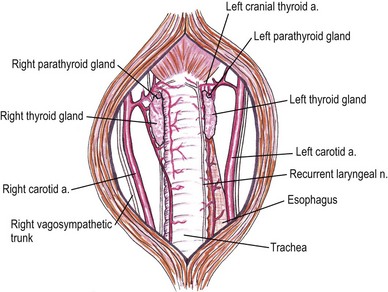
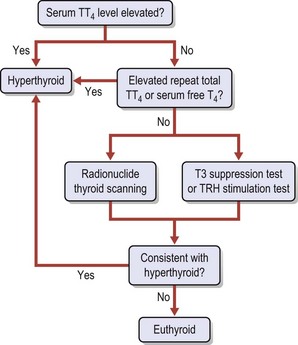
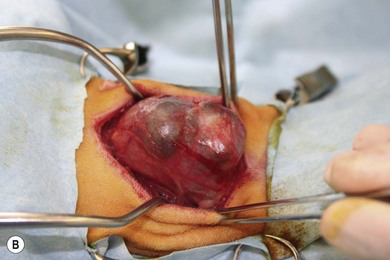
Chapter 53 Diseases of the thyroid and parathyroid glands are the most common indication for surgery in the neck of feline patients. Although they share a common anatomical location, the thyroid and parathyroid glands are functionally very different. The thyroid gland produces thyroxine, an important regulator of metabolic homeostasis. The parathyroid glands are responsible for calcium homeostasis.1 Diseases of these glands can cause profound metabolic changes and surgery can be very rewarding in correctly selected patients. This chapter provides a comprehensive overview of thyroid and parathyroid surgical disease in cats with a particular focus on surgical management of feline hyperthyroidism. The thyroid glands are a paired set of adenomatous glands located in the neck at about the level of the fourth through eighth tracheal rings, lateral but adjacent to the trachea itself (Fig. 53-1). The right thyroid gland is normally located slightly cranial to the left gland. Closely associated with the thyroid glands are the much smaller and pale tan-colored parathyroid glands. Each side contains two parathyroid glands, one located at the cranial pole and outside the thyroid parenchyma (external parathyroid gland) and a second caudal parathyroid gland within the thyroid parenchyma itself (internal parathyroid gland). For this reason, the caudal internal parathyroid glands are more difficult to visualize during surgery. The thyroid glands are encapsulated and ductless. The major blood supply to the thyroid glands is the cranial thyroid artery arising from the common carotid artery on each side. The artery enters the cranial pole and branches off to the parathyroid gland immediately or in some cases after traversing a short distance through the cranial pole of the thyroid gland. A caudal thyroid artery arising from the brachycephalic trunk is present in some but not all cats.2 Venous drainage is through the cranial and caudal thyroid veins into the internal jugular vein. The thyroid glands measure about 16 mm long, 4 mm wide, and 2 mm thick in the adult normal feline patient.3 The parathyroid glands are typically about 1–2 mm in diameter with the cranial external parathyroid glands appearing well demarcated from adjacent thyroid tissue. There may be an isthmus of thyroid tissue connecting the right and left thyroid glands in some feline patients,4 although this is more common in humans. Cats may also have ectopic thyroid tissue that can be located anywhere along the midline cervical area, thoracic inlet, or in some cases the thorax.5 There has also been a report of cystic ectopic thyroid tissue in the tongue.6 Studies have shown that 10–20% of hyperthyroid cats undergoing nuclear scintigraphy have ectopic hyperplastic thyroid tissue.7,8 Failure to identify hyperplastic ectopic thyroid tissue preoperatively can be a cause of persistent hyperthyroidism after surgery. There may also be ectopic parathyroid tissue in up to 50% of cats that can be located in the peritracheal fascia, mediastinum, or pericardium.2,7,9 Physical examination is often rewarding. Palpation of the ventral cervical area of the neck is performed by running two fingers gently down either side of the trachea from the larynx to the manubrium while the neck is extended with the head in slight dorsal extension (Fig. 53-2). The examiner may feel a thyroid ‘slip’ or small mass that passes under the fingers on either side. In some cases, a thyroid slip may only be palpable unilaterally or the thyroid nodule(s) may be close to the thoracic inlet and not palpable.2 A second palpation technique has also been described.10 This is described as a semi-quantitative technique using a scale of 0 to 6. Cats with non-palpable lobes are scored as 0. A score of 1 is assigned to a lobe that is barely palpable and 6 to a lobe approximately 2.5 cm or greater in length. To palpate the right thyroid lobe, the cat’s head is held with the clinician’s left hand, the chin elevated to 45° from the horizontal and the head turned 45° to the left from the vertical. The tip of the right index finger is placed in the groove between the trachea and the right sternohyoideus muscle just below the larynx and