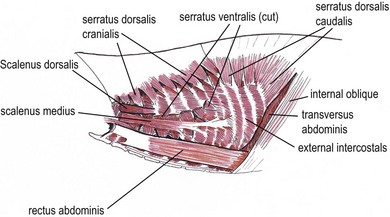
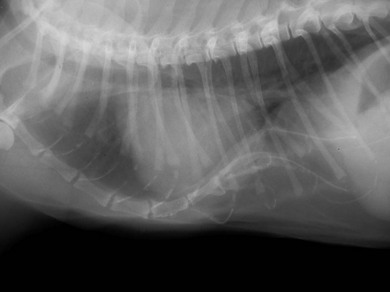
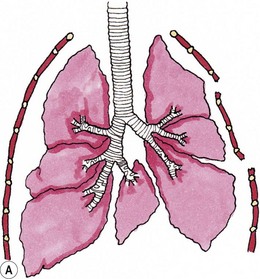
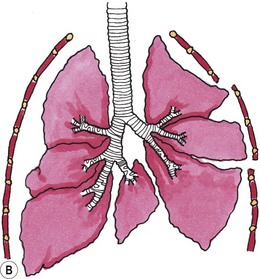
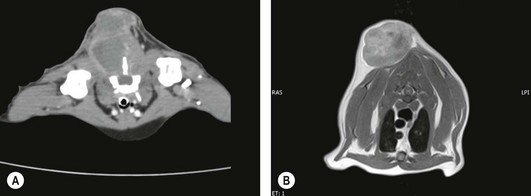
Chapter 43 The bony structure of the feline thorax consists of 13 thoracic vertebrae, 13 pairs of ribs, and nine sternebrae. The first nine ribs articulate with the sternum and are called sternal ribs; the last four are called asternal ribs. Each rib articulates with the corresponding vertebra at the synovial costovertebral joints. The distal part of the rib continues as the costal cartilage to connect with the sternum. The costal cartilages of the 10th, 11th and 12th ribs unite to form the costal arch. The cartilages of the last pair of ribs end freely; these ribs are often termed ‘floating ribs’. The sternum consists of eight sternebrae beginning cranially with the manubrium and ending caudally with the xiphoid cartilage of the xiphoid process. The intercostal space is filled with the internal and external intercostal muscles1 (Fig. 43-1). The latissimus dorsi is a triangular muscle that originates at the spinous processes of the last thoracic and first lumbar vertebrae, extending in a cranioventral direction to insert on the humerus. When the muscle contracts the thoracic limb is retracted caudally, but excision or incision of the muscle does not seem to cause lameness. This muscle is important for reconstructive surgery of the thoracic wall. The serratus ventralis muscle extends from the caudal margin of the first eight ribs to the medial surface of the scapula. The serratus dorsalis muscle is divided into two parts. The serratus dorsalis cranialis arises via a broad aponeurosis from the superficial leaf of the thoracolumbar fascia and inserts with serrations on the cranial borders and the lateral surfaces of ribs 2 to 10. The serratus dorsalis caudalis arises by a broad aponeurosis from the thoracolumbar fascia and extends cranioventrally to the caudal border of the 11th, 12th, 13th, and occasionally, the 10th rib. The scalenus muscle originates at the 4th and 5th cervical vertebra to insert at the 5th rib and forms a surgical landmark for thoracotomy (see Fig. 43-1). The superficial pectoral muscles originate at the cranial end of the sternum and insert at the greater tubercle of the humerus. The pectoralis profundus is a broad muscle extending between the sternum and the minor tubercle of the humerus. The internal thoracic artery originates from the left and right subclavian artery and passes under the transverse thoracic muscle to run caudally to form the cranial epigastric artery. The intercostal arteries and veins originate from the aorta and azygos vein; they then course ventrally along the caudal border of the rib to anastomose with the internal thoracic artery and vein. The intercostal nerves arise from the ventral branches of the thoracic nerves that run with the intercostal arteries and veins. Collateral branches of the main intercostal vessels and nerves can be found on the cranial border of the rib.2 Thoracic trauma patients should be evaluated for breathing difficulties and treated for shock. A significant pneumothorax or a pleural effusion that is causing respiratory compromise should be drained (see Chapter 41, Box 41-2) prior to taking radiographs. An intravenous catheter should be placed for administration of fluids. Administering fluids at shock rates must be balanced against the potential to cause further respiratory compromise if fluid overload occurs with the potential for pulmonary edema. Pulmonary contusions have been reported in up to 50% of animals with thoracic trauma and are a potential indication for limited fluid volume resuscitation (see Chapter 1). Acute traumatic and neoplastic thoracic wall conditions are usually painful; analgesic drugs should be administered. In trauma patients, a total body radiograph can be obtained to gain a preliminary overview of the injuries. Different studies show widely varying rates of thoracic injuries in the feline trauma patient of 11–90%.3 Stress, multiple injuries, and the critical nature of the patient often only allow single view radiographs to be taken initially. The safest view to do first is the dorsoventral view as this avoids the patient having to lie on its side and the potential for compromise to lung expansion that this would cause. The orthogonal view can be done at a later stage when the animal is stable and sedated or anesthetized. To evaluate for metastases or primary neoplasia, a right and left-sided laterolateral view and a dorsoventral