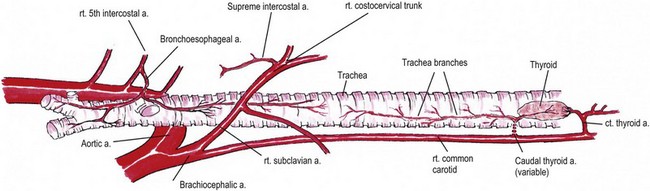
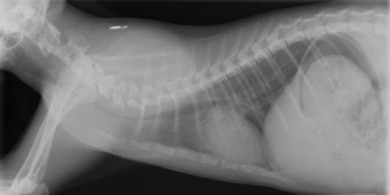
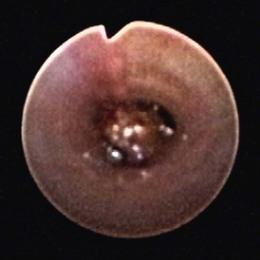
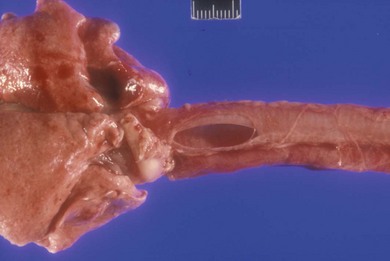
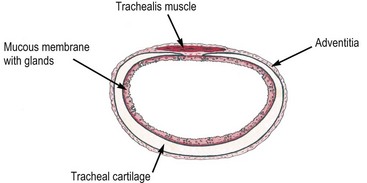
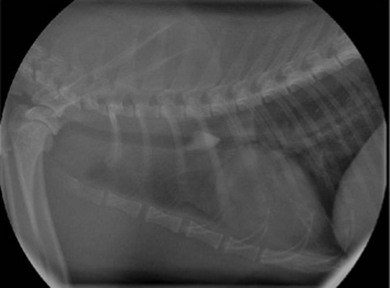
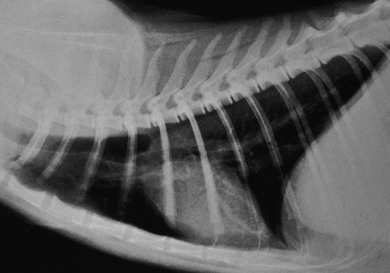
Chapter 46 The trachea extends from the cricoid cartilage to the carina. The normal cat trachea ranges from 7–10 mm in diameter1 and has 38–43 tracheal cartilages.2 These cartilage rings are composed of hyaline cartilage and are incomplete for a short distance dorsally. The dorsal space is filled with loose connective tissue covered by the trachealis muscle, which attaches to the external surface of the tracheal rings.3 Adjacent cartilage rings are joined by fibroelastic annular ligaments, which fuse with the perichondrium. The inner surface of the trachea is covered with respiratory epithelium supported by the submucosa. The tissue at the dorsal aspect of the trachea (muscle, connective tissue, submucosa, and mucosa) is commonly referred to as the dorsal tracheal membrane (Fig. 46-1). Figure 46-1 Cross-section of the feline trachea. The muscle attaches on the outside of the cartilage ring and the ring only has a very narrow defect dorsally. The blood supply to the trachea is segmental, coming from the cranial thyroid, caudal thyroid, and the bronchoesophageal arteries. The vascular pedicles are on the lateral aspects of the trachea. Venous drainage occurs through the thyroid, internal jugular, and bronchoesophageal veins. Sympathetic innervation is from the sympathetic trunk, while parasympathetic innervation is from the recurrent laryngeal nerve.4 The cervical trachea lies dorsal and medial to the sternohyoideus and sternothyroideus muscles. It is ventral to the longus colli and longus capitus muscles. The carotid sheaths are dorsal to the trachea in the cranial half of the neck and lateral to the trachea in the caudal half of the neck. The esophagus is dorsal in the cranial neck and is on the left dorsolateral or left lateral aspect in the caudal neck. The recurrent laryngeal nerves are on the dorsolateral aspects of the trachea. The thyroid and parathyroid glands are on the lateral aspects of the trachea in the cranial neck (Fig. 46-2). As the trachea passes through the thoracic inlet and into the mediastinum, it passes dorsal to the jugular veins, which join to become the cranial vena cava. Within the thorax,5 the aortic arch, left subclavian artery and brachiocephalic trunk lie on the left aspect of the trachea. The right subclavian artery and right vagus nerve are directly lateral to the trachea. The azygos vein crosses the right side of the trachea cranial to the carina. The esophagus moves from the left aspect of the trachea to dorsal as it approaches the carina. The trachea bifurcates into the main stem bronchi between the pulmonary arteries and veins. The main stem bronchi in the cat are short, quickly branching into lower level bronchi. Radiographic signs are dependent on the lesion. If obstruction is present, the foreign body or mass may be observed in the lumen of the trachea (Fig. 46-3). Stenosis or extratracheal compressive masses will cause a narrowing of the tracheal lumen. Tracheal collapse may be difficult to recognize without fluoroscopy, but narrowing of the cervical trachea along the affected segment should be observed on radiographs taken during inspiration (Fig. 46-4). The diameter of the cervical trachea of normal cats is 18–20% of the diameter of the thoracic inlet on lateral radiographs, depending on breed.6 Acute rupture will result in air outside the tracheal lumen. Depending on the location of the rupture, subcutaneous emphysema, air trapping in muscle and fascial planes, pneumomediastinum or pneumothorax may be observed (Fig. 46-5). Figure 46-3 Lateral radiograph of a cat, showing foreign body within the lumen of the trachea. (Image © Michael Tivers, reprinted with kind permission.) Figure 46-5 Lateral radiograph of a cat, showing