement is very fine and barely perceptible. Physiological tremor is elicited by holding the limb outstretched and can be a normal phenomenon. Physiological tremor may be caused by the influence of muscle spindle input, motor neurons, and muscle inertia. It is higher in frequency, in the range of 8 to 13 Hz.8 Physiological tremor can be enhanced by fear or anxiety, drug effects, metabolic disturbances, and epinephrine. Enhanced physiological tremor also is included in the category of essential tremor. Mechanisms include stimulation of beta-adrenergic receptors by increased circulating levels of catecholamines.12,13 Synchronization of motor units is influenced by central and peripheral nervous systems.
Abnormal or pathological tremor is used clinically and often affects specific muscle groups, and is classified based on electromyographic changes. Tremors in animals that are pathological are characterized by impairment of normal motor function.2,6 During activation of a muscle group, the motor unit discharges independently in an attempt to maintain a posture or regulate the movement of a limb or body part. In a pathological state, the motor unit discharges become synchronized, the result being tremor. This rhythmic synchronization determines the tremor amplitude and characteristic electromyographic pattern. Pathological tremor usually is preferential to certain muscle groups and the rate in most forms ranges between 4 and 7 Hz. Pathological tremors can be differentiated from physiological tremors by a greater amount of synchronization, thus greater amplitude and slower frequency.8
Pathological tremors are defined broadly as tremors at rest and during movement (action) (Table 57-1). Resting tremor is an involuntary rhythmic oscillation of part of the body that is not activated voluntarily and is supported against gravity.1 In people, resting tremor usually is a manifestation of Parkinson syndrome and other diseases associated with the basal nuclei. Resting tremor will tend to decrease during voluntary movement. These tremors are low-amplitude oscillations with midrange frequency (3 to 5 Hz). Resting tremor is characterized electromyographically as alternating activity in agonist and antagonist muscles. Resting tremor has not been recognized in domestic animals. Horses with degeneration of the substantia nigra and globus pallidus caused by ingesting the toxin present in yellow star thistle, and the Kerry Blue Terrier and Chinese Crested dog with a neurodegenerative disease that affects the substantia nigra and caudate nuclei, have action-related tremor but not resting tremor.14,15 This type of neurodegeneration has not been reported in cats.
Table 57-1 Terminology for Tremor with Subclassification
| Tremor Type | Definition | Frequency Hz |
|---|---|---|
| REST TREMOR | Tremor in a body part that is not voluntarily activated and completely supported against gravity | 3-5 |
| ACTION TREMOR | Tremor that is produced by voluntary muscle contraction—including postural, isometric, and kinetic | |
| Postural | Tremor that is present while voluntarily maintaining a position against gravity | 5-8 |
| Physiological | Present in normal joints or muscle that can oscillate | Distal joint: >7; Proximal joint: <4 |
| Enhanced physiological | Postural tremor elicited by endogenous or exogenous causes | 8-12 |
| Essential | Postural tremor of hands and head | 4-12 |
| Orthostatic | Postural induced tremor of limbs during standing | >12 |
| Kinetic | Tremor occurring during voluntary movement—including simple, intention and task specific | |
| Unspecified kinetic (simple) | Tremor that occurs during voluntary movements not target directed | 3-10 |
| Isometric | Tremor occurring as a result of muscle contraction against a stationary object | 3-10 |
| Intention | Tremor when amplitude increases during visually guided movements toward target at termination of movement | 2-4 |
| Task specific | Tremor may appear or become exacerbated during specific activities | 3-10 |
Adapted from Deuschl G, Bain P, Brin M: Consensus statement of the Movement Disorder Society on Tremor, Mov Disord 13(Suppl 3):2, 1998.
An action tremor occurs during voluntary contraction of skeletal muscle. Action tremor refers to a tremor that is present when the limbs are actively maintained in certain positions and persists throughout active movement.1 Action tremor is absent when limbs are relaxed and becomes evident when muscles become active. Action tremors often can appear as fine and fast oscillatory movements (5 to 8 Hz). In veterinary patients fine tremor more often is associated with diffuse neuromuscular disease weakness. Action tremor also is characterized by relatively rhythmic bursts of grouped motor neuron discharges that are not quite synchronous.