view are recommended. Computed tomography (CT) is useful for evaluating intrathoracic disease processes and for preoperative planning for reconstructive surgery involving the thoracic wall. Tumor margins can be highlighted with contrast media and pre- or postoperative radiation therapies can be planned. Magnetic resonance imaging (MRI) is useful for investigating soft tissues and is used in human medicine for preoperative planning and margin evaluation of intrathoracic and thoracic wall tumors. Movement of the chest during this test may cause the pictures to blur. By inducing a transient apnea the anesthetist can prevent this artifact. Ultrasound may be useful to evaluate the characteristics of a thoracic wall mass and to take ultrasound-guided biopsies. Tru-Cut biopsies, punch biopsies and trephine biopsies of the bone often require sedation or general anesthesia; if necessary, these can be performed under CT guidance.4 Facilities for intubation and an anesthetist familiar with intermittent positive pressure ventilation of patients should be available (see Chapter 2). Most anesthetics reduce the respiration capacity and this should be taken into consideration for patients with pneumothorax, pulmonary edema, pulmonary contusion, pleural effusion, and pneumonia, with appropriate management before anesthesia. Thoracic surgery is painful and therefore analgesia, preferably used in a multimodal approach, should be provided pre-, intra- and postoperatively not only to reduce pain but also to minimize the overall dose requirement for anesthetics intraoperatively and to obtain optimal ventilation of the lung. Pain can be minimized by an atraumatic surgical approach, retraction rather than incision of the latissimus dorsi muscle and careful placement of the sutures used to secure the ribs or sternebrae in apposition. Multimodal analgesic techniques such as local, epidural or interpleural nerve blocks or infusions should also be considered in the preoperative plan (see Chapters 2 and 41). Surgical diseases of the thoracic wall include congenital conditions such as pectus excavatum, traumatic lesions such as flail chest, penetrating bite wounds, and neoplasia. Many injuries or diseases will require surgical intervention and a concurrent thoracotomy may be inevitable. For further information on thoracotomy see Chapter 41. The etiology is poorly understood. Shortening of the central tendon of the diaphragm, abnormal intrauterine pressure, thickening of the substernal ligament or of the musculature of the cranial portion of the diaphragm, failure of osteogenesis or chondrogenesis, arrested sternal development, and rachitic influences have all been implicated. Multiple animals in some litters have been affected, so breeding from affected or related animals is not recommended.5 The diagnosis of pectus excavatum can be established by palpation of the thorax and by thoracic radiographs. The deformity can be assessed objectively by measuring the frontosagittal and vertebral indices on thoracic radiographs and by assessment of the minimum thoracic height. Several thoracic measurements need to be taken which are then used to calculate the frontosagittal index and the vertebral index and the minimal thoracic height (Box 43-1, Fig. 43-2). These values characterize the severity of pectus excavatum in cats (Table 43-1). The deviation of the sternum can cause rotation and displacement of the heart as well as compression of blood vessels and lung lobes. Cats with high values are more likely to have impaired ventilation or ECG changes. Table 43-1 Indices used to characterize pectus excavatum in cats Figure 43-2 Pectus excavatum in a three-year-old cat. Note the narrow distance between the xiphoid and the caudal thoracic vertebrae leading to compression of the thoracic organs. Concurrent congenital defects are possible and have to be ruled out before surgery. The need for surgical intervention (see Box 43-2), or the ability to treat the condition conservatively is dependent on the severity and presence of clinical signs. Surgical treatment of a moderate pectus excavatum depends on the clinical findings; a severe pectus excavatum is likely to require surgical treatment if the condition of the patient allows it. Mild pectus excavatum is often an incidental finding with no clinical relevance. Dog bite injuries are the most common causes of flail chest in cats, followed by blunt trauma. A flail chest results from a segmental fracture and/or dislocation of two or more adjacent ribs. The section of unstable ribs moves paradoxically during respiration. During