subcutaneous emphysema and pneumomediastinum due to iatrogenic tracheal rupture. Tracheal foreign bodies reported in cats include grass awns, tree needles, a twig, bark, wood mulch, gravel, small stones, teeth, bones, a bullet, and a safety pin.7 Young cats may be predisposed to this condition in that six of 12 cats in the largest published case series were 18 months or younger.7 The duration of observed clinical signs ranges from one to 21 days. Unless they are very small, e.g., tree needles,8 foreign bodies tend to lodge at or immediately cranial to the tracheal bifurcation, rather than in the bronchi, presumably due to the small diameter of the feline trachea and bronchi. Plain radiographs are usually sufficient for diagnosis. Many objects are radio-opaque and those that are not will be highlighted as a soft tissue density surrounded by tracheal air. Methods used to retrieve foreign bodies include removal using endoscopic guidance,9 removal using fluoroscopic guidance,7 and surgical removal.10 Non-surgical removal is preferred because of the need for a thoracotomy to approach the carina. Endoscopic removal involves visualization of the foreign body using a rigid or flexible endoscope. The foreign body is grasped with forceps or enclosed in a snare. Small objects may be grasped with forceps passed through the biopsy channel of the scope, but larger forceps must be carefully passed alongside the scope. Balloons have been passed beyond the foreign body under endoscopic or fluoroscopic guidance, inflated, and then pulled towards the larynx.11,12 A case series described successful removal of tracheal foreign bodies from ten cats using grasping forceps with a length of 58.7 cm from the tip to the handle.7 The forceps were placed, then the object was grasped and withdrawn, under fluoroscopic guidance. Two of these cases involved repeated unsuccessful attempts to remove the foreign body under endoscopic guidance, followed by successful use of the fluoroscopically guided forceps. The particular forceps used was of a custom design, but long-handled grasping forceps are common in minimally invasive surgery packs. Tracheal masses are less common than laryngeal masses in the cat, but do occur. Neoplasia is most common (Box 46-1). From the literature, the age at time of diagnosis of neoplastic masses ranged from two to 18 years, with all cats, except one with squamous cell carcinoma, being over six years of age, with a median age of 9.5 years.14,29 Affected breeds included domestic short-haired (DSH), domestic long-haired (DLH), Siamese, Himalayan, and Persian cats. Non-neoplastic masses are less common than neoplastic conditions (Box 46-1). Cats with myiasis were one to two years of age, while the other non-neoplastic masses were found in older cats. The masses were observed as focal soft tissue opacities within the trachea, focal annular thickening of the trachea or focal narrowing of the trachea on radiographs. Tracheoscopy allowed direct observation of masses (Fig. 46-6), removal of one of four Cuterebra larvae, and tissue removal for diagnostic purposes and/or debulking of the obstruction. Histology provided definitive diagnosis, but cytology was less reliable, most notably when lymphocytic/plasmacytic inflammation was found. Subsequent histologic examination found neoplasia in some of these instances. Treatment of tumors differed according to tumor type. Treatment of lymphoma/lymphosarcoma with surgical resection/anastomosis, radiation therapy, and/or chemotherapy resulted in disease-free intervals of up to 19 months.13,15,24,25 Resection/anastomosis resulting in complete removal of adenocarcinomas has resulted in long-term survival, while partial removal has resulted in disease-free intervals up to one year.13,18,19,22,25 Tracheal stenting relieved respiratory distress due to tracheal stenosis, but progression of carcinoma within the lung resulted in recurrent respiratory distress in six weeks.27 Definitive treatment of tracheal seromucinous, squamous cell