Action tremor is subclassified according to the activity produced by voluntary muscle contraction: postural, isometric, and kinetic tremor.7 Types of action tremor also have been subdivided as postural tremor and intention tremor.8 Postural-related tremors occur while any part of the body is maintained voluntarily against gravity. Essential tremor is a postural tremor characteristically present during maintenance of a position.16–18 This tremor occurs as an alternating flexion-extension movement. In human beings essential tremor is the most common hyperkinetic movement disorder. Orthostatic tremor is highly dependent on posture especially during standing, causing cramping and uncontrollable shaking in the limbs.19 Diagnostic criterion depends on confirmation of a high-frequency electromyographic recording pattern. The tremor activity will cease once the patient is lifted off the ground. Orthostatic tremor has been well described in dogs, but not recognized in cats.20 Action tremors that are kinetic in nature occur during any voluntary movement. Kinetic tremor is subclassified as intention tremor or nonintention (simple kinetic) tremor.7 Nonintention tremor occurs during any voluntary movement, but is not accentuated during goal-directed movements. Intention tremor is one of the most well-defined types of tremor in our veterinary patients. This type of kinetic action tremor occurs during purposeful voluntary movement,21 becomes apparent during goal-directed movements, and is greatest at the termination of movement.22 Intention tremors exhibit a high amplitude that fluctuates from beat to beat as the target goal is approached and a low frequency (<5 Hz) that is coarse. Afferent or efferent pathways of the cerebellum are the origin of the intention tremor. Some kinetic tremors may become exacerbated during specific activities; this is known as task-specific tremor. Isometric tremor occurs when muscles contract against a stationary object.
PATHOPHYSIOLOGY
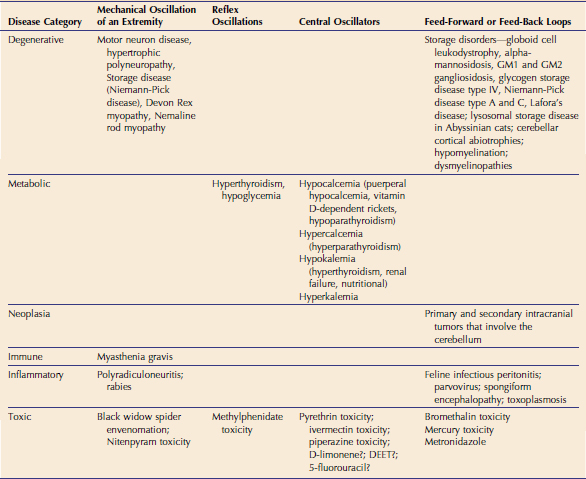
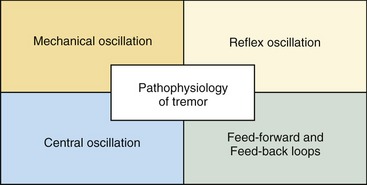
The underlying basis for generation of tremor is spontaneous neuronal or axonal discharges in the central nervous system (CNS) and/or peripheral nervous system.6 This increased excitability in animals often is caused by any disorder that interferes with normal myelination, ion channel function, electrolyte concentrations, and neurotransmission.10 Systems that produce rhythmic activity are called oscillators; such nomenclature has been adapted for human research.9 Oscillatory modes of neuronal behavior occur at all levels of the neuraxis that involve sensorimotor integration, motor timing, muscle coordination, and sympathetic control.23 Pathological tremors are subclassified according to several oscillatory mechanisms that relate to generation of the tremor: mechanical oscillator of an extremity, reflex oscillators, central oscillators, and feed-forward or feed-back loops9 (Table 57-2 and Figure 57-2). Some disease processes may involve a combination of these mechanisms.