run down the groove to the thoracic inlet. An enlarged lobe is typically felt as a ‘pop’. If no lobe is palpated on two runs, the cat’s head is released and repositioned for a third try. If this is also negative, a final try using more finger contact (typically the flat part of the middle finger) is used. Comparison between this newer technique and the classic palpation technique has found good within- and between-examiner agreements for both, although due to familiarity the classic technique may be preferred.11 Wetting the neck fur with water or clipping the area can also be helpful with either technique. Palpation of a nodule in this area is highly suggestive of a thyroid or parathyroid nodule, although there has also been a report of bilateral dermoid cysts presenting as enlarged thyroid glands in a cat.12 Thyroid and parathyroid disease of cats tends to affect middle-aged and older patients. The reported age range is four to 22 years, but 95% of cats with hyperthyroidism are older than 10 years.1 Juvenile hyperthyroidism has also been reported in an eight-month-old cat.13 Clinical signs of hyperthyroidism are often slowly progressive and include weight loss, polyphagia, vomiting, polyuria, polydipsia, increased activity, restlessness, diarrhea, panting, and weakness. Cats may appear in thin body condition with an unkempt coat. Tachycardia, a gallop rhythm, or heart murmur may be appreciated on auscultation. Some cats may present with clinical signs of congestive heart failure as hyperthyroidism can induce a secondary cardiomyopathy (hypertrophic or dilative).1 Respiratory distress, weakness, and cardiac arrhythmias may be present in these patients. Patients with larger cervical masses may have a cough, dysphagia, facial edema, and Horner syndrome. A small subset of cats may present with apathetic hyperthyroidism where the clinical signs are depression, anorexia, and weakness. This is reported in less than 5% of cases1 and is not typical. Parathyroid disease in cats is much less common, but affected animals may present with clinical signs consistent with hypercalcemia. This is primarily polyuria and polydipsia, although lethargy, inappetence, vomiting, and weakness may also be observed. Cardiac changes are much less likely, although renal disease may be present in patients with chronic hypercalcemia.1 Common abnormalities noted in cats with hyperthyroidism are mild erythrocytosis, high mean corpuscular volume, leukocytosis, lymphopenia, and eosinopenia. These changes are consistent with a stress response as a result of increased thyroid hormone levels. Blood biochemistry result may reveal elevated alanine aminotransferase (ALT), alkaline phosphatise (ALP), bilirubin, and lactate dehydrogenase (LDH). Interestingly, high serum liver enzyme levels do not seem to be associated with abnormalities in hepatic parenchyma and liver function, regardless of degree of increase. Serum liver enzyme activities were shown to return to normal after control of hyperthyroidism with 131I therapy in one study.14 Cats may also have renal dysfunction that is partially masked by the elevation of the renal glomerular filtration rate by hyperthyroidism. Azotemia, hyperphosphatemia, and hypokalemia may also be seen.1,7 Confirmation of hyperthyroidism is obtained by performing blood thyroid function tests (Fig. 53-3). High serum total thyroid hormone levels confirm hyperthyroidism. Measurement of resting total T4 (TT4) levels is preferred over T3 levels. In cases where clinical signs are highly suggestive of hyperthyroidism but the TT4 level is not elevated above normal, repeat total T4 and free T4 (fT4) concentrations should be measured one to two weeks after the initial test. Serum fT4 concentrations are more reliable than TT4 in part because non-thyroidal illness has more of a suppressive effect on serum TT4 than fT4. Serum fT4 is increased in many cats with occult hyperthyroidism and ‘normal’ TT4 test results. If these tests are equivocal, radionuclide thyroid scanning is advised. The T3 suppression test and thyroid releasing hormone stimulation test are also occasionally used in cats where TT4 and fT4 serum measurements are equivocal.15 A recent study demonstrated a significantly higher risk of euthyroid geriatric cats becoming hyperthyroid if they had thyroid stimulating