or neuroendocrine carcinoma has not been described. Surgical removal of a Cuterebra larva through a tracheotomy incision resolved disease in three cats, but one cat developed tracheal collapse in the region of the tracheotomy six years later.27,30,31 The cat with mycobacterial infection died of other causes six months after excisional biopsy of the tracheal lesion and a course of appropriate antibiotic therapy.33 Excisional biopsy of the tracheal polyp using the endoscopic biopsy forceps resulted in resolution of clinical signs for four months, after which the cat was lost to follow up.32 Tracheal avulsion is a traumatic lesion, thought to be caused by sudden hyperextension of the neck while the carina remains in a fixed position.35–40 Separation of the tracheal wall usually occurs just cranial to the carina. Depending on the degree of disruption, signs of respiratory distress will be present immediately or will be delayed. In cats with delayed clinical signs, the tissues surrounding the intrathoracic trachea maintain the airway, creating a pseudotrachea, and signs become apparent only when further motion results in sudden disruption of the remaining tissues or stenosis develops at the ends of the pseudotrachea, causing severe air trapping in the lung. Tracheal avulsion typically occurs in young adult cats with a history of known or presumed trauma, with times to presentation being one to 28 days after the traumatic episode. The onset of respiratory distress is often sudden and severe. If the animal is examined at the time of the injury and signs of respiratory distress are not present, radiographic findings associated with tracheal avulsion may easily be missed. These signs include separation of tracheal rings, focal tracheal narrowing, and the presence of air outside the trachea. Radiographic findings in cats exhibiting respiratory distress include obviously separated tracheal rings with an associated gas-filled diverticulum or dilated pseudotrachea (Fig. 46-7), stenosis of the tracheal lumen at the junctions of normal and avulsed tracheal tissue, pneumomediastinum, and over-inflation/hyperlucency of the lung fields associated with air trapping. Figure 46-7 Lateral radiograph of a cat, showing the pseudoairway associated with tracheal avulsion. (Image © Robert White, reprinted with kind permission.) Resolution of clinical signs with conservative therapy has been reported in one cat, but most cats with this condition need resection of the affected segment because the degree of stenosis at the ends of the affected tracheal segment worsens with time. Long-term resolution of clinical signs was documented in 18 of 20 cats treated with immediate repair or resection/anastomosis of the affected tracheal segment and followed for five months to seven years after surgery.37–40 Two cats did not survive the surgical procedure. Iatrogenic injury to the dorsal tracheal membrane may occur in cats undergoing endotracheal tube intubation.1,40–44 The majority of reported injuries are associated with dental procedures and appear to be secondary to endotracheal tube cuff over-inflation. Most ruptures occur at the thoracic inlet, the site at which the endotracheal tube cuff is routinely placed. Both high pressure, low volume cuffs and low pressure, high volume cuffs have been associated with injury. The average volume of air required for endotracheal cuff inflation resulting in an air-tight seal in the normal cat trachea is 1.6 mL. Studies in cat cadavers determined that inflation volumes over 6 mL resulted in tracheal rupture.1 The ruptures were linear tears at the junction of the dorsal tracheal membrane and the tracheal cartilage (Fig. 46-8). The mediastinum remained intact when rupture occurred.
Trachea and bronchus
Surgical anatomy
General considerations and diagnostic procedures
Diagnostic imaging

Surgical diseases
Foreign bodies
Tracheal masses
Tracheal avulsion
Iatrogenic tracheal rupture
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Trachea and bronchus