MECHANICAL OSCILLATION
Mechanical tremor occurs in the extremity muscles maintained against gravity and depends on the integrity of sensorimotor loops and limb mechanics.21 This can be elicited as the limb is held in extension. The limb will oscillate with a resonance frequency caused by activation of muscle spindles and rhythmic contraction of motor units necessary to maintain limb position. Mechanical oscillators are influenced by cardioballistic (vibration secondary to cardiac activity) oscillations, unsteady postural innervations, and unfused contractions of single motor units. Mechanical oscillation is caused by any disease process that alters the motor unit resulting in weakness and tremors (neuropathic tremor). Neuropathic tremor occurs as an irregular postural and kinetic tremor presumably caused by loss of input from muscle-spindle afferents.24,25 An action tremor of fast frequency can occur with some polyneuropathies. Neuropathy needs to be considered in patients presenting with isolated tremor along with abnormalities in electrophysiological studies.
Pathology of any part of the motor unit may manifest tremors as part of the clinical disease spectrum. Motor neuronopathies are disorders of the ventral horn cells that cause generalized weakness. Motor neuron loss results in progressive weakness with muscle atrophy. A characteristic feature of motor neuron disease that differs from peripheral neuropathy is muscular weakness and fasciculation with muscle atrophy, but preservation of reflexes until the late stage of the disease.26 Tremors are progressive and involve the head musculature predominately.27 Peripheral neuropathies consist of disorders that affect the axon, axonopathies; the Schwann cells or myelin directly, myelinopathies (demyelinating diseases); or both the axons and Schwann cells, mixed axonal and demyelinating diseases. Neuropathic tremor is associated most frequently with demyelinating neuropathies.1 The pathogenesis for generation of tremor is poorly understood. Myelin is essential for normal conduction of the nerve action potential. Axons lacking myelination may discharge spontaneously, associated with presence of high extracellular potassium levels and depolarization.4 Another explanation may be abnormalities in cerebellar Purkinje cells in animals with myelin abnormalities.4 Myelin deficiency most likely is seen as an action tremor and if severe, intention tremor. (Specific polyneuropathies in cats are described in detail in Chapter 50 of the fifth volume in this series.) Some storage diseases with predominant clinical and pathological findings of peripheral neuropathy will manifest tremor.28 (See Chapter 51 in the fourth volume of this series, and Chapter 56 in this volume.)
REFLEX OSCILLATION
Tremors can be generated through reflex activation of oscillators in the CNS.9,21 Any movement in one direction (i.e., flexion) will stretch the extensor muscles and cause a reflex activation of antagonistic muscles. This allows for smooth flexion of a joint so that there is no overshooting of the movement. Tremors can occur when the reflexively activated antagonistic muscle groups become synchronized excessively. This most often is because of situations or disease processes that cause activation of the sympathetic nervous system.12 Tremors associated with mechanism of reflex oscillation are activated by posture movement. Hyperthyroidism can manifest tremor in cats through this mechanism.29 A retrospective study reported 18 per cent of hyperthyroid cats exhibited signs of muscle tremor.30,31 Thyroid hormone and epinephrine can upregulate the sensitivity of muscle spindles and enhance the rhythmic afferent activity leading to greater synchronization and enhanced reflex activity.12 Cats with hyperthyroidism also may have hypocalcemia and hypokalemia that too can accentuate tremor-associated neuromuscular weakness.32,33
Hypoglycemia causes release of norepinephrine to stimulate gluconeogenesis.34,35 The adrenergic response thereby increases synchronization of muscle spindles, resulting in tremor.36 Adrenergic manifestations are evident when the onset of hypoglycemia is rapid. Other adrenergic signs include mydriasis, tachycardia, irritability, vocalization, and nervousness. Methylphenidate is a CNS stimulant used to treat hyperactivity in children, and its mechanism of action is to increase the release and decrease reuptake of norepinephrine and dopamine. Methylphenidate toxicity has been reported to cause tremor in a cat.37 The cat presented with generalized tremor, vocalization, agitation, and hypersensitivity to external stimuli. The cat was treated symptomatically with diazepam and supportive care and clinical signs resolved within 24 hours.