hormone (TSH) below the reference range. Cats that became hyperthyroid within 14 months also had higher ALP levels and higher prevalence of goiter than controls.16 An elevated ionized calcium level is the most common biochemical abnormality noted on cats with primary hyperparathyroidism. Isosthenuria may be seen on urinalysis. Azotemia may be occasionally noted. It is essential to rule out other causes of hypercalcemia, especially hypercalcemia of malignant disease. Thoracic and abdominal radiographs along with ultrasound of the abdomen and neck are essential. Parathyroid hormone or parathyroid hormone-related protein serum level tests of the radionuclide can also be utilized.17 Thyrotoxic cardiomyopathy may develop in cats with hyperthyroidism. This may either be hypertrophic or, less commonly, dilative cardiomyopathy. Tachycardia, pulse deficits, pounding heartbeat, a gallop rhythm, cardiac murmur, or muffled cardiac sounds secondary to pleural effusion may be noted on physical examination. Electrocardiographic abnormalities may also be noted, including arrhythmias, increased R-wave in lead II, and widened QRS complexes.15 Thoracic radiographs may reveal pleural effusion, cardiomegaly, or pulmonary edema. Echocardiogram may reveal thickening (hypertrophic) or dilation (dilative) changes to the atria, ventricles, and septum with decreased myocardial contractility. Hypertrophic thyrotoxic cardiomyopathy may be reversible once the cat is euthyroid, but dilative thyrotoxic cardiomyopathy is not. Systemic hypertension is also common in cats with hyperthyroidism, but is commonly clinically silent. The hypertension results from the effects of increased β-adrenergic activity on heart rate, contractility, vasodilation, and activation of the renin–angiotensin–aldosterone system.15 If hypertension does not resolve with treatment using anti-thyroid drugs, treatment with the calcium blocker amlodipine (0.13–0.3 mg/kg once daily) is recommended before surgery. Imaging can be very useful in the evaluation of patients with thyroid and parathyroid disease. The two primary modalities used are ultrasound and nuclear scintigraphy. Plain thoracic and abdominal radiographs are also helpful in the further evaluation of patients with hypercalcemia or those suspected of having malignant disease, to rule out metastatic disease or mediastinal masses.18 Ultrasound imaging of the thyroid and parathyroid glands requires high frequency transducers in the 7.5–10 MHz range.19 Transducers in this range allow resolution of smaller structures with better anatomical detail. In particular, this allows visualization of parathyroid adenomas that tend to be unilateral and can therefore help the surgeon plan the procedure. Ultrasound is also useful in evaluating unilateral versus bilateral thyroid disease, as well as the extent of any localized invasion that may be a result of thyroid or parathyroid adenocarcinoma.20 Ultrasound of the thoracic inlet may also be helpful in localizing ectopic thyroid tissue. Thorough preoperative evaluation of patients will also often require echocardiography to evaluate underlying cardiac disease and ultrasonography of the urinary system to evaluate the kidneys and bladder. This can be performed with lower frequency transducers. Hyperthyroid cats will have an increased uptake in the abnormal thyroid gland(s). Unilateral disease can be differentiated from bilateral disease and ectopic thyroid tissue can also be identified. Nuclear scintigraphy is not able to reliably distinguish between thyroid adenocarcinoma and adenoma.8 A comprehensive overview of nuclear scintigraphy is included in Chapter 8. The most common indication for surgery of the feline thyroid glands is removal of benign functional neoplastic thyroid tissue. Surgery to excise thyroid carcinoma is also performed, although carcinomas occur in only about 2–3% of patients with hyperthyroidism.7,21 A thyroid cyst and thyroid cyst adenomas have also been reported in cats.22 These cystic masses should be considered as differential diagnoses but are still relatively uncommon (Fig. 53-4). Surgical procedures to remove thyroid masses are usually elective and patients will often be higher risk anesthesia patients that benefit from preoperative stabilization and a thorough preoperative workup. Figure 53-4 (A) An eight-year-old female neutered domestic short-hair cat with massive goiter. (B) Dysphagia was associated with a space occupying unilateral non-functional thyroid cyst which on histopathologic analysis was reported to be a cystic thyroid adenoma. (Courtesy of Jon Hall.) Hyperthyroidism is a condition resulting from excessive thyroid hormone levels produced by functional adenomatous or hyperplastic thyroid tissue. It is the most common endocrine disorder of cats.21 The disease is bilateral in 70–90% of cats, resulting in enlargement of the thyroid glands on both sides.1,7,23 Treatment options for cats with hyperthyroidism include the use of radioactive iodine, surgical thyroidectomy, and oral medication with methimazole and carbimazole. Selection of the appropriate treatment will depend on a variety of factors including age, concurrent diseases, availability of treatment options, and owner input.24 Surgical thyroidectomy may not be the best option in all cats. Some cats may benefit from a more holistic treatment that balances the hyperthyroidism with treatment of concurrent underlying diseases such as renal failure and hyperaldosteronism. Where available, radioactive iodine (131I) is the treatment of choice for most cases of feline hyperthyroidism. Anesthesia is not required and a single dose of radioactive iodine will result in normal thyroid function in 95% of cats.25 As the radioactive iodine is concentrated almost exclusively in hyperfunctional adenomatous hyperthyroid tissue, normal tissue and the parathyroid glands receive only a small radiation dose.7,21,25 In addition, ectopic hyperplastic thyroid tissue is also treated regardless of the anatomic location. High-dose radioactive iodine therapy has also been used for the treatment of thyroid carcinomas.26,27 A comprehensive overview of radioactive iodine therapy for feline hyperthyroidism is included in Chapter 8. The main limitations of radioactive iodine therapy are the availability of treatment facilities and costs. Medical treatment of hyperthyroidism typically consists of oral medication with methimazole or carbimazole which block the synthesis of thyroid hormone.28 Carbimazole is converted to methimazole after administration.29 Side effects of methimazole include gastrointestinal upset, facial excoriation, neutropenia, and hepatic enzyme elevations.30 Serious side effects such as agranulocytosis and thrombocytopenia have also been reported with methimazole but not carbimazole and therefore carbimazole is preferred when available.1 Restoration of euthyroidism will lead to a drop in glomerular filtration rate of the kidneys. Treating azotemic hyperthyroid cats with an anti-thyroid drug until it can be determined whether correction of the hyperthyroid state will exacerbate the azotemia may be prudent.31 Medical management is an important part of preparing a cat for definitive treatment with radioactive iodine or surgical thyroidectomy and can also be used for long-term treatment. However, one study reported a significantly lower survival time for cats treated with methimazole alone versus those treated with 131I alone or methimazole followed by 131I.32 The main limitation of medical treatment is inability of the owner to orally dose the cat, although alternate options for medication delivery like transdermal patches have been developed.33 A recent prescription diet for hyperthyroid cats has also been made available (Hill’s Prescription Diet y/d, Hill’s Pet Nutrition, Topeka, KS). The goal of the diet is to decrease thyroid hormone production by limiting iodine uptake without the use of additional anti-thyroid drugs. The diet also contains taurine and carnitine for cardiac health and lower phosphorous and sodium levels to support renal function. Other treatments, including percutaneous ultrasound-guided radiofrequency heat ablation, have been tried and have been shown to be effective transiently but not permanently.34
Thyroid and parathyroid
Surgical anatomy
General considerations
Signalment and clinical signs
Biochemical and hematologic investigations
Concurrent diseases
Diagnostic imaging
Ultrasound
Nuclear scintigraphy
Surgical diseases of the thyroid glands

Hyperthyroidism
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Veterian Key
Fastest Veterinary Medicine Insight Engine