inspiration the flail segment collapses inward; during expiration it moves outward. Air is shunted from the lung under the flail segment to the opposite hemithorax (Fig. 43-3). Figure 43-3 Schematic drawings showing the air movement with flail chest. (A) During inspiration the negative pressure causes movement of the flail segment into the thorax. (B) During expiration air from the unaffected hemithorax pushes the flail segment outward. Stabilization of the patient is the main priority, and this involves securing a patent airway, assessing for adequate ventilation, and establishing oxygenation. If pulse oximetry shows an oxygen saturation of less than 92% at a FiO2 of 21%, supplemental oxygen is needed by face mask, oxygen cage, or a nasopharyngeal or nasotracheal oxygen tube could be inserted. Endotracheal intubation may be necessary if the saturation cannot be kept above 92%.7 Electrocardiography (ECG) may identify cardiac dysrhythmias although they may not be present until 12 to 48 hours after injury. Pain management should be initiated at this time. If possible, the patient should be placed in lateral recumbency; to inhibit paradoxical movement the flail segment should be down. Reduced volume resuscitation (see Chapter 1) is implemented to avoid pulmonary edema.8 The prognosis for a cat with flail chest depends on the severity of concomitant lung injuries. In mild cases the prognosis is favorable, whereas in severe cases with established clinical signs it is guarded. Prognosis worsens with cardiac dysrhythmias, the need for mechanical ventilation, and concurrent injuries. In a clinical study, the outcomes of 24 cases of flail chests were compared (21 dogs and three cats): nine flail chests were surgically stabilized and 15 were not stabilized. There was no significant difference in hospitalization time or outcome.9 Types of crushing injuries include perforating and non-perforating bite wounds and other incidents where a compressive injury occurs to the thorax, e.g., an object falling on to the cat. Dog bite wounds involving the chest wall are the most common crush injury to the feline thoracic wall. Most cats sustain severe damage to the chest wall, with devitalized muscle tissue, fractured ribs and sternebrae, pneumothorax, and internal organ damage. The degree of skin damage may be misleading; major internal organ injury may be present despite the patient only presenting with minor skin wounds or skin bruising. After a crush injury, devitalized tissues and serum accumulation provide a good medium for growing inoculated bacteria. Puncture bite wounds by cats do not cause crushing injuries but they enclose bacteria in the tissue where abscesses can form. These may extend into the thorax causing pyothorax (see Chapter 44). A thorough clinical examination that also rules out further injury sites is recommended. Twenty five percent of bite wounds involve multiple parts of the body.10 Radiography, CT, and ultrasound are currently the most useful diagnostic imaging modalities. In cases of thoracic wall injury, it is advisable to check for rib fractures, lung contusions, spinal injuries, pneumothorax, and hemothorax. Open and closed pneumothoraces should be differentiated. Cats with thoracic wall tumors are usually presented with a recently recognized acute or chronic visible swelling at the affected site. Three-view radiographs can lead to a presumptive diagnosis of thoracic wall tumor, especially in cases with a soft tissue mass, osteolysis or osteoproliferation, and can be useful for exclusion of metastasis. Additional diagnostics valuable for presurgical planning include contrast CT, MRI or scintigraphy.11 These advanced imaging modalities can be used to evaluate the invasiveness of the tumor (Fig. 43-4) and to assess for metastasis. Figure 43-4 Advanced imaging is helpful in presurgical planning and to estimate the extent and depth of the tumor. (A) Contrast enhanced computed tomographic image of a fibrosarcoma in the cat. (B) A magnetic resonance imaging scan of a cat with a thoracic wall fibrosarcoma. (B, Courtesy of the University of Cambridge.)
Thoracic wall
Surgical anatomy
Bony skeleton
Musculature
Vasculature
General considerations
Preoperative evaluation and stabilization of trauma patients
Diagnostic imaging
Anesthesia and analgesia
Surgical diseases
Pectus excavatum
Frontosagittal index
Vertebral index
Normal
0.7–1.3
12.6–18.8
Mild PE
2.0
>9.0
Moderate PE
2.0–3.0
6.0–9.0
Severe PE
>3.0
<6.0
Flail chest
Crushing injuries and bite wounds
Neoplasia
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Thoracic wall