CENTRAL OSCILLATION
Central oscillators have frequencies that are independent of limb mechanics.21 Central oscillators are groups of cells in the CNS that have the capacity to fire repetitively. Two hypotheses have been proposed for mechanisms underlying central oscillations. The first is the rhythmic activity of a group of neurons within a nucleus. The second is that oscillations are generated within loops consisting of neuronal populations and their axonal connections. These connections promote neuronal activity through synapses that promote inhibitory or excitatory influences. Mechanisms that affect membrane conductance can result in tremor by activating central oscillators. Normally neurons fire randomly, but if their membrane conductance is altered so that their activity is synchronized, tremors can result.8
The resting membrane and threshold potential of a neuron is maintained by balances between sodium, potassium, calcium, and chloride.38 Excess or depletion of these electrolytes can alter membrane conductance and influence central oscillators. Hyperchloridemia causes membrane hyperpolarization, lessening the likelihood for generation of an action potential. Hypercalcemia (>14 mg/dL) increases membrane threshold (increases necessary depolarization) resulting in hypoexcitability of the muscle membrane. Hypocalcemia (<7.5 mg/dL) causes membrane hyperexcitability by decreasing the membrane threshold (decreases amount of depolarization necessary for action potential). Hypokalemia (<3 mEq/L) increases the resting membrane potential, making the myofiber refractory to depolarization. Hyperkalemia (>6.5 mEq/L) decreases the resting membrane potential, resulting in hyperexcitability. Neurotransmitters also modulate membrane properties and the interactions among oscillating neurons.21
FEED-FORWARD AND FEED-BACK LOOPS
A fourth mechanism is malfunction of the feed-forward loops within the CNS, especially involving the cerebellum and feed-back information from the periphery.9 The cerebellum is important in modulating control of fine motor activity. Cerebellar dysfunction can produce static and kinetic tremor within the classification of postural and intention tremor, respectively. Normally, rapid limb movements generated toward a goal-directed target are stopped by short burst muscle contractions from antagonist muscle groups.39 If there are delays in loops controlling these actions, goal-directed movements also will be delayed and overshoot in an attempt to compensate.40 These movements result in a coarse tremor generated at the proximal joints known as intention tremor. Cats with cerebellar dysfunction may exhibit this activity during eating or playing. The resting posture of an animal with cerebellar dysfunction may show broad-based stance with the thoracic and pelvic limbs and truncal ataxia. Titubation refers to forward and backward or side-to-side swaying motions (postural tremor) that occur with rostral cerebellar lesion involvement.41 Fine tremors also may occur in the head and neck in animals with pure cerebellar dysfunction.42,43 Tremor of cerebellar origin in cats may be associated with lateral cerebellar zone and vermal lesions.43,44 Cerebellar dysfunction results from a number of primary cerebellar disorders (Box 57-1).
Box 57-1 Primary Cerebellar Disorders in Cats Associated with Tremor
DEGENERATIVE
Lysosomal storage diseases, motor neuronopathy, myelinopathies, cerebellar cortical degeneration
Unconscious proprioceptive feedback also is vital for cerebellar control of motor function. This information is conveyed by rapid conduction of heavily myelinated fibers. Moreover, any process that interferes with these heavily myelinated pathways can result in tremor that is activated by posture and goal-directed movements. During action the tremor at times may be so coarse as to resemble intention tremor of cerebellar disease.4,45 Disorders of the peripheral nervous system that result in myelination may result from congenital, inherited, metabolic, inflammatory, and toxic etiologies.
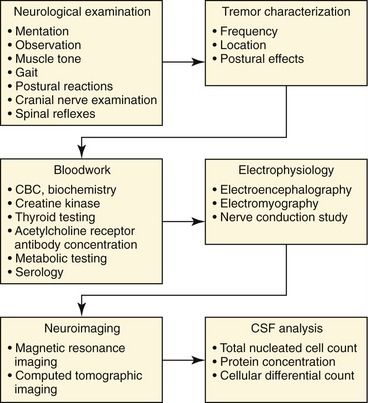
DIAGNOSTIC APPROACH
Diagnosis of the underlying cause of tremor in cats requires thorough patient evaluation and a systematic approach (Figure 57-3).10 Neurological examination will determine presence or absence of neurological disease and possible neuroanatomical localization (see Chapter 49 in the fifth volume of this series). It is important to exclude underlying causes of generalized weakness that may show clinical signs of tremor.46 The patient is evaluated at rest, during maintenance of a static posture during standing and recumbency, and at gait (action). Muscle tone is evaluated at rest and during changes with posture and activity. Muscle tone represents the resistance to passive movement of a joint as seen in spasticity (increased tone in extensor muscles) and rigidity (increased tone in extensor and flexor muscles). Cats with neuromuscular weakness will manifest a plantigrade stance, and in severe weakness the thoracic limbs will be palmigrade. The muscles are visibly observed for any rippling or other spontaneous movements.
The character of the tremor is observed to determine rate and coarseness. Tremor is described according to its frequency: low (<4 Hz), medium (4 to 7 Hz), and high (>7 Hz).7 Regions of the body are described based on localization: head, axial (proximal) musculature, and appendicular (distal) musculature. Fine tremors are high frequency and low amplitude, and are seen commonly with neuropathic tremor and neuromuscular weakness. Coarse tremors are low frequency and high amplitude, and are associated more commonly with intention tremor and cerebellar dysfunction. The tremor also is observed during voluntary movement for evidence of action tremor. With a stethoscope applied to the affected regions, the tremor can be auscultated for pitch and sound.20 Tremors can be observed as the cat is lifted off the ground while relieving muscle contraction.
Results of complete blood count, serum biochemistry (including creatine kinase activity), and urinalysis are useful for screening other metabolic and systemic disease processes.47 Electrolyte disturbances involving sodium, potassium, chloride, and calcium can result in neuromuscular weakness and tremor. Creatine kinase (CK) activity is useful for evaluating for evidence of myopathic disease and muscle damage (Table 57-3). CK activity may be elevated by muscle damage secondary to other underlying problems.47 Elevations in CK may be mild to severe with some tremor disorders depending on the causative source of the myopathy.48 Normal reference range for cats is less than 580 IU/L. Large increases or persistent increases are considered to be of clinical significance. In degenerative conditions the CK may be normal or only mildly elevated. Specific blood tests are used to evaluate for adrenal and thyroid dysfunction. Increased serum thyroxine (T4) concentration will confirm hyperthyroidism. Acetylcholine receptor antibody concentration is a specific test for myasthenia gravis.49 Exercise evaluation for underlying metabolic myopathy is conducted with serum lactate and pyruvate concentrations, but significance with myopathy in cats is unknown. Serology is performed for infectious disease testing.
Table 57-3 Documented Diseases in Cats Associated with Tremor and Elevated Creatine Kinase Activity
| Disease | Severity of Creatine Kinase Elevation |
|---|---|
| DEGENERATIVE | |
| Inherited motor neuron disease | ++ |
| Nemaline rod myopathy | Normal to + |
| Niemann-Pick disease type A and phenotypic variant of type A | + |
| Glycogen storage disease type IV | + to ++ |
| Late-onset cerebellar abiotrophy | ? |
| METABOLIC | |
| Hyperthyroidism | + to ++ |
| Hypoparathyroidism | ++ to +++ |
| Periparturient hypocalcemia | ++ to +++ |
| Hypokalemia | + to +++ |
| IMMUNE | |
| Myasthenia gravis | + to ++ |
| INFECTIOUS | |
| Toxoplasmosis | ? |
| Feline immunodeficiency virus | +++ |
| TOXIC | |
| Black widow spider envenomation | +++ |
| Metronidazole toxicity | +++ |
+, Mild; ++, moderate; +++, severe; ?, elevated enzyme activity but degree not reported.
Electrophysiological techniques are important in characterizing tremor and excluding other movement disorders. Electroencephalography can determine if the movement disorder is associated with a cortical event like seizure. Electrodiagnostic testing (see Chapter 50 in the third volume of this series) also supports disease associated with myopathy or neuropathy. Electromyography and nerve conduction studies assess function of the motor unit.50 Electromyography evaluates muscle for spontaneous electrical discharge activity that can occur with primary myopathic disease or secondary to neuropathic disease. Motor nerve conduction studies evaluate for evidence of axonopathy and/or myelinopathy. Slow nerve conduction velocity occurs in demyelinating neuropathies. Histopathological examination of nerve and muscle is important in determining whether the underlying weakness is neurogenic or myopathic in origin.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree